Abstract
Objective
Idiopathic nephrotic syndrome (INS) is the most common glomerular disease in children. Toll-like receptors (TLRs) have been reported to be associated with response to steroid treatment in children with INS. Nevertheless, the correlation between TLR genes and the progression of INS has not yet been clarified. The present study aimed to investigate the association of single-nucleotide polymorphisms (SNPs) in TLR2, TLR4, and TLR9 with susceptibility to INS as well as the clinical phenotyping of steroid responsiveness in Chinese children with INS.
Methods
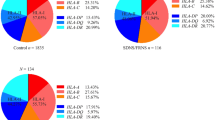
A total of 183 pediatric inpatients with INS were included and given standard steroid therapy. Based on their clinical response to steroids, the patients were classified into three groups: steroid-sensitive nephrotic syndrome (SSNS), steroid-dependent nephrotic syndrome (SDNS), and steroid-resistant nephrotic syndrome (SRNS). A total of 100 healthy children were employed as controls. The blood genome DNA was extracted from each participant. Six SNPs (rs11536889, rs1927914, rs7869402, rs11536891, rs352140, and rs3804099) in TLR2, TLR4, and TLR9 were selected and detected by multiplex polymerase chain reaction with next-generation sequencing to assess TLR gene polymorphisms.
Results
Among the 183 patients with INS, 89 (48.6%) had SSNS, 73 (39.9%) had SDNS, and 21 (11.5%) had SRNS. No significant difference was found in the genotype distribution between healthy children and patients with INS. However, the genotype and allele frequencies of TLR4 rs7869402 were significantly different between SRNS and SSNS. Compared with patients with the C allele and CC genotype, patients with the T allele and CT genotype had an increased risk of SRNS.
Conclusion
TLR4 rs7869402 affected the steroid response in Chinese children with INS. It might be a predictor for the early detection of SRNS in this population.
Similar content being viewed by others
References
Noone DG, Iijima K, Parekh R. Idiopathic nephrotic syndrome in children. Lancet, 2018,392(10141):61–74
Chen J, Qiao XH, Mao JH. Immunopathogenesis of idiopathic nephrotic syndrome in children: two sides of the coin. World J Pediatr, 2021,17(2):115–122
Iijima K, Sako M, Nozu K. Rituximab for nephrotic syndrome in children. Clin Exp Nephrol, 2017,21(2):193–202
Tullus K, Webb H, Bagga A. Management of steroid-resistant nephrotic syndrome in children and adolescents. Lancet Child Adolesc Health, 2018,2(12):880–890
Sameer AS, Nissar S. Toll-Like Receptors (TLRs): Structure, Functions, Signaling, and Role of Their Polymorphisms in Colorectal Cancer Susceptibility. Biomed Res Int, 2021,2021:1157023
Bergallo M, Loiacono E, Gambarino S, et al. Toll-like receptors are essential for the control of endogenous retrovirus expression in Idiopathic Nephrotic Syndrome. Minerva Urol Nefrol, 2017,69(2):201–208
Mishra OP, Kumar R, Narayan G, et al. Toll-like receptor 3 (TLR-3), TLR-4 and CD80 expression in peripheral blood mononuclear cells and urinary CD80 levels in children with idiopathic nephrotic syndrome. Pediatr Nephrol, 2017,32(8):1355–1361
Gbadegesin RA, Adeyemo A, Webb NJ, et al. HLA-DQA1 and PLCG2 Are Candidate Risk Loci for Childhood-Onset Steroid-Sensitive Nephrotic Syndrome. J Am Soc Nephrol, 2015,26(7):1701–1710
Hinkes BG, Mucha B, Vlangos CN, et al. Nephrotic syndrome in the first year of life: two thirds of cases are caused by mutations in 4 genes (NPHS1, NPHS2, WT1, and LAMB2). Pediatrics, 2007,119(4):e907–e919
Fei S, Gui Z, Feng D, et al. Association Between a TLR2 Gene Polymorphism (rs3804099) and Proteinuria in Kidney Transplantation Recipients. Front Genet, 2021,12:798001
Abdolvahabi R, Sarrafnejad A, Nafar M, et al. Association Between TLR2, TLR4, and CD14 Gene Polymorphisms and Acute Rejection in Kidney Transplant. Exp Clin Transplant, 2018,16(1):31–37
Elloumi N, Fakhfakh R, Abida O, et al. Relevant genetic polymorphisms and kidney expression of Toll-like receptor (TLR)-5 and TLR-9 in lupus nephritis. Clin Exp Immunol, 2017,190(3):328–339
Subspecialty Group of Renal Diseases, the Society of Pediatrics, Chinese Medical Association. Evidence-based guideline on diagnosis and treatment of steroid-sensitive, relapsing/steroid-dependent nephrotic syndrome in children(2016). Zhonghua Er Ke Za Zhi (Chinese), 2017,55(10):729–734
Li T, Jing J, Dong N, et al. TLR4 rs1927914 polymorphism contributes to serum TLR4 levels in patients with aortic aneurysm. Exp Mol Pathol, 2021,119:104609
Wu H, Gao H, Li A, et al. Impact of Genetic Variation in TLR4 3′UTR on NSCLC Genetic Susceptibility. J Oncol, 2020,2020:7593143
Hamann L, Glaeser C, Hamprecht A, et al. Toll-like receptor (TLR)-9 promotor polymorphisms and atherosclerosis. Clin Chim Acta, 2006,364(1–2):303–307
Colucci M, Corpetti G, Emma F, et al. Immunology of idiopathic nephrotic syndrome. Pediatr Nephrol, 2018,33(4):573–584
Campbell RE, Thurman JM. The Immune System and Idiopathic Nephrotic Syndrome. Clin J Am Soc Nephrol, 2022,17(12):1823–1834
Chen SY, Chen CH, Huang YC, et al. Genetic susceptibility to idiopathic membranous nephropathy in high-prevalence Area, Taiwan. Biomedicine (Taipei), 2014,4:9
Chen YT, Wei CC, Ng KL, et al. Toll-like receptor 9 SNPs are susceptible to the development and progression of membranous glomerulonephritis: 27 years follow-up in Taiwan. Ren Fail, 2013,35(10):1370–1375
Shelke V, Kale A, Anders HJ, et al. Epigenetic regulation of Toll-like receptors 2 and 4 in kidney disease. J Mol Med (Berl), 2022,100(7):1017–1026
Larkins NG, Liu ID, Willis NS, et al. Non-corticosteroid immunosuppressive medications for steroid-sensitive nephrotic syndrome in children. Cochrane Database Syst Rev, 2020,4:D2290
Horinouchi T, Nozu K, Iijima K. An updated view of the pathogenesis of steroid-sensitive nephrotic syndrome. Pediatr Nephrol, 2022,37(9):1957–1965
Yang M, Kumar RK, Foster PS. Pathogenesis of steroid-resistant airway hyperresponsiveness: interaction between IFN-gamma and TLR4/MyD88 pathways. J Immunol, 2009,182(8):5107–5115
Kuznetsov NV, Zargari A, Gielen AW, et al. Biomarkers can predict potential clinical responders to DIMS0150 a toll-like receptor 9 agonist in ulcerative colitis patients. BMC Gastroenterol, 2014,14:79
Brown HJ, Lock HR, Wolfs TG, et al. Toll-like receptor 4 ligation on intrinsic renal cells contributes to the induction of antibody-mediated glomerulonephritis via CXCL1 and CXCL2. J Am Soc Nephrol, 2007,18(6):1732–1739
Cunningham PN, Wang Y, Guo R, et al. Role of Toll-like receptor 4 in endotoxin-induced acute renal failure. J Immunol, 2004,172(4):2629–2635
Sato K, Yoshimura A, Kaneko T, et al. A single nucleotide polymorphism in 3′-untranslated region contributes to the regulation of Toll-like receptor 4 translation. J Biol Chem, 2012,287(30):25163–25172
Li Z, Gao H, Liu Y, et al. Genetic variants in the regulation region of TLR4 reduce the gastric cancer susceptibility. Gene, 2021,767:145181
Jiang S, Ma J, Ye S, et al. Associations Among Disseminated Intravascular Coagulation, Thrombocytopenia Cytokines/Chemokines and Genetic Polymorphisms of Toll-Like Receptor 2/4 in Chinese Patients with Sepsis. J Inflamm Res, 2022,15:1–15
Acknowledgments
We thank all the children and their families who participated in this study for their cooperation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Conflict of Interest Statement
The authors declare that they have no conflicts of interest.
This study was funded by the Science and Technology Projects of Zhejiang Province (No. LGC21H200004), the Key Research and Development Plan of Zhejiang Province (No. 2019C03028), and the Medical Scientific Projects from Health Department of Zhejiang Province (No. 2018KY455).
Rights and permissions
About this article
Cite this article
Gao, Hh., Li, W., Shou, Xy. et al. Correlation between Toll-like Receptor Gene Polymorphisms and Idiopathic Nephrotic Syndrome in Chinese Children. CURR MED SCI 43, 585–591 (2023). https://doi.org/10.1007/s11596-023-2728-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-023-2728-3