Abstract
Purpose
The acquisition of good quality ultrasound (US) images requires good acoustic coupling between the ultrasound probe and the patient’s skin. In practice, this good coupling is achieved by the operator applying a force to the skin through the probe. This force induces a deformation of the tissues underlying the probe. The distorted images deteriorate the quality of the reconstructed 3D US image.
Methods
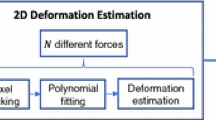
In this work, we propose two methods to correct these deformations. These methods are based on the construction of a biomechanical model to predict the mechanical behavior of the imaged soft tissues. The originality of the methods is that they do not use external information (force or position value from sensors, or elasticity value from the literature). The model is parameterized thanks to the information contained in the image. This is allowed thanks to the optimization of two key parameters for the model which are the indentation d and the elasticity ratio α.
Results
The validation is performed on real images acquired on a gelatin-based phantom using an ultrasound probe inducing an increasing vertical indentation using a step motor. The results showed a good correction of the two methods for indentations less than 4 mm. For larger indentations, one of the two methods (guided by the similarity score) provides a better quality of correction, presenting a Euclidean distance between the contours of the reference image and the corrected image of 0.71 mm.
Conclusion
The proposed methods ensured the correction of the deformed images induced by a linear probe pressure without using any information coming from sensors (force or position), or generic information about the mechanical parameters. The corrected images can be used to obtain a corrected 3D US image.














Similar content being viewed by others
References
Artignan X, Smitsmans MH, Lebesque JV, Jaffray DA, Van Her M, Bartelink H (2004) Online ultrasound image guidance for radiotherapy of prostate cancer: impact of image acquisition on prostate displacement. Int J Radiat Oncol Biol Phys 59(2):595–601
Xiao G, Brady JM, Noble JA, Burcher M, English R (2002) Nonrigid registration of 3-D free-hand ultrasound images of the breast. IEEE Trans Med Imag 21(4):405–412. https://doi.org/10.1109/TMI.2002.1000264
Virga S, Göbl R, Baust M, Navab N, Hennersperger C (2018) Use the force: deformation correction in robotic 3D ultrasound. Int J Comput Assist Radiol Surgry 13(5):619–627. https://doi.org/10.1007/s11548-018-1716-8
Treece GM, Prager RW, Gee AH, Berman L (2002) "Correction of probe pressure artifacts in freehand 3D ultrasound. Med Image Anal 6(3):199–214. https://doi.org/10.1016/S1361-8415(02)00080-4
Lindop JE, Treece GM, Gee AH, Prager RW (2006) 3D elastography using freehand ultrasound. Ultrasound Med Biol 32(4):529–545. https://doi.org/10.1016/j.ultrasmedbio.2005.11.018
Colley E, Carroll J, Thomas S, Varcoe RL, Simmons A, Barber T (2018) A methodology for non-invasive 3-D surveillance of arteriovenous fistulae using freehand ultrasound. IEEE Trans Biomed Eng 65(8):1885–1891. https://doi.org/10.1109/TBME.2017.2782781
Jiang Z, Zhou Y, Bi Y, Zhou M, Wendler T, Navab N (2021) Deformation-aware robotic 3D ultrasound. IEEE Robot Autom Lett 6(4):7675–7682. https://doi.org/10.1109/LRA.2021.3099080
Berge CSZ, Kapoor A, Navab N (2014) Orientation-driven ultrasound compounding using uncertainty information. In: Chama D, Stoyanov DL, Collins I, Sakuma P, Abolmaesumi P, Jannin P (eds) Information processing in computer-assisted interventions. Springer International Publishing, pp 236–245
Sun SY, Anthony BW, Gilbertson MW (2010) Trajectory-based deformation correction in ultrasound images, vol. 7629, pp. 76290A-76290A-9.
Burcher MR, Lianghao H, Noble JA (2001) "Deformation correction in ultrasound images using contact force measurements," In: Proceedings IEEE Workshop on Mathematical Methods in Biomedical Image Analysis (MMBIA 2001), pp. 63–70, https://doi.org/10.1109/MMBIA.2001.991700
Pheiffer TS, Thompson RC, Rucker DC, Simpson AL, Miga MI (2014) Model-based correction of tissue compression for tracked ultrasound in soft tissue image-guided surgery. Ultrasound Med Biol 40(4):788–803. https://doi.org/10.1016/j.ultrasmedbio.2013.11.003
Dahmani J, Petit Y, Laporte C (2017) "Model-based correction of ultrasound image deformations due to probe pressure," In: Medical Imaging 2017: Image Processing, SPIE, vol. 10133, pp. 392–400
Boehler T, Peitgen H-O (2008) Reducing motion artifacts in 3-D breast ultrasound using non-linear registration. In: Metaxas D, Axel L, Fichtinger G, Székely G (eds) Medical image computing and computer-assisted intervention–MICCAI 2008. Springer, Berlin Heidelberg, pp 998–1005
Treece GM, Gee AH, Prager RW (2005) RF and amplitude-based probe pressure correction for 3D ultrasound. Ultrasound Med Biol 31(4):493–503. https://doi.org/10.1016/j.ultrasmedbio.2004.12.018
Chan TF, Vese LA (2001) Active contours without edges. IEEE Trans Image Process 10(2):266–277. https://doi.org/10.1109/83.902291
Dahmani J, Laporte C, Pereira D, Belanger P, Petit Y (2020) "Predictive model for designing soft-tissue mimicking ultrasound phantoms with adjustable elasticity. IEEE Trans Ultrason Ferroelectr Freq Control 67(4):715–726. https://doi.org/10.1109/tuffc.2019.2953190
Funding
Canadian Network for Research and Innovation in Machining Technology, Natural Sciences and Engineering Research Council of Canada, Fonds de recherche du Québec—Nature et technologies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare to have no conflict of interest.
Human and animals rights
No humans or animals were used in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dahmani, J., Petit, Y. & Laporte, C. Quantitative validation of two model-based methods for the correction of probe pressure deformation in ultrasound. Int J CARS 19, 309–320 (2024). https://doi.org/10.1007/s11548-023-03006-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-023-03006-w