Abstract
Purpose
Breast cancer's impact necessitates refined diagnostic approaches. This study develops a nomogram using radiology quantitative features from contrast-enhanced cone-beam breast CT for accurate preoperative classification of benign and malignant breast tumors.
Material and methods
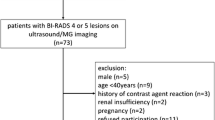
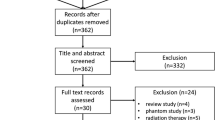
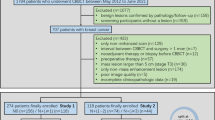
A retrospective study enrolled 234 females with breast tumors, split into training and test sets. Contrast-enhanced cone-beam breast CT-images were acquired using Koning Breast CT-1000. Quantitative assessment features were extracted via 3D-slicer software, identifying independent predictors. The nomogram was constructed to preoperative differentiation benign and malignant breast tumors. Calibration curve was used to assess whether the model showed favorable correspondence with pathological confirmation. Decision curve analysis confirmed the model's superiority.
Results
The study enrolled 234 female patients with a mean age of 50.2 years (SD ± 9.2). The training set had 164 patients (89 benign, 75 malignant), and the test set had 70 patients (29 benign, 41 malignant). The nomogram achieved excellent predictive performance in distinguishing benign and malignant breast lesions with an AUC of 0.940 (95% CI 0.900–0.940) in the training set and 0.970 (95% CI 0.940–0.970) in the test set.
Conclusion
This study illustrates the effectiveness of quantitative radiology features derived from contrast-enhanced cone-beam breast CT in distinguishing between benign and malignant breast tumors. Incorporating these features into a nomogram-based diagnostic model allows for breast tumor diagnoses that are objective and possess good accuracy. The application of these insights could substantially increase reliability and efficacy in the management of breast tumors, offering enhanced diagnostic capability.







Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the receiver operating curve
- BI-RADS:
-
Breast imaging reporting and data system
- CB-BCT:
-
Cone-beam breast CT
- CE CB-BCT:
-
Contrast-enhanced cone-beam breast CT
- CI:
-
Confidence interval
- DCA:
-
Decision curve analysis
- DCIS:
-
Ductal carcinoma in situ
- ICC:
-
Intraclass correlation coefficient
- IQR:
-
Interquartile range
- MG:
-
Mammography
- MRI:
-
Magnetic resonance imaging
- NCE CB-BCT:
-
Non-contrast-enhanced cone-beam breast CT
- NME:
-
Non-mass enhancement
- OR:
-
Odds ratio
- ROC:
-
Receiver operating characteristic
- ROI:
-
Region of interest
- SD:
-
Standard deviation
- US:
-
Ultrasound
References
Arnold M, Morgan E, Rumgay H et al (2022) Current and future burden of breast cancer: global statistics for 2020 and 2040. Breast 66:15–23
Wu J, Li C, Gensheimer M et al (2021) Radiological tumor classification across imaging modality and histology. Nat Mach Intell 3:787–798
Spak DA, Plaxco JS, Santiago L, Dryden MJ, Dogan BE (2017) BI-RADS fifth edition: a summary of changes. Diagn Interv Imaging 98:179–190
Ku YJ, Kim HH, Cha JH et al (2016) Correlation between MRI and the level of tumor-infiltrating lymphocytes in patients with triple-negative breast cancer. AJR Am J Roentgenol 207:1146–1151
Moon HG, Kim N, Jeong S et al (2015) The clinical significance and molecular features of the spatial tumor shapes in breast cancers. PLoS ONE 10:e0143811
He N, Wu Y-P, Kong Y et al (2016) The utility of breast cone-beam computed tomography, ultrasound, and digital mammography for detecting malignant breast tumors: a prospective study with 212 patients. Eur J Radiol 85:392–403
Zhao B, Zhang X, Cai W, Conover D, Ning R (2015) Cone beam breast CT with multiplanar and three dimensional visualization in differentiating breast masses compared with mammography. Eur J Radiol 84:48–53
Wienbeck S, Fischer U, Luftner-Nagel S, Lotz J, Uhlig J (2018) Contrast-enhanced cone-beam breast-CT (CBBCT): clinical performance compared to mammography and MRI. Eur Radiol 28:3731–3741
Uhlig J, Uhlig A, Biggemann L, Fischer U, Lotz J, Wienbeck S (2019) Diagnostic accuracy of cone-beam breast computed tomography: a systematic review and diagnostic meta-analysis. Eur Radiol 29:1194–1202
Ma Y, Liu A, O’Connell AM et al (2021) Contrast-enhanced cone beam breast CT features of breast cancers: correlation with immunohistochemical receptors and molecular subtypes. Eur Radiol 31:2580–2589
Zhu Y, Zhang Y, Ma Y et al (2020) Cone-beam breast CT features associated with HER2/neu overexpression in patients with primary breast cancer. Eur Radiol 30:2731–2739
Li H, Yin L, He N et al (2019) Comparison of comfort between cone beam breast computed tomography and digital mammography. Eur J Radiol 120:108674
Wienbeck S, Lotz J, Fischer U (2017) Review of clinical studies and first clinical experiences with a commercially available cone-beam breast CT in Europe. Clin Imaging 42:50–59
Goto T, Camargo CA, Faridi MK, Freishtat RJ, Hasegawa K (2019) Machine learning-based prediction of clinical outcomes for children during emergency department triage. JAMA Netw Open 2:e186937
Collins GS, Reitsma JB, Altman DG, Moons KGM (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. Ann Intern Med 162:55–63
Steyerberg EW, Bleeker SE, Moll HA, Grobbee DE, Moons KGM (2003) Internal and external validation of predictive models: a simulation study of bias and precision in small samples. J Clin Epidemiol 56:441–447
Steyerberg E (2009) Clinical prediction models: a practical approach to development, validation, and updating
American College of Radiology (ACR) Committee on Drugs and Contrast Media (2021) ACR manual on contrast media. Version 2021. Available via https://www.acr.org/-/media/ACR/Files/Clinical-Resources/Contrast_Media.pdf
European Society of Urogenital Radiology (ESUR) Contrast Medium Safety Committee (2019) ESUR guidelines on contrast agents. version 10.0. Available via https://www.esur.org/wp-content/uploads/2022/03/ESUR-Guidelines-10_0-Final-Version.pdf
Fedorov A, Beichel R, Kalpathy-Cramer J et al (2012) 3D slicer as an image computing platform for the quantitative Imaging network. Magn Reson Imaging 30:1323–1341
Shrout PE, Fleiss JL (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86:420–428
Vigneshwar NG, Moore EE, Moore HB et al (2022) Precision medicine: clinical tolerance to hyperfibrinolysis differs by shock and injury severity. Ann Surg 275:e605–e607
Yu Q, Ning Y, Wang A et al (2023) Deep learning-assisted diagnosis of benign and malignant parotid tumors based on contrast-enhanced CT: a multicenter study. Eur Radiol 33:6054–6065
Tagliafico AS, Piana M, Schenone D, Lai R, Massone AM, Houssami N (2020) Overview of radiomics in breast cancer diagnosis and prognostication. Breast 49:74–80
Michaels AY, Chung CSW, Frost EP, Birdwell RL, Giess CS (2017) Interobserver variability in upgraded and non-upgraded BI-RADS 3 lesions. Clin Radiol 72:694.e691-694.e696
Eghtedari M, Chong A, Rakow-Penner R, Ojeda-Fournier H (2021) Current status and future of BI-RADS in multimodality imaging, from the AJR special series on radiology reporting and data systems. AJR Am J Roentgenol 216:860–873
European Society of R (2015) Medical imaging in personalised medicine: a white paper of the research committee of the European society of radiology (ESR). Insights Imaging 6:141–155
O’Connor JPB, Aboagye EO, Adams JE et al (2017) Imaging biomarker roadmap for cancer studies. Nat Rev Clin Oncol 14:169–186
Galati F, Moffa G, Pediconi F (2022) Breast imaging: beyond the detection. Eur J Radiol 146:110051
Hsu SM, Kuo WH, Kuo FC, Liao YY (2019) Breast tumor classification using different features of quantitative ultrasound parametric images. Int J Comput Assist Radiol Surg 14:623–633
Thakur SB, Horvat JV, Hancu I et al (2019) Quantitative in vivo proton MR spectroscopic assessment of lipid metabolism: value for breast cancer diagnosis and prognosis. J Magn Reson Imaging JMRI 50:239–249
Iima M, Kataoka M, Kanao S et al (2018) Intravoxel incoherent motion and quantitative non-Gaussian diffusion MR imaging: evaluation of the diagnostic and prognostic value of several markers of malignant and benign breast lesions. Radiology 287:432–441
Zhang Q, Spincemaille P, Drotman M et al (2022) Quantitative transport mapping (QTM) for differentiating benign and malignant breast lesion: Comparison with traditional kinetics modeling and semi-quantitative enhancement curve characteristics. Magn Reson Imaging 86:86–93
Liney GP, Sreenivas M, Gibbs P, Garcia-Alvarez R, Turnbull LW (2006) Breast lesion analysis of shape technique: semiautomated vs. manual morphological description. Journal of Magnetic Resonance Imaging : JMRI 23:493–498
Reiser I, Nishikawa RM, Giger ML, Boone JM, Lindfors KK, Yang K (2012) Automated detection of mass lesions in dedicated breast CT: a preliminary study. Med Phys 39:866–873
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144:646–674
Mohammed ZM, McMillan DC, Edwards J et al (2013) The relationship between lymphovascular invasion and angiogenesis, hormone receptors, cell proliferation and survival in patients with primary operable invasive ductal breast cancer. BMC Clin Pathol 13:31
Heaphy CM, Griffith JK, Bisoffi M (2009) Mammary field cancerization: molecular evidence and clinical importance. Breast Cancer Res Treat 118:229–239
Uematsu T (2015) Focal breast edema associated with malignancy on T2-weighted images of breast MRI: peritumoral edema, prepectoral edema, and subcutaneous edema. Breast Cancer (Tokyo, Japan) 22:66–70
Lee KM, Kim EJ, Jahng GH, Park BJ (2014) Value of perfusion weighted magnetic resonance imaging in the diagnosis of supratentorial anaplastic astrocytoma. J Korean Neurosurg Soc 56:261–264
Schwertfeger KL, Cowman MK, Telmer PG, Turley EA, McCarthy JB (2015) Hyaluronan, inflammation, and breast cancer progression. Front Immunol 6:236
Cheon H, Kim HJ, Kim TH et al (2018) Invasive breast cancer: prognostic value of peritumoral edema identified at preoperative MR imaging. Radiology 287:68–75
Shin HJ, Park JY, Shin KC et al (2016) Characterization of tumor and adjacent peritumoral stroma in patients with breast cancer using high-resolution diffusion-weighted imaging: correlation with pathologic biomarkers. Eur J Radiol 85:1004–1011
Fan M, He T, Zhang P, Zhang J, Li L (2017) Heterogeneity of diffusion-weighted imaging in tumours and the surrounding stroma for prediction of Ki-67 proliferation status in breast cancer. Sci Rep 7:2875
Chen JH, Zhang Y, Chan S, Chang RF, Su MY (2018) Quantitative analysis of peri-tumor fat in different molecular subtypes of breast cancer. Magn Reson Imaging 53:34–39
Obeid JP, Stoyanova R, Kwon D et al (2017) Multiparametric evaluation of preoperative MRI in early stage breast cancer: prognostic impact of peri-tumoral fat. Clin Transl Oncol Off Publ Fed Spanish Oncol Soc Natl Cancer Inst Mexico 19:211–218
Braman NM, Etesami M, Prasanna P et al (2017) Intratumoral and peritumoral radiomics for the pretreatment prediction of pathological complete response to neoadjuvant chemotherapy based on breast DCE-MRI. Breast Cancer Res BCR 19:57
Zhou J, Zhang Y, Chang KT et al (2020) Diagnosis of benign and malignant breast lesions on DCE-MRI by using radiomics and deep learning with consideration of peritumor tissue. J Magn Reson Imaging 51:798–809
Çetinkaya E, Yıldız Ş, Otçu H, Sharifov R, Çelik Yabul F, Alkan A (2022) The value of adjacent vessel sign in malignant breast tumors. Diagn Interv Radiol 28:463–469
Caiazzo C, Di Micco R, Esposito E et al (2018) The role of MRI in predicting Ki-67 in breast cancer: preliminary results from a prospective study. Tumori 104:438–443
Shin HJ, Kim HH, Shin KC et al (2016) Prediction of low-risk breast cancer using perfusion parameters and apparent diffusion coefficient. Magn Reson Imaging 34:67–74
Mann RM, Kuhl CK, Kinkel K, Boetes C (2008) Breast MRI: guidelines from the European society of breast imaging. Eur Radiol 18:1307–1318
Macura KJ, Ouwerkerk R, Jacobs MA, Bluemke DA (2006) Patterns of enhancement on breast MR images: interpretation and imaging pitfalls. Radiographics 26(6):1719–1734
Kuhl CK, Mielcareck P, Klaschik S et al (1999) Dynamic breast MR imaging: are signal intensity time course data useful for differential diagnosis of enhancing lesions? Radiology 211:101–110
Huang JS, Pan HB, Yang TL et al (2020) Kinetic patterns of benign and malignant breast lesions on contrast enhanced digital mammogram. PLoS ONE 15:e0239271
Prionas ND, Lindfors KK, Ray S et al (2010) Contrast-enhanced dedicated breast CT: initial clinical experience. Radiology 256:714–723
Phi X-A, Tagliafico A, Houssami N, Greuter MJW, de Bock GH (2018) Digital breast tomosynthesis for breast cancer screening and diagnosis in women with dense breasts - a systematic review and meta-analysis. BMC Cancer 18:380
Sprague BL, Arao RF, Miglioretti DL et al (2017) National performance benchmarks for modern diagnostic digital mammography: update from the breast cancer surveillance consortium. Radiology 283:59–69
Dullum JR, Lewis EC, Mayer JA (2000) Rates and correlates of discomfort associated with mammography. Radiology 214:547–552
Jochelson MS, Dershaw DD, Sung JS et al (2013) Bilateral contrast-enhanced dual-energy digital mammography: feasibility and comparison with conventional digital mammography and MR imaging in women with known breast carcinoma. Radiology 266:743–751
Cong W, Intes X, Wang G (2017) Optical tomographic imaging for breast cancer detection. J Biomed Opt 22:1–6
O’Connell AM, Kawakyu-O’Connor D (2012) Dedicated cone-beam breast computed tomography and diagnostic mammography: comparison of radiation dose, patient comfort, and qualitative review of imaging findings in BI-RADS 4 and 5 lesions. J Clin Imaging Sci 2:7
O’Connell AM, Karellas A, Vedantham S, Kawakyu-O’Connor DT (2018) Newer technologies in breast cancer imaging: dedicated cone-beam breast computed tomography. Semin Ultrasound CT MR 39:106–113
Zhu Y, O’Connell AM, Ma Y et al (2021) Dedicated breast CT: state of the art—part II. Clinical application and future outlook. Eur Radiol 32:2286–2300
Uhlig J, Fischer U, Biggemann L, Lotz J, Wienbeck S (2019) Pre- and post-contrast versus post-contrast cone-beam breast CT: can we reduce radiation exposure while maintaining diagnostic accuracy? Eur Radiol 29:3141–3148
Acknowledgements
The authors thank the patients for their willingness to cooperate with our study. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. This work was supported by the National Key R&D Program of China (2020YFA0714002). The funders had no role in study design, data analysis, decision to publish, or preparation of the manuscript.
Funding
This work was supported by the National Key R&D Program of China (2020YFA0714002) and Joint project of Chongqing Health Commission and Science and Technology Bureau (No. 2022ZDXM006 and 2022QNXM015) and Key Project of Technological Innovation and Application Development of Chongqing Science and Technology Bureau (No. CSTC2021jscxksbN0030).
Author information
Authors and Affiliations
Contributions
TS contributed to the conception and design of the study, completed image acquisition and analysis, interpreted the data, drafted the manuscript, and provided substantial manuscript revisions. YZ contributed to the study's conception and design, data interpretation, and manuscript revision. HY contributed to the image acquisition and analysis. ZO contributed to the completed image acquisition and analysis, the conception and design of the study. JF and LL contributed to the image acquisition. FL contributed to the study's conception and design, and manuscript revision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
Institutional Review Board approval was obtained (2022-K313).
Consent to participation
This retrospective study was approved by the institutional review board of our hospital (2022-K313). The requirement for the patients’ informed consent was waived.
Consent for publication
In this manuscript, all images analyzed are entirely unidentifiable, and the only individual detail provided is the age of the participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Su, T., Zheng, Y., Yang, H. et al. Nomogram for preoperative differentiation of benign and malignant breast tumors using contrast-enhanced cone-beam breast CT (CE CB-BCT) quantitative imaging and assessment features. Radiol med 129, 737–750 (2024). https://doi.org/10.1007/s11547-024-01803-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-024-01803-0