Abstract
Background
The percutaneous thermal ablation techniques (pTA) are radiofrequency ablation, cryoablation, and microwave ablation, suitable for the treatment of bone oligometastases. Magnetic resonance-guided focused ultrasound (MRgFUS) is a noninvasive ablation technique.
Objectives
To compare the effectiveness and safety of MRgFUS and pTA for treating bone oligometastases and their complications.
Methods
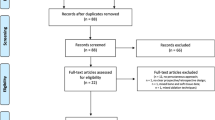
Studies were selected with a PICO/PRISMA protocol: pTA or MRgFUS in patients with bone oligometastases; non-exclusive curative treatment. Exclusion criteria were: primary bone tumor; concurrent radiation therapy; palliative therapy; and absence of imaging at follow-up. PubMed, BioMed Central, and Scopus were searched. The modified Newcastle–Ottawa Scale assessed articles quality. For each treatment (pTA and MRgFUS), we conducted two separate random-effects meta-analyses to estimate the pooled effectiveness and safety. The effectiveness was assessed by combining the proportions of treated lesions achieving local tumor control (LTC); the safety by combining the complications rates of treated patients. Meta-regression analyses were performed to identify any outcome predictor.
Results
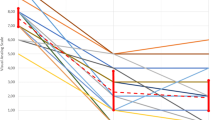
A total of 24 articles were included. Pooled LTC rate for MRgFUS was 84% (N = 7, 95% CI 66–97%, I2 = 74.7%) compared to 65% of pTA (N = 17, 95% CI 51–78%, I2 = 89.3%). Pooled complications rate was similar, respectively, 13% (95% CI 1–32%, I2 = 81.0%) for MRgFUS and 12% (95% CI 8–18%, I2 = 39.9%) for pTA, but major complications were recorded with pTA only.
The meta-regression analyses, including technique type, study design, tumor, and follow-up, found no significant predictors.
Discussion
The effectiveness and safety of the two techniques were found comparable, even though MRgFUS is a noninvasive treatment that did not cause any major complication. Limited data availability on MRgFUS and the lack of direct comparisons with pTA may affect these findings.
Conclusions
MRgFUS can be a valid, safe, and noninvasive treatment for bone oligometastases. Direct comparison studies are needed to confirm its promising benefits.





Similar content being viewed by others
References
Fornetti J, Welm AL, Stewart SA (2018) Understanding the bone in cancer metastasis. J Bone Miner Res 33:2099–2113
Macedo F, Ladeira K, Pinho F, Saraiva N, Bonito N, Pinto L, Goncalves F (2017) Bone metastases: an overview. Oncol Rev 11:321
Wu JS, Wong RK, Lloyd NS, Johnston M, Bezjak A, Whelan T (2004) Supportive Care Guidelines Group of Cancer Care Ontario. Radiotherapy fractionation for the palliation of uncomplicated painful bone metastases—an evidence-based practice guideline. BMC Cancer 4:71
Saravana-Bawan S, David E, Sahgal A, Chow E (2019) Palliation of bone metastases-exploring options beyond radiotherapy. Ann Palliat Med 8:168–177
Deschavanne PJ, Fertil B (1996) A review of human cell radiosensitivity in vitro. Int J Radiat Oncol Biol Phys 34:251–266
Wagner A, Haag E, Joerger AK et al (2021) Comprehensive surgical treatment strategy for spinal metastases. Sci Rep 11:7988
Dupuy DE, Liu D, Hartfeil D et al (2010) Percutaneous radiofrequency ablation of painful osseous metastases: a multicenter American College of Radiology Imaging Network trial. Cancer 116:989–997
Bazzocchi A, Aparisi Gómez MP, Taninokuchi Tomassoni M, Napoli A, Filippiadis D, Guglielmi G (2023) Musculoskeletal oncology and thermal ablation: the current and emerging role of interventional radiology. Skelet Radiol 52:447–459
Kurup AN, Callstrom MR (2016) Increasing role of image-guided ablation in the treatment of musculoskeletal tumors. Cancer J 22:401–410
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev 10:89
Vernuccio F, Godfrey D, Meyer M, Williamson HV, Salama JK, Niedzwiecki D, Stephens SJ, Ronald J, Palta M, Marin D (2019) Local tumor control and patient outcome using stereotactic body radiation therapy for hepatocellular carcinoma: iRECIST as a potential substitute for traditional criteria. AJR Am J Roentgenol 213:1232–1239
Costelloe CM, Chuang HH, Madewell JE et al (2010) Cancer response criteria and bone metastases: RECIST 1.1. MDA and PERCIST J Cancer 1:80–92
Hamaoka T, Madewell JE, Podoloff DA, Hortobagyi GN, Ueno NT (2004) Bone imaging in metastatic breast cancer. J Clin Oncol 22:2942–2953
Omary RA, Bettmann MA, Cardella JF et al (2003) Quality improvement guidelines for the reporting and archiving of interventional radiology procedures. J Vasc Interv Radiol 14:S293–S295
National Cancer Institute (2009) Common Terminology Criteria for Adverse Events (CTCAE). Depart of Health and Human Serv, Nat Inst of Health, Nat Canc Inst (U.S.)
Schieda N, van der Pol CB, Walker D, Tsampalieros AK, Maralani PJ, Woo S, Davenport MS (2020) Adverse events to the gadolinium-based contrast agent gadoxetic acid: systematic review and meta-analysis. Radiology 297(3):565–572
Walker DT, Davenport MS, McGrath TA, McInnes MDF, Shankar T, Breakthrough SN (2020) Hypersensitivity reactions to gadolinium-based contrast agents and strategies to decrease subsequent reaction rates: a systematic review and meta-analysis. Radiology 296(2):312–321
Cazzato RL, Palussière J, Buy X, Denaro V, Santini D, Tonini G, Grasso RF, Zobel BB, Poretti D, Pedicini V, Balzarini L, Lanza E (2015) Percutaneous long bone cementoplasty for palliation of malignant lesions of the limbs: a systematic review. Cardiovasc Intervent Radiol 38:1563–1572
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Autrusseau PA, Schneegans O, Koch G, Weiss J, Caudrelier J, Dalili D, Perolat R, Auloge P, Cazzato RL, Gangi A, Garnon J (2022) Safety and efficacy of percutaneous cryoablation of extraspinal thyroid cancer bone metastases with curative intent: single-center experience with a median follow-up of more than 5 years. J Vasc Interv Radiol 33:797–804
Arrigoni F, Bianchi G, Formiconi F, Palumbo P, Zugaro L, Gravina GL, Barile A, Masciocchi C (2022) CT-guided cryoablation for management of bone metastases: a single center experience and review of the literature. Radiol Med 127:199–205
Cazzato RL, De Marini P, Leonard-Lorant I, Dalili D, Koch G, Autrusseau PA, Mayer T, Weiss J, Auloge P, Garnon J, Gangi A (2021) Percutaneous thermal ablation of sacral metastases: Assessment of pain relief and local tumor control. Diagn Interv Imaging 102:355–361
Giles SL, Brown MRD, Rivens I, Deppe M, Huisman M, Kim YS, Farquhar-Smith P, Williams JE, Ter Haar GR, deSouza NM (2019) Comparison of imaging changes and pain responses in patients with intra- or extraosseous bone metastases treated palliatively with magnetic resonance-guided high-intensity-focused ultrasound. J Vasc Interv Radiol 30:1351–1360
Gallusser N, Goetti P, Becce F, Vauclair F, Rüdiger HA, Bize PE, Cherix S (2019) Percutaneous image-guided cryoablation of painful bone metastases: a single institution experience. Orthop Traumatol Surg Res 105:369–374
Tsai YC, Lee HL, Kuo CC, Chen CY, Hsieh KL, Wu MH, Wen YC, Yu HW, Hsu FC, Tsai JT, Chiou JF (2019) Prognostic and predictive factors for clinical and radiographic responses in patients with painful bone metastasis treated with magnetic resonance-guided focused ultrasound surgery. Int J Hyperthermia 36:932–937
Luigi Cazzato R, Auloge P, De Marini P, Rousseau C, Chiang JB, Koch G, Caudrelier J, Rao P, Garnon J, Gangi A (2018) Percutaneous image-guided ablation of bone metastases: local tumor control in oligometastatic patients. Int J Hyperthermia 35:493–499
Ma Y, Wallace AN, Waqar SN, Morgensztern D, Madaelil TP, Tomasian A, Jennings JW (2018) Percutaneous image-guided ablation in the treatment of osseous metastases from non-small cell lung cancer. Cardiovasc Intervent Radiol 41:726–733
Vaswani D, Wallace AN, Eiswirth PS, Madaelil TP, Chang RO, Tomasian A, Jennings JW (2018) Radiographic local tumor control and pain palliation of sarcoma metastases within the musculoskeletal system with percutaneous thermal ablation. Cardiovasc Intervent Radiol 41:1223–1232
Gardner CS, Ensor JE, Ahrar K, Huang SY, Sabir SH, Tannir NM, Lewis VO, Tam AL (2017) Cryoablation of bone metastases from renal cell carcinoma for local tumor control. J Bone Joint Surg Am 99:1916–1926
Singh VA, Shah SU, Yasin NF, Abdullah BJJ (2017) Magnetic resonance-guided focused ultrasound for the treatment of bone tumors. J Orthop Surg (Hong Kong) 25:1–7
Erie AJ, Morris JM, Welch BT, Kurup AN, Weisbrod AJ, Atwell TD, Schmit GD, Kwon ED, Callstrom MR (2017) Retrospective review of percutaneous image-guided ablation of oligometastatic prostate cancer: a single-institution experience. J Vasc Interv Radiol 28:987–992
Aubry S, Dubut J, Nueffer JP, Chaigneau L, Vidal C, Kastler B (2017) Prospective 1-year follow-up pilot study of CT-guided microwave ablation in the treatment of bone and soft-tissue malignant tumours. Eur Radiol 27:1477–1485
McArthur TA, Narducci CA, Lander PH, Lopez-Ben R (2017) Percutane image-guided cryoablation of painful osseous metastases: a retrospective single-center review. Curr Probl Diagn Radiol 46:282–287
Wallace AN, McWilliams SR, Connolly SE, Symanski JS, Vaswani D, Tomasian A, Vyhmeister R, Lee AM, Madaelil TP, Hillen TJ, Jennings JW (2016) Percutaneous image-guided cryoablation of musculoskeletal metastases: pain palliation and local tumor control. J Vasc Interv Radiol 27:1788–1796
Anzidei M, Napoli A, Sacconi B, Boni F, Noce V, Di Martino M, Saba L, Catalano C (2016) Magnetic resonance-guided focused ultrasound for the treatment of painful bone metastases: role of apparent diffusion coefficient (ADC) and dynamic contrast enhanced (DCE) MRI in the assessment of clinical outcome. Radiol Med 121:905–915
Wallace AN, Tomasian A, Vaswani D, Vyhmeister R, Chang RO, Jennings JW (2016) Radiographic local control of spinal metastases with percutaneous radiofrequency ablation and vertebral augmentation. AJNR Am J Neuroradiol 37:759–765
Tomasian A, Wallace A, Northrup B, Hillen TJ, Jennings JW (2016) Spine cryoablation: pain palliation and local tumor control for vertebral metastases. AJNR Am J Neuroradiol 37:189–195
Joo B, Park MS, Lee SH, Choi HJ, Lim ST, Rha SY, Rachmilevitch I, Lee YH, Suh JS (2015) Pain palliation in patients with bone metastases using magnetic resonance-guided focused ultrasound with conformal bone system: a preliminary report. Yonsei Med J 56:503–509
Hegg RM, Kurup AN, Schmit GD, Weisbrod AJ, Atwell TD, Olivier KR, Moynihan TJ, Callstrom MR (2014) Cryoablation of sternal metastases for pain palliation and local tumor control. J Vasc Interv Radiol 25:1665–1670
Deschamps F, Farouil G, Ternes N, Gaudin A, Hakime A, Tselikas L, Teriitehau C, Baudin E, Auperin A, de Baere T (2014) Thermal ablation techniques: a curative treatment of bone metastases in selected patients? Eur Radiol 24:1971–1980
McMenomy BP, Kurup AN, Johnson GB, Carter RE, McWilliams RR, Markovic SN, Atwell TD, Schmit GD, Morris JM, Woodrum DA, Weisbrod AJ, Rose PS, Callstrom MR (2013) Percutaneous cryoablation of musculoskeletal oligometastatic disease for complete remission. J Vasc Interv Radiol 24:207–213
Napoli A, Anzidei M, Marincola BC, Brachetti G, Ciolina F, Cartocci G, Marsecano C, Zaccagna F, Marchetti L, Cortesi E et al (2013) Primary pain palliation and local tumor control in bone metastases treated with magnetic resonance-guided focused ultrasound. Invest Radiol 48:351–358
Gianfelice D, Gupta C, Kucharczyk W, Bret P, Havill D, Clemons M (2008) Palliative treatment of painful bone metastases with MR imaging-guided focused ultrasound. Radiology 249:355–363
Wood JA (2008) Methodology for dealing with duplicate study effects in a meta-analysis. Organ Res Methods 11:79–95
Reyes DK, Pienta KJ (2015) The biology and treatment of oligometastatic cancer. Oncotarget 6:8491–8524
Spratt DE, Beeler WH, de Moraes FY, Rhines LD, Gemmete JJ, Chaudhary N, Shultz DB, Smith SR, Berlin A, Dahele M et al (2017) An integrated multidisciplinary algorithm for the management of spinal metastases: an International Spine Oncology Consortium report. Lancet Oncol 18:e720–e730
Quan GMY, Pointillart V, Palussière J, Bonichon F (2012) Multidisciplinary treatment and survival of patients with vertebral metastases from thyroid carcinoma. Thyroid 22:125–130
Capanna R, Piccioli A, Di Martino A, Daolio PA, Ippolito V, Maccauro G, Piana R, Ruggieri P, Gasbarrini A, Spinelli MS et al (2014) Management of long bone metastases: recommendations from the Italian Orthopaedic Society bone metastasis study group. Expert Rev Anticancer Ther 14:1127–1134
Horn SR, Dhillon ES, Poorman GW, Tishelman JC, Segreto FA, Bortz CA, Moon JY, Behery O, Shepard N, Diebo BG et al (2018) Epidemiology and national trends in prevalence and surgical management of metastatic spinal disease. J Clin Neurosci 53:183–187
Gennaro N, Sconfienza LM, Ambrogi F, Boveri S, Lanza E (2019) Thermal ablation to relieve pain from metastatic bone disease: a systematic review. Skeletal Radiol 48:1161–1169
Mehta TI, Heiberger C, Kazi S, Brown M, Weissman S, Hong K, Mehta M, Yim D (2020) Effectiveness of radiofrequency ablation in the treatment of painful osseous metastases: a correlation meta-analysis with machine learning cluster identification. J Vasc Interv Radiol 31:1753–1762
Kurup AN, Callstrom MR (2010) Image-guided percutaneous ablation of bone and soft tissue tumors. Semin Interv Radiol 27:276–284
Jolesz FA, McDannold NJ (2014) Magnetic resonance-guided focused ultrasound: a new technology for clinical neurosciences. Neurol Clin 32:253–269
Baal JD, Chen WC, Baal U, Wagle S, Baal JH, Link TM, Bucknor MD (2021) Efficacy and safety of magnetic resonance-guided focused ultrasound for the treatment of painful bone metastases: a systematic review and meta-analysis. Skeletal Radiol 50:2459–2469
Mercadante S, Fulfaro F (2007) Management of painful bone metastases. Curr Opin Oncol 19:308–314
Ferrario L, Garagiola E, Gerardi C, Bellavia G, Colombo S, Ticca C, Rossetti C, Ciboldi M, Meroni M, Vanzulli A et al (2022) Innovative and conventional “conservative” technologies for the treatment of uterine fibroids in Italy: a multidimensional assessment. Health Econ Rev 12:21
Yamamoto K, Sarica C, Loh A, Vetkas A, Samuel N, Milano V, Zemmar A, Germann J, Cheyuo C, Boutet A et al (2022) Magnetic resonance-guided focused ultrasound for the treatment of tremor. Expert Rev Neurother 22:849–861
Cobianchi Bellisari F, Palumbo P, Masciocchi C, Zoccali C, Barile A, Arrigoni F (2021) Needleless ablation of osteoid osteoma and osteoblastoma: the emergent role of MRgFUS. J Clin Med 11:128
Borasi G, Russo G, Alongi F, Nahum A, Candiano GC, Stefano A, Gilardi MC, Messa C (2013) High-intensity focused ultrasound plus concomitant radiotherapy: a new weapon in oncology? J Ther Ultrasound 1:6
Masala S, Schillaci O, Bartolucci AD, Calabria F, Mammucari M, Simonetti G (2011) Metabolic and clinical assessment of efficacy of cryoablation therapy on skeletal masses by 18F-FDG positron emission tomography/computed tomography (PET/CT) and visual analogue scale (VAS): initial experience. Skeletal Radiol 40:159–165
Manenti G, Cicciò C, Squillaci E, Strigari L, Calabria F, Danieli R, Schillaci O, Simonetti G (2012) Role of combined DWIBS/3D-CE-T1w whole-body MRI in tumor staging: comparison with PET-CT. Eur J Radiol 81:1917–1925
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study. ML was responsible for the study's conception, design, and research. VB was responsible for the statistical analysis. FC collaborated on the statistical methodology. ML, FC, and VL wrote the manuscript. FC, VL, and DKF revised and corrected the manuscript. LT and RI coordinated and supervised the work. All authors read and approved the manuscript for submission.
Corresponding author
Ethics declarations
Conflict of interest
Authors do not have conflicts of interest in the manuscript, including financial, consultant, institutional, and other relationships that might lead to bias or a conflict of interest.
Informed consent
Written informed consent was not required for this study.
Ethical approval
Institutional review board approval was not required.
Human and animal rights
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Leporace, M., Lancellotta, V., Baccolini, V. et al. Magnetic resonance-guided focused ultrasound versus percutaneous thermal ablation in local control of bone oligometastases: a systematic review and meta-analysis. Radiol med 129, 291–306 (2024). https://doi.org/10.1007/s11547-024-01780-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-024-01780-4