Abstract
Purpose
We aimed at assessing the predictive ability of ultrasound-based radiomics combined with clinical characteristics for axillary lymph node (ALN) status in early-stage breast cancer patients and to compare performance in different peritumoral regions.
Materials and methods
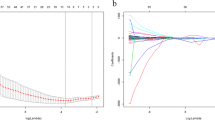
A total of 755 patients (527 in the primary cohort and 228 in the external validation cohort) were enrolled in this study. Ultrasound images for all patients were acquired and radiomics analysis performed for intratumoral and different peritumoral regions. The MRMR and LASSO regression analyses were performed on extracted features from the primary cohort to construct a radiomics signature formula combined with clinical characteristics. Pearson’s coefficient and the variance inflation factor (VIF) were performed to check the correlation and the multicollinearity among the final predictors. The best performing model was selected to develop a nomogram, which was established by performing binary logistic regression and acquiring cut-off values based on the corresponding nomogram scores of the masses.
Results
Among all the radiomics models, the “Mass + Margin3mm” model exhibited the best performance. The areas under the curves (AUC) of the nomogram in the primary and external validation cohorts were 0.906 (95% confidence intervals [CI] 0.882–0.930) and 0.922 (95% CI 0.894–0.960), respectively. They both showed good calibrations. The nomogram exhibited a good ability to discriminate between positive and negative lymph nodes (AUC: 0.853 (95% CI 0.816–0.889) in primary cohort, 0.870 (95% CI 0.818–0.922) in validation cohort), and between low-volume and high-volume lymph nodes (AUC: 0.832 (95% CI 0.781–0.884) in primary cohort, 0.911 (95% CI 0.858–0.964) in validation cohort).
Conclusions
The established nomogram is a prospective clinical prediction tool for non-invasive assessment of ALN status. It has the ability to enhance the accuracy of early-stage breast cancer treatment.





Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are not publicly available due to patient permission was not sought for the sharing of data at the time of recruitment, but are available from the corresponding author on reasonable request.
Abbreviations
- ALN:
-
Axillary lymph node
- ALND:
-
Axillary lymph node dissection
- ALNM:
-
Axillary lymph node metastasis
- AUC:
-
Area under curve
- BI-RADS:
-
The breast imaging reporting and data system
- BMUS:
-
B-mode ultrasound
- DCA:
-
Decision curve analysis
- DFS:
-
Disease-free survival
- ER:
-
Estrogenic receptor
- FNR:
-
False negative rate
- FPR:
-
False positive rate
- HER2:
-
Human epidermal growth factor receptor-2
- ICCs:
-
Interclass correlation coefficients
- LASSO:
-
Least absolute shrinkage and selection operator
- LRNI:
-
Locoregional nodal irradiation
- MRMR:
-
Max-relevance and min-redundancy
- NPV:
-
Negative predictive value
- PPV:
-
Positive Predictive Value
- PR:
-
Progesterone receptor
- ROC:
-
Receiver operating characteristic
- ROI:
-
Region of interest
- SLNB:
-
Sentinel lymph node biopsy
- SLND:
-
Sentinel lymph node dissection
- US:
-
Ultrasound
- VIF:
-
Variance inflation factor
References
Park KU, Caudle A (2018) Management of the axilla in the patient with breast cancer. Surg Clin North Am 98(4):747–760
Giuliano AE, Ballman KV, McCall L, Beitsch PD, Brennan MB, Kelemen P et al (2017) Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with Invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (alliance) randomized clinical trial. JAMA 318(10):918–926
Brackstone M, Baldassarre FG, Perera FE, Cil T, Chavez Mac Gregor M, Dayes IS et al (2021) Management of the axilla in early-stage breast cancer: ontario health (cancer care ontario) and ASCO guideline. J Clin Oncol 39(27):3056–3082
Boughey JC, Moriarty JP, Degnim AC, Gregg MS, Egginton JS, Long KH (2010) Cost modeling of preoperative axillary ultrasound and fine-needle aspiration to guide surgery for invasive breast cancer. Ann Surg Oncol 17(4):953–958
Guo R, Lu G, Qin B, Fei B (2018) Ultrasound imaging technologies for breast cancer detection and management: a review. Ultrasound Med Biol 44(1):37–70
Evans A, Rauchhaus P, Whelehan P, Thomson K, Purdie CA, Jordan LB et al (2014) Does shear wave ultrasound independently predict axillary lymph node metastasis in women with invasive breast cancer? Breast Cancer Res Treat 143(1):153–157
Luo Y, Zhao C, Gao Y, Xiao M, Li W, Zhang J et al (2020) Predicting axillary lymph node status with a nomogram based on breast lesion ultrasound features: performance in N1 breast cancer patients. Front Oncol 10:581321
Zhang H, Dong Y, Jia X, Zhang J, Li Z, Chuan Z et al (2022) Comprehensive risk system based on shear wave elastography and BI-RADS categories in assessing axillary lymph node metastasis of invasive breast cancer—a multicenter study. Front Oncol 12:830910
Bi WL, Hosny A, Schabath MB, Giger ML, Birkbak NJ, Mehrtash A et al (2019) Artificial intelligence in cancer imaging: clinical challenges and applications. CA Cancer J Clin 69(2):127–157
Lambin P, Rios-Velazquez E, Leijenaar R, Carvalho S, van Stiphout RG, Granton P et al (2012) Radiomics: extracting more information from medical images using advanced feature analysis. Eur J Cancer 48(4):441–446
Jiang M, Li CL, Luo XM, Chuan ZR, Chen RX, Tang SC et al (2022) Radiomics model based on shear-wave elastography in the assessment of axillary lymph node status in early-stage breast cancer. Eur Radiol 32(4):2313–2325
Koelliker SL, Chung MA, Mainiero MB, Steinhoff MM, Cady B (2008) Axillary lymph nodes: US-guided fine-needle aspiration for initial staging of breast cancer–correlation with primary tumor size. Radiology 246(1):81–89
Tabachnick B, Fidell LS (2007) Using multivariate statistics, 5th edn. Allyn & Bacon/Pearson Education, Boston, PA
Akinwande MO, Dikko HG, Samson A (2015) V ariance inflation factor: As a condition for the inclusion of suppressor variable(s) in regression analysis. Open J Stat 5:754
Galimberti V, Cole BF, Viale G, Veronesi P, Vicini E, Intra M et al (2018) Axillary dissection versus no axillary dissection in patients with breast cancer and sentinel-node micrometastases (IBCSG23-01): 10-year follow-up of a randomised, controlled phase 3 trial. Lancet Oncol 19:1385–1393
Meretoja TJ, Leidenius MH, Heikkilä PS, Boross G, Sejben I, Regitnig P et al (2012) International multicenter tool to predict the risk of nonsentinel node metastases in breast cancer. J Natl Cancer Inst 104:1888–1896
Zheng X, Yao Z, Huang Y, Yu Y, Wang Y, Liu Y et al (2021) Deep learning radiomics can predict axillary lymph node status in early-stage breast cancer. Nat Commun 11(1):1236
Krag DN, Anderson SJ, Julian TB, Brown AM, Harlow SP, Ashikaga T et al (2007) Technical outcomes of sentinel-lymph-node resection and conventional axillary-lymph-node dissection in patients with clinically node-negative breast cancer: results from the NSABP B-32 randomised phase III trial. Lancet Oncol 8(10):881–888
Pesek S, Ashikaga T, Krag LE, Krag D (2012) The false-negative rate of sentinel node biopsy in patients with breast cancer: a meta-analysis. World J Surg 36(9):2239–2251
Dong F, She R, Cui C, Shi S, Hu X, Zeng J et al (2021) One step further into the blackbox: a pilot study of how to build more confidence around an AI-based decision system of breast nodule assessment in 2D ultrasound. Eur Radiol 31(7):4991–5000
Zhou J, Zhan W, Chang C, Zhang X, Jia Y, Dong Y et al (2014) Breast lesions: evaluation with shear wave elastography, with special emphasis on the “stiff rim” sign. Radiology 272(1):63–72
Han X, Cao W, Wu L, Liang C (2022) Radiomics assessment of the tumor immune microenvironment to predict outcomes in breast cancer. Front Immunol 12:773581
Reyal F, Rouzier R, Depont-Hazelzet B, Bollet MA, Pierga JY, Alran S et al (2011) The molecular subtype classification is a determinant of sentinel node positivity in early breast carcinoma. PLoS ONE 6(5):e20297
Braman N, Prasanna P, Whitney J, Singh S, Beig N, Etesami M et al (2019) Association of peritumoral radiomics with tumor biology and pathologic response to preoperative targeted therapy for HER2 (ERBB2)-positive breast cancer. JAMA Netw Open 2(4):e192561
Zhang Y, Zhu Y, Zhang K, Liu Y, Cui J, Tao J et al (2020) Invasive ductal breast cancer: preoperative predict Ki-67 index based on radiomics of ADC maps. Radiol Med (Torino) 125(2):109–116
Gursoy M, Sezgin G, Horoz EM, Dirim Mete B, Erdogan N (2019) Histopathological and tumor characteristics associated with false negative axillary ultrasonography results in breast cancer. Med Ultrason 21(3):232–238
Zhan C, Hu Y, Wang X, Liu H, Xia L, Ai T (2022) Prediction of axillary lymph node metastasis in breast cancer using intra-peritumoral textural transition analysis based on dynamic contrast-enhanced magnetic resonance imaging. Acad Radiol 29(Suppl 1):S107–S115
Veronesi U, Paganelli G, Viale G, Luini A, Zurrida S, Galimberti V et al (2003) A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. N Engl J Med 349(6):546–553
Acknowledgments
The authors thank Home for Researchers editorial team (https://www.home-for-researchers.com) for language editing service.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and material preparation and analysis were performed by JS, HW, XD, WX, SW and YW. The first draft of the manuscript was written by WZ and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest. The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This retrospective study was approved by the ethical committee and informed consents were obtained from all patients (approval number: KY2022-301).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, W., Wang, S., Wang, Y. et al. Ultrasound-based radiomics nomogram for predicting axillary lymph node metastasis in early-stage breast cancer. Radiol med 129, 211–221 (2024). https://doi.org/10.1007/s11547-024-01768-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-024-01768-0