Abstract
Purpose
Dual-energy X-ray absorptiometry (DXA) is the gold standard for measuring bone mineral density (BMD) with tolerable error rate, high precision, and excellent consistency. Our objective was to investigate the frequency and distribution of errors in a cohort of patients with Thalassemia major (TM).
Methods
We reviewed the DXA examinations of 340 patients with β-TM followed by our institution, acquired in different imaging centers between 2009 and 2019. We collected sex and age at the time of the first examination and at the last visit, as well as BMD, T-score, and Z-score values. Errors were analyzed by anatomical site (lumbar spine, total hip, femoral neck).
Results
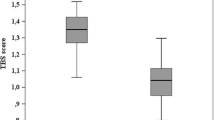
Out of 5099 total DXA scans, 11.85% presented one or more errors. Specifically, the incorrect examinations were 315 out of 1707 (18.45%) at the lumbar spine level, 113 out of 1697 (6.66%) at the total hip, 176 out of 1695 (10.38%) at the femoral neck. Errors in vertebral inclusion were the most frequently registered (45.86%). A significant difference resulted from the comparison of the T-score and Z-score median values of all the lumbar spine DXA examinations and the correct ones (p value 0.037 and 0.0003, respectively).
Conclusion
Although not directly involved in the performance and interpretation of DXA, physicians interested in osteoporosis management should be familiar with the protocols to minimize errors and allow the proper use of bone densitometry. DXA obtained at the spine level is more frequently affected by errors in patients with TM, potentially influencing the diagnostic assessment of bone health status.



Similar content being viewed by others
References
Origa R (1993) Beta-Thalassemia. In: Adam MP, Everman DB, Mirzaa GM et al (eds) GeneReviews®. University of Washington, Seattle
Voskaridou E, Kattamis A, Fragodimitri C et al (2019) National registry of hemoglobinopathies in Greece: updated demographics, current trends in affected births, and causes of mortality. Ann Hematol. https://doi.org/10.1007/s00277-018-3493-4
Pellegrino F, Zatelli MC, Bondanelli M et al (2019) Dual-energy X-ray absorptiometry pitfalls in Thalassemia major. Endocrine 65:469–482. https://doi.org/10.1007/s12020-019-02003-x
Tubman VN, Fung EB, Vogiatzi M et al (2015) Guidelines for the standard monitoring of patients with Thalassemia: report of the Thalassemia longitudinal cohort. J Pediatr Hematol Oncol 37:e162-169. https://doi.org/10.1097/MPH.0000000000000307
Guidelines for the management of transfusion dependent Thalassaemia (4th edition – Version 2.0). In: TIF. https://thalassaemia.org.cy/publications/tif-publications/guidelines-for-the-management-of-transfusion-dependent-thalassaemia-4th-edition-2021-v2/. Accessed 22 Oct 2022
Shepherd JA, Schousboe JT, Broy SB et al (2015) Executive summary of the 2015 ISCD position development conference on advanced measures from DXA and QCT: fracture prediction beyond BMD. J Clin Densitom Off J Int Soc Clin Densitom 18(3):274–286. https://doi.org/10.1016/j.jocd.2015.06.013
Gordon CM, Leonard MB, Zemel BS (2014) International society for clinical densitometry 2013 pediatric position development conference: executive summary and reflections. J Clin Densitom Off J Int Soc Clin Densitom 17:219–224. https://doi.org/10.1016/j.jocd.2014.01.007
Carnevale A, Pellegrino F, Bravi B et al (2022) The role of opportunistic quantitative computed tomography in the evaluation of bone disease and risk of fracture in Thalassemia major. Eur J Haematol n/a. https://doi.org/10.1111/ejh.13847
Albano D, Agnollitto PM, Petrini M et al (2021) Operator-related errors and pitfalls in dual energy X-ray absorptiometry: how to recognize and avoid them. Acad Radiol 28:1272–1286. https://doi.org/10.1016/j.acra.2020.07.028
Krueger D, Shives E, Siglinsky E et al (2019) DXA errors are common and reduced by use of a reporting template. J Clin Densitom Off J Int Soc Clin Densitom 22:115–124. https://doi.org/10.1016/j.jocd.2018.07.014
Messina C, Bandirali M, Sconfienza LM et al (2015) Prevalence and type of errors in dual-energy X-ray absorptiometry. Eur Radiol 25:1504–1511. https://doi.org/10.1007/s00330-014-3509-y
Garg MK, Kharb S (2013) Dual energy X-ray absorptiometry: pitfalls in measurement and interpretation of bone mineral density. Indian J Endocrinol Metab 17:203–210. https://doi.org/10.4103/2230-8210.109659
Borges JLC, Sousa da Silva M, Ward RJ et al (2019) Repeating vertebral fracture assessment: 2019 ISCD official position. J Clin Densitom Off J Int Soc Clin Densitom 22:484–488. https://doi.org/10.1016/j.jocd.2019.07.005
ISCD, the International Society of Clinical Densitometry (2019) 2019 ISCD official positions—Adult
Chan YL, Pang LM, Chik KW et al (2002) Patterns of bone diseases in transfusion-dependent homozygous thalassaemia major: predominance of osteoporosis and desferrioxamine-induced bone dysplasia. Pediatr Radiol 32:492–497. https://doi.org/10.1007/s00247-002-0664-0
Korovessis P, Papanastasiou D, Tiniakou M, Beratis NG (1996) Incidence of scoliosis in beta-Thalassemia and follow-up evaluation. Spine 21:1798–1801. https://doi.org/10.1097/00007632-199608010-00015
Watts NB (2004) Fundamentals and pitfalls of bone densitometry using dual-energy X-ray absorptiometry (DXA). Osteoporos Int J Establ Result Coop Eur Found Osteoporos Natl Osteoporos Found USA 15:847–854. https://doi.org/10.1007/s00198-004-1681-7
Glüer CC (2000) The use of bone densitometry in clinical practice. Baillieres Best Pract Res Clin Endocrinol Metab 14:195–211. https://doi.org/10.1053/beem.2000.0069
Licata AA, Binkley N, Petak SM, Camacho PM (2018) Consensus statement by the American association of clinical endocrinologists and American college of endocrinology on the quality of DXA scans and reports. Endocr Pract Off J Am Coll Endocrinol Am Assoc Clin Endocrinol 24:220–229. https://doi.org/10.4158/CS-2017-0081
Shuhart CR, Yeap SS, Anderson PA et al (2019) Executive summary of the 2019 ISCD position development conference on monitoring treatment, DXA cross-calibration and least significant change, spinal cord injury, peri-prosthetic and orthopedic bone health, transgender medicine, and pediatrics. J Clin Densitom 22(4):453–471. https://doi.org/10.1016/j.jocd.2019.07.001
Messina C, Sconfienza LM, Bandirali M et al (2016) Adult dual-energy X-ray absorptiometry in clinical practice: how i report it. Semin Musculoskelet Radiol 20:246–253. https://doi.org/10.1055/s-0036-1592370
Lewiecki EM, Gordon CM, Baim S et al (2008) International society for clinical densitometry 2007 adult and pediatric official positions. Bone 43:1115–1121. https://doi.org/10.1016/j.bone.2008.08.106
Shevroja E, Cafarelli FP, Guglielmi G, Hans D (2021) DXA parameters, trabecular bone score (TBS) and bone mineral density (BMD), in fracture risk prediction in endocrine-mediated secondary osteoporosis. Endocrine 74:20–28. https://doi.org/10.1007/s12020-021-02806-x
Wong P, Fuller PJ, Gillespie MT et al (2014) Thalassemia bone disease: a 19-year longitudinal analysis. J Bone Miner Res Off J Am Soc Bone Miner Res 29:2468–2473. https://doi.org/10.1002/jbmr.2266
Baldini M, Marcon A, Ulivieri FM et al (2017) Bone quality in beta-Thalassemia intermedia: relationships with bone quantity and endocrine and hematologic variables. Ann Hematol 96:995–1003. https://doi.org/10.1007/s00277-017-2959-0
Osella G, Priola AM, Priola SM et al (2018) Dual-energy X-ray absorptiometry predictors of vertebral deformities in beta-Thalassemia major. J Clin Densitom 21:507–516. https://doi.org/10.1016/j.jocd.2017.06.028
Hansen KE, Binkley N, Christian R et al (2005) Interobserver reproducibility of criteria for vertebral body exclusion. J Bone Miner Res Off J Am Soc Bone Miner Res 20:501–508. https://doi.org/10.1359/JBMR.041134
Hansen KE, Binkley N, Blank RD et al (2007) An atlas improves interobserver agreement regarding application of the ISCD vertebral body exclusion criteria. J Clin Densitom Off J Int Soc Clin Densitom 10:359–364. https://doi.org/10.1016/j.jocd.2007.08.003
Tsang JF, Leslie WD (2007) Exclusion of focal vertebral artifacts from spine bone densitometry and fracture prediction: a comparison of expert physicians, three computer algorithms, and the minimum vertebra. J Bone Miner Res Off J Am Soc Bone Miner Res 22:789–798. https://doi.org/10.1359/jbmr.070319
Acknowledgements
We thank Dr Roberto Reverberi for statistical analysis. We are grateful to United Onlus for their assistance and active participation in clinical and educational activities.
Funding
This study received no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Elisa Lucioni, Fabio Pellegrino, Damiano Remor, Desy Niero, Filomena Longo, Maria Chiara Zatelli, Melchiore Giganti, Aldo Carnevale, and Maria Rosaria Ambrosio declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lucioni, E., Pellegrino, F., Remor, D. et al. Bone densitometry in Thalassemia major: a closer look at pitfalls and operator-related errors in a 10-year follow-up population. Radiol med 129, 488–496 (2024). https://doi.org/10.1007/s11547-024-01759-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-024-01759-1