Abstract
Purpose
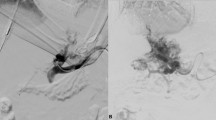
This study aims to analyze safety and effectiveness of PHIL® (Microvention, CA-USA) in peripheral endovascular embolization procedures, both in elective and emergent scenarios.
Materials and Methods
This is a multicenter retrospective study, involving 178 patients from five interventional radiology departments from January 2017 to December 2021. Patients treated by an endovascular embolization with PHIL® were included; different PHIL® viscosities were adopted. Exclusion criteria were: neuroradiological endovascular interventions, other cohesive liquid embolics adopted during the same procedure, follow-up < 30 days. Technical success was intended as definitive target vessel occlusion without the need for other embolics after PHIL® injection. Clinical success was considered as restoration of hemodynamic status in case of emergent embolization and improvement of clinical conditions in case of elective procedures, without additional interventions at 30 days.
Results
Sixty-four women and 114 men, mean age 62 years (range 6–91), were evaluated. Sixty-three patients were in elective scenarios (AVMs, type-II endoleaks, tumors, varices, aneurysms, varicoceles) and 115 were in emergent settings (hemorrhage, pseudoaneurysms, hemoptysis, priapism); 190 procedures were performed in 178 patients. Overall technical and clinical success rates were 94.7% and 92.1%, respectively. The complications rate was 7.4% (6 grade-I, 7 grade-III, 1 grade-IV). PHIL®-25 was the more adopted viscosity; totally, 311 vials were injected (rate: 1.64 vial/procedure).
Conclusion
In this series, PHIL® proved to be a safe and effective liquid embolic in peripheral embolizations, both in elective and emergent scenarios. The pre-filled syringe preparation allowed operators to use it even when unplanned at beginning of the intervention.






Similar content being viewed by others
References
Molyneux AJ, Coley SC (2000) Embolization of spinal cord arteriovenous malformations with an ethylene vinyl alcohol copolymer dissolved in dimethyl sulfoxide (Onyx liquid embolic system): Report of two cases. J Neurosurg 93(2 Suppl):304–8
Lucatelli P, Corona M, Teodoli L et al (2021) Use of Phil embolic agent for bleeding in non-neurological interventions. J Clin Med 10(4):701
Vollherbst DF, Sommer CM, Ulfert C et al (2017) Liquid embolic agents for endovascular embolization: evaluation of an established (Onyx) and a novel (PHIL) embolic agent in an in vitro AVM model. Am J Neuroradiol 38:1377–1382
Piacentino F, Fontana F, Curti M et al (2021) Non-adhesive liquid embolic agents in extra-cranial district: state of the art and review of the literature. J Clin Med 10(21):4841
Koçer N, Hanimoglu H, Batur S et al (2016) Preliminary experience with precipitating hydrophobic injectable liquid in brain arteriovenous malformations. Diagn Interv Radiol 22(2):184–189
Samaniego EA, Kalousek V, Abdo G, Ortega-Gutierrez S (2016) Preliminary experience with precipitating hydrophobic injectable liquid (PHIL) in treating cerebral AVMs. J Neurointerv Surg 8(12):1253–1255
Lamin S, Chew HS, Chavda S et al (2017) Embolization of intracranial dural arteriovenous fistulas using PHIL liquid embolic agent in 26 patients: a multicenter study. AJNR Am J Neuroradiol 38(1):127–131
Leyon JJ, Chavda S, Thomas A, Lamin S (2016) Preliminary experience with the liquid embolic material agent PHIL (precipitating hydrophobic injectable liquid) in treating cranial and spinal dural arteriovenous fistulas: technical note. J Neurointerv Surg 8(6):596–602
Varadharajan S, Ramalingaiah AH, Saini J et al (2018) Precipitating hydrophobic injectable liquid embolization of intracranial vascular shunts: initial experience and technical note. J Neurosurg 129(5):1217–1222
Psychogios G, Berlis A, Märkl B et al (2017) Percutaneous phil™-embolization for preoperative therapy of carotid body paragangliomas. Laryngorhinootologie 96(1):22–26
Kurda D, Guduguntla G, Maingard J et al (2019) Precipitating hydrophobic injectable liquid (PHIL) embolic for the treatment of a uterine arteriovenous malformation: a technical report. CVIR Endovasc 2(1):17
Giurazza F, Corvino F, Silvestre M et al (2021) Embolization of peripheral arteriovenous malformations and fistulas with precipitating hydrophobic injectable liquid (PHIL®). Radiol Med 126(3):474–483
Lamanna A, Maingard J, Florescu G et al (2021) Endovascular balloon-assisted liquid embolisation of soft tissue vascular malformations: technical feasibility and safety. CVIR Endovasc 4(1):49
Helmy A, Shaida N (2017) Treatment of type II endoleaks with a novel agent: precipitating hydrophobic injectable liquid (PHIL). Cardiovasc Intervent Radiol 40(7):1094–1098
Prashar A, Butt S, Shaida N (2020) Introducing PHIL (precipitating hydrophobic injectable liquid): a new embolic agent for the body interventional radiologist. Diagn Interv Radiol 26:140–142
Filippiadis DK, Binkert C, Pellerin O, Hoffmann RT, Krajina A, Pereira PL (2017) CIRSE quality assurance document and standards for classification of complications: the CIRSE classification system. Cardiovasc Intervent Radiol 40:1141–1146
Giurazza F, Corvino F, Cangiano G et al (2019) Transarterial embolization of peripheral high-flow arteriovenous malformation with ethylene vinyl alcohol copolymer (Onyx ®): single-center 10-year experience. Radiol Med 124(2):154–162
Vollherbst DF, Otto R, Do T et al (2018) Imaging artifacts of onyx and PHIL on conventional CT, cone-beam CT and MRI in an animal model. Interv Neuroradiol 24(6):693–701
Schmitt N, Floca RO, Paech D et al (2021) Imaging artifacts of liquid embolic agents on conventional CT in an experimental in vitro model. AJNR Am J Neuroradiol 42(1):126–131
Raissi D, Yu Q, Mardini SH (2018) Upper gastrointestinal bleed embolization with onyx®: the “Tattoo Effect.” J Clin Imaging Sci 8:46
In’t Veld M, Willems PW (2016) Absence of skin discoloration after transarterial embolization of a subcutaneous auricular arteriovenous malformation with PHIL. Interv Neuroradiol 22(5):606–10
Smith SJ, Thomas A, Ashpole RD (2009) Intra-operative combustion of Onyx embolic material. Br J Neurosurg 23(1):76–8
Vollherbst DF, Otto R, von Deimling A (2018) Evaluation of a novel liquid embolic agent (precipitating hydrophobic injectable liquid (PHIL)) in an animal endovascular embolization model. J Neurointerv Surg 10(3):268–274
Vollherbst DF, Sommer CM, Ulfert C et al (2017) Liquid embolic agents for endovascular embolization: evaluation of an established (Onyx) and a novel (PHIL) embolic agent in an in vitro AVM model. AJNR Am J Neuroradiol 38(7):1377–1382
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent to study participation was waived due to the retrospective design.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Giurazza, F., Cionfoli, N., Paladini, A. et al. PHIL® (precipitating hydrophobic injectable liquid): retrospective multicenter experience on 178 patients in peripheral embolizations. Radiol med 127, 1303–1312 (2022). https://doi.org/10.1007/s11547-022-01552-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-022-01552-y