Abstract
Purpose
Ischaemic stroke due to occlusion of large cerebral vessels has a poor prognosis. The clinical outcome is related to efficacy and timing of recanalisation of the occluded arteries. We report our experience with a thrombus aspiration device (Penumbra), and focus on pre- and postprocedural management.
Materials and methods
We retrospectively reviewed 18 consecutive patients with acute ischaemic stroke due to the occlusion of large cerebral vessels who were treated with mechanical thrombolysis at our centre between September 2009 and July 2010. Preprocedural symptoms were quantified using the National Institutes of Health Stroke Scale (NIHSS). Mechanical thrombolysis was performed with the Penumbra system. Intravenous thrombolysis was done only if <3 h had elapsed since symptom onset. Associated vessel stenoses were treated with stenting. All patients underwent neurological examination and postprocedural magnetic resonance angiography (MRA) at 3 and 6 months.
Results
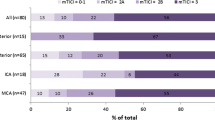
Mechanical thrombolysis using the Penumbra system was performed in all cases. A total of 83% of treated vessels had a value of 2/3 according to the Thrombolysis in Cerebral Infarction (TICI) scale. In seven patients (39%) intravenous thrombolysis was unsuccessful, and salvage mechanical thrombolysis followed. Three patients died after the procedure (16.7%). Five patients (27.8%) required a stenting procedure. All patients reported a significant improvement in symptoms (mean baseline NIHSS 19.6±5.6; mean postprocedural NIHSS, 7.8±5.5 p<0.0001)
Conclusions
Our preliminary experience with the Penumbra mechanical thrombolysis system confirms previously reported results showing the efficacy and safety of the device in treating acute stroke caused by the occlusion of large intracranial vessels.
Riassunto
Obiettivo
L’ictus ischemico dovuto ad occlusione di vasi cerebrali di grosso calibro ha una prognosi infausta. I risultati clinici sono correlati all’efficacia e tempestività della ricanalizzazione dell’arteria occlusa. Riportiamo la nostra esperienza con un dispositivo di trombo aspirazione focalizzando l’attenzione sulla gestione pre- e postprocedurale.
Materiali e metodi
Riportiamo retrospettivamente i risultati di 18 pazienti consecutivi affetti da ictus ischemico acuto dovuto ad occlusione di vasi cerebrali di grosso calibro trattati con trombolisi meccanica nel nostro centro tra settembre 2009 e luglio 2010. I sintomi pre-procedurali sono stati quantificati attraverso la National Institute of Health Stroke Scale (NHISS). La trombolisi meccanica è stata condotta utilizzando il sistema Penumbra. La trombolisi endovenosa è stata effettuata solamente laddove il tempo dall’esordio della sintomatologia fosse inferiore alle 3 ore. Le stenosi dei vasi associate sono state trattate mediante stenting. Tutti i pazienti hanno eseguito un esame neurologico ed uno studio in angio-risonanza magnetica (RM) post-procedurale a distanza di 3 e 6 mesi dal trattamento.
Risultati
La trombolisi meccanica con sistema Penumbra è stata eseguita in tutti i casi. L’83% dei vasi trattati avevano un valore di 2 su 3 nella scala di trombolisi nell’ictus cerebri (TICI). In 7 pazienti (38,8%) la trombolisi endovenosa non ha avuto successo ed una trombolisi meccanica di salvataggio è stata eseguita. Tre pazienti sono deceduti dopo la procedura (16,7%). In 5 pazienti (27,8%) una procedura di stenting è stata necessaria. In tutti i pazienti abbiamo osservato un significativo miglioramento dei sintomi (NHISS basale medio 19,6±5,6; NHISS post-procedurale medio 7,8±5,5; p<0,0001).
Conclusioni
La nostra esperienza preliminare con il sistema di trombolisi meccanica Penumbra conferma risultati precedentemente riportati, dimostrando la sua efficacia e sicurezza nel trattamento dello stroke acuto dovuto all’occlusione di vasi endocranici di grande calibro.
Similar content being viewed by others
References/Bibliografia
Alexandrov AV, Molina CA, Grotta JC et al (2004) CLOTBUST Investigators. Ultrasound-enhanced systemic thrombolysis for acute ischemic stroke. N Engl J Med 351:2170–2178
Adams HP, del Zoppo G, Alberts MJ et al (2007) Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Stroke 38:1655–1711
Penumbra Pivotal Stroke Trial Investigator (2009) The Penumbra Pivotal Stroke Trial: safety and effectiveness of a new generation of mechanical devices for clot removal in intracranial large vessel occlusive disease. Stroke 40:2161–2168
Bose A, Henkes H, Alfke K et al (2008) The Penumbra system: a mechanical device for the treatment of acute stroke due to thromboembolism. AJNR Am J Neuroradiol 29:1409–1413
Grunwald IQ, Walter S, Papanagiotou P et al (2009) Revascularization in acute ischaemic stroke using the Penumbra system: the first single center experience. Eur J Neurol 16:1210–1216
Kulcsar Z, Bonvin C, Pereira VM et al (2009) Penumbra system: a novel mechanical thrombectomy device for large-vessel occlusions in acute stroke. AJNR Am J Neuroradiol 31:628–633
Struffert T, Kohrmann M, Engelhorn T et al (2009) Penumbra stroke system as an “add-on” for the treatment of large vessel occlusive disease following thrombolysis: first results. Eur Radiol 19:2286–2293
Schaefer PW, Barak ER, Kamalian S et al (2008) Quantitative assessment of core/penumbra mismatch in acute stroke: CT and MR perfusion imaging are strongly correlated when sufficient brain volume is imaged. Stroke 29:2986–2992
Tomsick T (2007) TIMI, TIBI, TICI: I came, I saw, I got confused. AJNR Am J Neuroradiol 28:382–384
Kasner SE, Chalela JA, Luciano JM et al (1999) Reliability and validity of estimating the NIH stroke scale score from medical reports. Stroke 30:1534–1537
Bonita R, Beaglehole R (1988) Recovery of motor function after stroke. Stroke 19:1497–1500
Heuschmann PU, Berger K, Misselwitz B et al (2003) Frequency of thrombolytic therapy in patients with an acute ischemic stroke of in hospital mortality: the German Stroke Register Study Group. Stroke 34:1106–1113
Saqqur M, Molina CA, Salam A et al (2007) CLOTBUST Investigators. Clinical deterioration after intravenous recombinant tissue plasminogen activator treatment: a multicenter transcranial Doppler study. Stroke 38:69–74
The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group (1995) Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 333:1581–1587
Labiche LA, AL-Senani F, Wojner AW et al (2003) Is the benefit of early recanalization sustained at 3 months? A prospective cohort study. Stroke 34:695–698
Smith WS, Sung G, Starkman S et al (2005) Safety and efficacy of mechanical embolectomy in acute ischemic stroke: results of the Merci Trial. Stroke 36:1432–1438
Smith WS (2006) Safety of mechanical thrombectomy and intravenous tissue plasminogen activator in acute ischemic stroke. Results of the multi Mechanical Embolus Removal in Cerebral Ischemia (MERCI) trial, part I. AJNR Am J Neuroradiol 27:1177–1182
Muir KW, Weir CJ, Alwan W et al (1999) C-Reactive protein and outcome after ischemic stroke. Stroke 30:981–985
Lippi G, Favaloro EJ, Montagna M, Franchini M (2010) C-reactiv protein and venous thromboembolism: casual or casual association? Clin Chem Lab Med 48:1693–1701
Di Napoli M, Papa F; Villa Pini Stroke Data Bank Investigators (2002) Inflammation, hemostatic markers and antithrombotic agents in relation to long ternm risk of new cardiovascular events in first-ever ischemic stroke patients. Stroke 33:1763–1771
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gandini, R., Pampana, E., Del Giudice, C. et al. Acute stroke treatment using the Penumbra endovascular mechanical thrombolysis device: a single-centre experience. Radiol med 117, 1199–1214 (2012). https://doi.org/10.1007/s11547-012-0819-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-012-0819-5