Abstract
Purpose
This study compared superparamagnetic iron-oxide-enhanced magnetic resonance imaging (SPIO-MRI) and combined fluorodeoxyglucose positron emission tomography and computed tomography (FDG-PET/CT) in evaluating liver metastases from colorectal adenocarcinoma following chemotherapy.
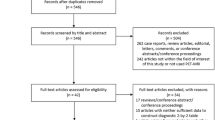
Materials and methods
Nineteen patients were included in this retrospective study. SPIO-MRI and PET/CT results were compared with surgery, intraoperative ultrasound and pathology results in 11 patients and with the follow-up in eight patients.
Results
SPIO-MRI and PET/CT identified 125 and 71 metastases, respectively. False negative lesions were 11 for SPIO-MRI and 65 for PET/CT. In the whole study population, the per-lesion analysis of SPIO-MRI and PET/CT showed a sensitivity of 92% and 52% (p<0.001) and the per-segment analysis a sensitivity of 99% and 79% (p<0.001), respectively. In patients who underwent surgery, the per-lesion analysis of SPIO-MRI and PET/CT showed a sensitivity of 85% and 58% (p<0.05) and the per-segment analysis a sensitivity of 97% and 63% (p<0.05), respectively. In patients who underwent follow-up, the per-lesion analysis of SPIO-MRI and PET/CT showed a sensitivity of 97% and 47% (p<0.001) and the per-segment analysis a sensitivity of 100% and 63% (p<0.007), respectively. For lesions ≥15 and <30mm and for lesions <15 mm, SPIO-MRI demonstrated a higher sensitivity than PET/CT (p<0.001).
Conclusions
SPIO-MRI appears superior to PET/CT in evaluating liver metastases from colorectal adenocarcinoma following chemotherapy.
Riassunto
Obiettivo
Scopo del presente lavoro è stato confrontare la superparamagnetic iron oxid-risonanza magnetica (SPIORM) e la tomografia computerizzata associata a tomografia a emissione di positroni con fluorodesossiglucosio (TC-PET-FDG) nella valutazione delle metastasi epatiche di adenocarcinoma colorettale dopo chemioterapia.
Materiali e metodi
Diciannove pazienti sono stati inclusi in questo studio. I risultati della SPIO-RM e della TC-PET sono stati confrontati con la chirurgia, l’ecografia intraoperatoria e l’anatomia patologica in 11 pazienti; con il follow-up in 8 pazienti.
Risultati
La SPIO-RM e la TC-PET hanno individuato 125 e 71 metastasi rispettivamente (falsi negativi: 11 e 65 rispettivamente). Considerando tutti i pazienti: analisi per lesione sensibilità del 92% per SPIO-RM e del 52% per TC-PET (p<0,001), analisi per segmento epatico sensibilità del 99% e del 79% (p<0,001) rispettivamente. Nei pazienti operati: analisi per lesione sensibilità del 85% per SPIO-RM e del 58% per TC-PET (p<0,05), analisi per segmento epatico sensibilità del 97% e del 63% (p<0,05) rispettivamente. Nei pazienti non operati in follow-up: analisi per lesione sensibilità del 97% per SPIO-RM e del 47% per TC-PET (p<0,001), analisi per segmento epatico sensibilità del 100% e del 63% (p<0,007) rispettivamente. La SPIO-RM ha dimostrato una sensibilità superiore alla TC-PET-FDG nella valutazione delle lesioni comprese tra 15 e 30 mm e delle lesioni <15 mm (p<0,001).
Conclusioni
La SPIO-RM appare superiore alla TC-PET nella valutazione delle metastasi epatiche dopo chemioterapia
Similar content being viewed by others
References/Bibliografia
Weitz J, Koch M, Debus J et al (2005) Colorectal cancer. Lancet 365:153–165
Penna C, Nordlinger B (2002) Colorectal metastasis (liver and lung). Surg Clin N Am 82:1075–1090
Stangl R, Altendorf-Hofmann A, Charnley RM, Scheele J (1994) Factors influencing the natural history of colorectal liver metastases. Lancet 343:1405–1410
Tomizawa N, Ohwada S, Ogawa T et al (2006) Factors affecting the prognosis of anatomical liver resection for liver metastases from colorectal cancer. Hepatogastroenterology 53:89–93
Vauthey JN, Zorzi D, Pawlik TM (2005) Making Unresectable Hepatic Colorectal Metastases Resectable-Does It Work? Semin Oncol 32:S118–S122
Kinkel K, Lu Y, Both M et al (2002) Detection of hepatic metastases from cancers of the gastrointestinal tract by using noninvasive imaging methods (US, CT, MR imaging, PET): a metaanalysis. Radiology 224:748–756
Schima W, Kulinna C, Langenberger H, Ba-Ssalamah A (2005) Liver metastases of colorectal cancer: US, CT or MR? Cancer Imaging 23:S149–S156
Semelka RC, Cance WG, Marcos HB, Mauro MA (1999) Liver metastases: comparison of current MR techniques and spiral CT during arterial portography for detection in 20 surgically staged cases. Radiology 213:86–91
Ward J, Robinson PJ, Guthrie JA, et al (2005) Liver Metastases in Candidates for Hepatic Resection: Comparison of Helical CT and Gadolinium- and SPIO enhanced MR Imaging. Radiology 237:170–180
Kim YK, Ko SW, Hwang SB et al (2006) Detection and characterization of liver metastases: 16-slice multidetector computed tomography versus superparamagnetic iron oxide-enhanced magnetic resonance imaging. Eur Radiol 16:1337–1345
Kim MJ, Kim JH, Lim JS et al (2004) Detection and characterization of focal hepatic lesions: mangafodipir vs. superparamagnetic iron oxide-enhanced magnetic resonance imaging. J Magn Reson Imaging 20:612–621
Wiering B, Krabbe PF, Jager GJ et al (2005) The impact of fluor-18-deoxyglucose-positron emission tomography in the management of colorectal liver metastases. Cancer 104:2658–2670
Bipat S, van Leeuwen MS, Comans EF et al (2005) Colorectal Liver Metastases: CT, MR Imaging, and PET for Diagnosis-Meta-analysis. Radiology 237:123–131
Sahani DV, Kalva SP, Fischman AJ et al (2005) Detection of liver metastases from adenocarcinoma of the colon and pancreas: comparison of mangafodipir trisodium-enhanced liver MRI and whole-body FDG PET. AJR Am J Roentgenol 185:239–246
Strotzer M, Gmeinwieser J, Schmidt J et al (1997) Diagnosis of liver metastases from colorectal adenocarcinoma. Comparison of spiral-CTAP combined with intravenous contrast-enhanced spiral-CT and SPIO-enhanced MR combined with plain MR imaging. Acta Radiol 38:986–992
Kim YK, Lee JM, Kim CS et al (2005) Detection of liver metastases: gadobenate dimeglumine-enhanced three-dimensional dynamic phases and one-hour delayed phase MR imaging versus superparamagnetic iron oxide-enhanced MR imaging. Eur Radiol 15:220–228
Vogl TJ, Schwarz W, Blume S et al (2003) Preoperative evaluation of malignant liver tumors: comparison of unenhanced and SPIO (Resovist)-enhanced MR imaging with biphasic CTAP and intraoperative US. Eur Radiol 13:262–272
Conlon R, Jacobs M, Dasgupta D, Lodge JP (2003) The value of intraoperative ultrasound during hepatic resection compared with improved preoperative magnetic resonance imaging. Eur J Ultrasound 16:211–216
Del Frate C, Bazzocchi M, Mortele KJ et al (2002) Detection of liver metastases: comparison of gadobenate dimeglumine-enhanced and ferumoxides-enhanced MR imaging examinations. Radiology 225:766–772
Furuhata T, Okita K, Tsuruma T et al (2003) Efficacy of SPIO-MR imaging in the diagnosis of liver metastases from colorectal carcinomas. Dig Surg 20:321–325
Kim MJ, Kim JH, Choi JY et al (2006) Optimal TE for SPIO-enhanced gradient-recalled echo MRI for the detection of focal hepatic lesions. AJR Am J Roentgenol 187:255–266
Mawlawi O, Erasmus JJ, Munden RF et al (2006) Quantifying the effect of IV contrast media on integrated PET/CT: clinical evaluation. AJR Am J Roentgenol 186:308–319
Rappeport ED, Loft A, Berthelsen AK et al (2007) Contrast-enhanced FDGPET/ CT vs. SPIO-enhanced MRI vs. FDG-PET vs. CT in patients with liver metastases from colorectal cancer: a prospective study with intraoperative confirmation. Acta Radiol 48:369–378
Orlacchio A, Schillaci O, Fusco N et al (2009) Role of PET/CT in the detection of liver metastases from colorectal cancer. Radiol Med 114:571–585
Onishi H, Murakami T, Kim T et al (2006) Hepatic metastases: detection with multi-detector row CT, SPIO-enhanced MR imaging, and both techniques combined. Radiology 239:131–138
Leen E, Ceccotti P, Moug SJ et al (2006) Potential value of contrast-enhanced intraoperative ultrasonography during partial hepatectomy for metastases: an essential investigation before resection? Ann Surg 243:236–240
Ward J, Guthrie JA, Wilson D et al (2003) Colorectal hepatic metastases: detection with SPIO-enhanced breath-hold MR imaging-Comparison of optimized sequences. Radiology 228:709–718
Erturk SM, Ichikawa T, Fujii H et al (2006) PET imaging for evaluation of metastatic colorectal cancer of the liver. Eur J Radiol 58:229–235
Kim HJ, Kim KW, Byun JH et al (2006) Comparison of mangafodipir trisodium- and ferucarbotran-enhanced MRI for detection and characterization of hepatic metastases in colorectal cancer patients. AJR Am J Roentgenol 186:1059–1066
Akhurst T, Kates TJ, Mazumdar M et al (2005) Recent chemotherapy reduces the sensitivity of [18F] fluorodeoxyglucose positron emission tomography in the detection of colorectal metastases. J Clin Oncol 23:8713–8716
Goshen E, Davidson T, Zwas ST, Aderka D (2006) PET/CT in the evaluation of response to treatment of liver metastases from colorectal cancer with bevacizumab and irinotecan. Technol Cancer Res Treat 5:37–43
Wiering B, Krabbe PF, Dekker HM et al (2007) The role of FDG-PET in the selection of patients with colorectal liver metastases. Ann Surg Oncol 14:771–779
Patrikeos A, Breidahl W, Robins P (2005) F-18 FDG uptake associated with elastofibroma dorsi. Clin Nucl Med 30:617–618
Pierce JC 3rd, Henderson R (2004) Hypermetabolism of elastofibroma dorsi on PET-CT. AJR Am J Roentgenol 183:35–37
Israel O, Yefremov N, Bar-Shalom R et al (2005) PET/CT detection of unexpected gastrointestinal foci of 18FFDG uptake: incidence, localization patterns, and clinical significance. J Nucl Med 46:758–762
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bacigalupo, L., Aufort, S., Eberlé, M.C. et al. Assessment of liver metastases from colorectal adenocarcinoma following chemotherapy: SPIO-MRI versus FDG-PET/CT. Radiol med 115, 1087–1100 (2010). https://doi.org/10.1007/s11547-010-0560-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-010-0560-x