Abstract
Purpose
We evaluated the reliability of stereotactic vacuum-assisted breast biopsies (VAB) from our personal experience.
Materials and methods
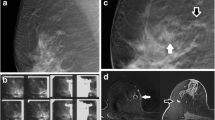
Between January 2003 and December 2005, 268 patients underwent VAB with an 11-gauge probe at our institution. Inclusion criteria were nonpalpable lesions, undetectable by ultrasound and suspected at mammography (microcalcifications, circumscribed mass, architectural distortion), for which cytology and/or core biopsy could not provide a definite diagnosis. Lesion mammographic patterns were microcalcifications in 186 cases (77.5%), mostly localised clusters (130/186: 70%); circumscribed mass with or without microcalcifications in 36 cases (15%) and architectural distortion with or without microcalcifications in 18 cases (7.5%). On the basis of the Breast Imaging Reporting and Data System (BI-RADS) classification, 16 cases (7%) were graded as highly suspicious for malignancy (BI-RADS 5), 81 (34%) as suspicious for malignancy (BI-RADS 4b), 97 (40%) as indeterminate (BI-RADS 4a) and 46 (19%) as probably benign (BI-RADS 3). Lesion size was ≤10 mm in 161 cases (67%) and > 20 mm in only 38 cases (16%), 30 of which appeared as microcalcifications.
Results
In 28/268 lesions (10.5%) the biopsy could not be performed (nonidentification of the lesion; inaccessibility due to location or breast size). In 12/240 (5%) biopsies, the sample was not representative. Pathology releaved 100/240 (42%) malignant or borderline lesions and 140/240 (58%) benign lesions. Among the malignant lesions, 16/100 (16%) were invasive carcinoma [infiltrating ductal carcinoma (IDC) or infiltrating lobular carcinoma (ILC)], 13/100 (13%) were microinvasive (T1mic), 35/100 (35%) were ductal carcinoma in situ (DCIS), 9/100 (9%) were lobular carcinoma in situ (CLIS). Among the borderline lesions, 27/100 (27%) were atypical epithelial hyperplasia [atypical ductal hyperplasia (ADH) or atypical lobular hyperplasia (ALH)]. In 9/100 surgically treated lesions (9%), there was discordance between the microhistological findings of VAB and the pathological results of the surgical procedure: 8/9 were underestimated by VAB (four ADH vs. DCIS, three DCIS vs. IDC, one ADH vs. IDC), and 1/9 was overestimated (T1mic vs. DCIS). Complications following VAB occurred in 9/240 patients (3.7%).
Conclusions
In our experience, VAB showed fair reliability in the diagnosis of nonpalpable breast lesions despite a portion of failed (10.5%), nonsignificant (5%) procedures and underestimated lesions (9%).
Riassunto
Obiettivo
Valutare l’accuratezza del sistema di agobiopsia mammaria in stereotassi con metodica multidirezionale e dispositivo aspirante sotto vuoto (VAB) nell’esperienza personale, al fine di dimostrare la validità di questa metodica.
Materiali e metodi
Nel periodo compreso fra gennaio 2003 e dicembre 2005, 268 pazienti sono state sottoposte a manovra ago-bioptica con VAB utilizzando ago 11-gauge. Sono state avviate al VAB tutte le pazienti con alterazioni sospette alla mammografia, non riconoscibili con ecografia, non palpabili (focolai di microcalcificazioni, minuscole lesioni focali con o senza microcalcificazioni, aspetti di sovvertimento) in cui la tipizzazione non poteva essere ottenuta con metodiche alternative (citologia e/o core-biopsy) e non si riteneva opportuno il follow-up. L’aspetto radiologico delle lesioni è stato di microcalcificazioni in 186 casi (77,5%), per lo più distribuite in unico focolaio (130/186: 70%); opacità focale con o senza microcalcificazioni in 36 casi (15%), infine, in 18 casi (7,5%) distorsione, con o senza microcalcificazioni. Utilizzando la classificazione BIRADS il giudizio radiologico è stato “altamente sospetto” di malignità (BIRADS 5) in 16 casi (7%), “sospetto” di malignità (BI-RADS 4b) in 81 casi (34%), “indeterminato” (BI-RADS 4a) in 97 casi (40%) e “probabilmente benigno” (BI-RADS 3) in 46 casi (19%). Centosessantuno lesioni (67%) avevano diametro ≤10 mm; solo 38 lesioni (16%) erano >20 mm,la maggior parte di queste, 30 casi, si manifestavano alla mammografia sotto forma di microcalcificazioni.
Risultati
In 28/268 casi (10,5%) non è stato possibile procedure al prelievo (mancata visualizzazione della lesione, inaccessibilità al bersaglio per sede della lesione o ridotto spessore della mammella). Il campione è risultato non significativo in 12/240 procedure espletate (5%). Il riscontro di patologia francamente maligna o di lesioni border-line si è verificato nel 42% dei casi (100/240), nei restanti 140 casi (58%) si è rilevata patologia benigna. Fra le lesioni maligne, è stata posta diagnosi di carcinoma infiltrante (CDI e CLI) in 16 casi (16/100: 16%), di carcinoma microinfiltrante (T1mic) in 13 casi (13/100: 13%), di carcinoma duttale in situ (CDIS) in 35 casi (35/100: 35%); di carcinoma lobulare in situ (CLIS) in 9 casi (9/100: 9%) e di iperplasia epiteliale atipica (ADH e ALH) in 27 casi (27/100:27%). In 9/100 lesioni (9%) si è avuta discordanza fra i reperti microistologici del VAB e i risultati patologici delle procedure chirurgiche: 8/9 sono state sottostimate dal VAB (4 ADH vs CDIS, 3 CDIS vs CDI, 1 ADH vs CDI) e 1/9 è stata sovrastimata (T1mic vs CDIS). La comparsa di complicanze in seguito a manovra bioptica con VAB si è verificata in 9/240 pazienti (3,7%).
Conclusioni
Il prelievo con VAB è risultato essere nella esperienza personale metodica discretamente affidabile nella tipizzazione di lesioni mammarie non palpabili, seppur gravata da una quota di procedure mancate (10,5%), di campionamenti non significativi (5%), ed infine da lesioni sottostimate (9%).
Similar content being viewed by others
References/Bibliografia
Ciatto S, Cataliotti L, Distante V (1987) Nonpalpable lesions detected with mammography: review of 512 consecutive cases. Radiology 165:99–102
Meyer JE, Kopans DB, Stomper PC et al (1984) Occult breast abnormalities: percutaneous preoperative needle localization. Radiology 150:335–337
Kopans DB (1992) The positive predictive value of mammography. AJR Am J Roentgenol 158:521–526
Ciatto S, Rosselli Del Turco M, Ambrogetti D et al (1997) Solid nonpalpable breast lesions. Success and failure of guided fine-needle aspiration cytology in a consecutive series of 2444 cases. Acta Radiol 38:815–820
Leifland K, Lagerstedt U, Svane G (2003) Comparison of stereotactic fine needle aspiration cytology and core needle biopsy in 522 nonpalpable breast lesions. Acta Radiol 44:387–391
Parker SH, Burbank F, Jackman RJ et al (1994) Percutaneous large-core breast biopsy: a multi-institutional study. Radiology 193:359–364
Liberman L, Dershaw DD, Glassman JR et al (1997) Analysis of cancers not diagnosed at stereotactic core breast biopsy. Radiology 203:151–157
Liberman L, Sama MP (2000) Costeffectiveness of stereotactic 11-gauge directional vacuum-assisted breast biopsy. AJR Am J Roentgenol 175:53–58
Burbank F (1997) Stereotactic breast biopsy of atypical ductal hyperplasia and ductal carcinoma in situ lesions: improved accuracy with directional, vacuum-assisted biopsy. Radiology 202:843–847
Dhillon MS, Bradley SA, England DW (2006) Mammotome biopsy: impact on preoperative diagnosis rate. Clin Radiol 61:276–281
Kettritz U, Morack G, Decker T (2004) Stereotactic vacuum-assisted breast biopsies in 500 women with microcalcifications: radiological and pathological correlations. Eur J Radiol 55:270–276
Orel SG, Kay N, Reynolds C et al (1999) BI-RADS categorization as a predictor of malignancy. Radiology 211:845–850
Parker SH, Klaus AJ (1997) Performing a breast biopsy with a directional, vacuum-assisted biopsy instrument. Radiographics 17:1233–1252
Heywang-Kobrunner SH, Schaumloffel U, Viehweg P et al (1998) Minimally invasive stereotaxic vacuum core breast biopsy. Eur Radiol 8:377–385
Della Sala SW, Pellegrini M, Bernardi D et al (2004) Advantages and limits of percutaneous breast core biopsy with Mammotome and stereotactic equipment in upright seated patient. Radiol Med 108:335–344
Cangiarella J, Waisman J, Symmans WF et al (2001) Mammotome core biopsy for mammary microcalcification: analysis of 160 biopsies from 142 women with surgical and radiologic followup. Cancer 91:173–177
Jackman RJ, Nowels KW, Rodriguez-Soto J, et al (1999) Stereotactic, automated, large-core needle biopsy of nonpalpable breast lesions: false-negative and histologic underestimation rates after long-term follow-up. Radiology 210:799–805
Philpotts LE, Shaheen NA, Carter D et al (1999) Comparison of rebiopsy rates after stereotactic core needle biopsy of the breast with 11-gauge vacuum suction probe versus 14-gauge needle and automatic gun. AJR Am J Roentgenol 172:683–687
Kettritz U, Rotter K, Schreer I et al (2004) Stereotactic vacuum-assisted breast biopsy in 2874 patients: a multicenter study. Cancer 100:245–251
Giardina C, Guerrieri AM, Ingravallo G et al (2002) The stereotaxic core breast biopsy using the Mammotome: an alternative to intraoperative examination. Pathologica 94:182–189
Philpotts LE, Lee CH, Horvath LJ et al (1997) Canceled stereotactic core-needle biopsy of the breast: analysis of 89 cases. Radiology 205:423–428
Liberman L, Smolkin JH, Dershaw DD et al (1998) Calcification retrieval at stereotactic, 11-gauge, directional, vacuum-assisted breast biopsy. Radiology 208:251–260
Ciatto S, Houssami N, Ambrogetti D et al (2006) Accuracy and underestimation of malignancy of breast core needle biopsy: the Florence experience of over 4000 consecutive biopsies. Breast Cancer Res Treat 2006 101:291–297
Brenner RJ, Fajardo L, Fisher PR et al (1996) Percutaneous core biopsy of the breast: effect of operator experience and number of samples on diagnostic accuracy. AJR Am J Roentgenol 166:341–346
Meyer JE, Smith DN, DiPiro PJ et al (1997) Stereotactic breast biopsy of clustered microcalcifications with a directional, vacuum-assisted device. Radiology 204:575–576
Apesteguia L, Mellado M, Saenz J et al (2002) Vacuum-assisted breast biopsy on digital stereotaxic table of nonpalpable lesions non-recognisable by ultrasonography. Eur Radiol 12:638–645
Won B, Reynolds HE, Lazaridis CL et al (1999) Stereotactic biopsy of ductal carcinoma in situ of the breast using an 11-gauge vacuum-assisted device: persistent underestimation of disease. AJR Am J Roentgenol 173:227–229
Jackman RJ, Birdwell RL, Ikeda DM (2002) Atypical ductal hyperplasia: can some lesions be defined as probably benign after stereotactic 11-gauge vacuum-assisted biopsy, eliminating the recommendation for surgical excision? Radiology 224:548–554
Brenner RJ, Bassett LW, Fajardo LL et al (2001) Stereotactic core-needle breast biopsy: a multi-institutional prospective trial. Radiology 218:866–872
Liberman L, Abramson AF, Squires FB et al (1998) The breast imaging reporting and data system: positive predictive value of mammographic features and final assessment categories. AJR Am J Roentgenol 171:35–40
Meyer JE, Smith DN, Lester SC et al (1999) Large-core needle biopsy of nonpalpable breast lesions. JAMA 281:1638–1641
Darling ML, Smith DN, Lester SC et al (2000) Atypical ductal hyperplasia and ductal carcinoma in situ as revealed by large-core needle breast biopsy: results of surgical excision. AJR Am J Roentgenol 175:1341–1346
Brem RF, Behrndt VS, Sanow L et al (1999) Atypical ductal hyperplasia: histologic underestimation of carcinoma in tissue harvested from impalpable breast lesions using 11-gauge stereotactically guided directional vacuum-assisted biopsy. AJR Am J Roentgenol 172:1405–1407
Jackman RJ, Burbank F, Parker SH et al (2001) Stereotactic breast biopsy of nonpalpable lesions: determinants of ductal carcinoma in situ underestimation rates. Radiology 218:497–450
Jackman RJ, Rodriguez-Soto J (2006) Breast microcalcifications: retrieval failure at prone stereotactic core and vacuum breast biopsy-frequency, causes, and outcome. Radiology 239:61–70
Burbank F (1997) Stereotactic breast biopsy: comparison of 14-and 11-gauge Mammotome probe performance and complication rates. Am Surg 63:988–995
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tonegutti, M., Girardi, V. Stereotactic vacuum-assisted breast biopsy in 268 nonpalpable lesions. Radiol med 113, 65–75 (2008). https://doi.org/10.1007/s11547-008-0226-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-008-0226-0