Abstract
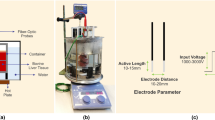
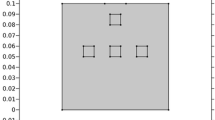
Radiofrequency ablation is a nominally invasive technique to eradicate cancerous or non-cancerous cells by heating. However, it is still hampered to acquire a successful cell destruction process due to inappropriate RF intensities that will not entirely obliterate tumorous tissues, causing in treatment failure. In this study, we are acquainted with a nanoassisted RF ablation procedure of cardiac tumor to provide better outcomes for long-term survival rate without any recurrences. A three-dimensional thermo-electric energy model is employed to investigate nanothermal field and ablation efficiency into the left atrium tumor. The cell death model is adopted to quantify the degree of tissue injury while injecting the Fe3O4 nanoparticles concentrations up to 20% into the target tissue. The results reveal that when nanothermal field extents as a function of tissue depth (10 mm) from the electrode tip, the increasing thermal rates were approximately 0.54362%, 3.17039%, and 7.27397% for the particle concentration levels of 7%, 10%, and 15% compared with no-particle case. In the 7% Fe3O4 nanoparticles, 100% fractional damage index is achieved after ablation time of 18 s whereas tissue annihilation approach proceeds longer to complete for no-particle case. The outcomes indicate that injecting nanoparticles may lessen ablation time in surgeries and prevent damage to adjacent healthy tissue.
Graphical Abstract













Similar content being viewed by others
Change history
21 February 2024
A Correction to this paper has been published: https://doi.org/10.1007/s11517-024-03040-z
Abbreviations
- \(\theta\) (°C):
-
Temperature
- t (s):
-
Time
- c (J kg−1 °C−1):
-
Specific heat
- k (W m−1 °C−1):
-
Thermal conductivity
- \({q}_{RF}\) (W m−3):
-
Volumetric heat source
- \({Q}_{m}\) (W m−3):
-
Metabolic heat source
- J (A m−2):
-
Electric current density
- \({J}_{e}\) (A m−2):
-
External electric current density
- E (V m−1):
-
Electric field intensity
- V (V):
-
Electric potential
- (x, y, z):
-
Cartesian coordinate system
- ρ (kg m−3):
-
Tissue density
- ρ b (kg m−3):
-
Blood density
- \({\omega }_{b}({s}^{-1})\) :
-
Blood perfusion rate
- \({\omega }_{b0}({s}^{-1})\) :
-
Constant blood perfusion of tissue/tumor
- \(\alpha (t)\) :
-
Cumulative tissue damage
- \({\Omega }_{d}\) :
-
Fraction of necrotic tissue
- \(\sigma (S\ {m}^{-1})\) :
-
Electrical conductivity
- \(\eta\) :
-
Particle volume fractions
- b:
-
Blood
- eff:
-
Effective
- max:
-
Maximum
References
Berjano EJ (2006) Theoretical modeling for radiofrequency ablation: state-of-the-art and challenges for the future. Biomed Eng Online 5:1–17
Singh S, Melnik R (2020) Thermal ablation of biological tissues in disease treatment: a review of computational models and future directions. Electromagn Biol Med 39:49–88
Munshi A (2021) Ablative radiosurgery for cardiac arrhythmias–a systematic review. Cancer/Radiothérapie 25:373–379
Luo M, Jiang H, Shi T (2022) Multi-stage puncture path planning algorithm of ablation needles for percutaneous radiofrequency ablation of liver tumors. Comput Biol Med 145:105506
Possebon R, Jiang Y, Mulier S, Wang C, Chen F, Feng Y, Ni Y (2018) A piecewise function of resistivity of liver: determining parameters with finite element analysis of radiofrequency ablation. Med Biol Eng Compu 56:385–394
Park MJ, Kim YS, Rhim H, Lim HK, Lee MW, Choi D (2011) A comparison of US-guided percutaneous radiofrequency ablation of medium-sized hepatocellular carcinoma with a cluster electrode or a single electrode with a multiple overlapping ablation technique. J Vasc Interv Radiol 22:771–779
Chen MH, Yang W, Yan K, Gao W, Dai Y, Wang YB, Zhang XP, Yin SS (2005) Treatment efficacy of radiofrequency ablation of 338 patients with hepatic malignant tumor and the relevant complications. World J Gastroenterol 11:6395–6401
Zhang B, Moser MAJ, Zhang EM, Luo Y, Liu C, Zhang W (2016) A review of radiofrequency ablation: large target tissue necrosis and mathematical modelling. Physica Med 32:961–971
Hossain SMC, Ferdows M, Alam MS, Bangalee MZI, Memon K, Islam MS, Zhao G (2021) Two-phase flow model based bubble packing algorithm for optimization of multiprobe cryosurgery. Int Commun Heat Mass Transfer 127:105515
Zhang X, Hossain SMC, Wang Q, Qiu B, Zhao G (2019) Two-phase flow and heat transfer in a self-developed MRI compatible LN2 cryoprobe and its experimental evaluation. Int J Heat Mass Transf 136:709–718
Pérez JJ, Nadal E, Berjano E, González-Suárez A (2022) Computer modeling of radiofrequency cardiac ablation including heartbeat-induced electrode displacement. Comput Biol Med 144:105346
Zhang X, Chapal Hossain SM, Zhao G, Qiu B, He X (2018) Two-phase heat transfer model for multiprobe cryosurgery. Appl Therm Eng 113(2017):47–57
Hossain SMC, Zhang X, Haider Z, Hu P, Zhao G (2018) Optimization of prostatic cryosurgery with multi-cryoprobe based on refrigerant flow. J Therm Biol 76:58–67
Chen Y-C, Tu Y-K, Tsai Y-J, Tsai Y-P, Hsiao C-K (2022) Local thermal effect of power-on setting on monopolar coagulation: a three-dimensional electrothermal coupled finite element study. Med Biol Eng Compu 60:3525–3538
Satish V, Repaka R (2023) Microwave ablation trocar for ablating cancerous tumors: a numerical analysis. Med Biol Eng Compu 61:1113–1131
Tyebally S, Chen D, Bhattacharyya S, Mughrabi A, Hussain Z, Manisty C, Westwood M, Ghosh AK, Guha A (2020) Cardiac Tumors: JACC CardioOncology State-of-the-Art Review. JACC CardioOncol 2:293–311
Bussani R, Castrichini M, Restivo L, Fabris E, Porcari A, Ferro F, Pivetta A, Korcova R, Cappelletto C, Manca P, Nuzzi V, Bessi R, Pagura L, Massa L, Sinagra G (2020) Cardiac tumors: diagnosis, prognosis, and treatment. Curr Cardiol Rep 22:169
Basso C, Rizzo S, Valente M, Thiene G (2016) Cardiac masses and tumours. Heart 102:1230–1245
Zaltieri M, Massaroni C, Cauti FM, Schena E (2021) Techniques for temperature monitoring of myocardial tissue undergoing radiofrequency ablation treatments: an overview. Sensors 21:1453
Irastorza RM, d’Avila A, Berjano E (2018) Thermal latency adds to lesion depth after application of high-power short-duration radiofrequency energy: Results of a computer-modeling study. J Cardiovasc Electrophysiol 29:322–327
Pérez JJ, D’Avila A, Aryana A, Berjano E (2015) Electrical and thermal effects of esophageal temperature probes on radiofrequency catheter ablation of atrial fibrillation: results from a computational modeling study. J Cardiovasc Electrophysiol 26:556–564
Pérez JJ, González-Suárez A, Berjano E (2018) Numerical analysis of thermal impact of intramyocardial capillary blood flow during radiofrequency cardiac ablation. Int J Hyperthermia 34:243–249
Ooi EH, Lee KW, Yap S, Khattab MA, Liao IY, Ooi ET, Foo JJ, Nair SR, Mohd Ali AF (2019) The effects of electrical and thermal boundary condition on the simulation of radiofrequency ablation of liver cancer for tumours located near to the liver boundary. Comput Biol Med 106:12–23
Shao YL, Arjun B, Leo HL, Chua KJ (2017) A computational theoretical model for radiofrequency ablation of tumor with complex vascularization. Comput Biol Med 89:282–292
A. González-Suárez, J.J. Pérez, R.M. Irastorza, A. D'Avila, E. Berjano (2021) Computer modeling of radiofrequency cardiac ablation: 30 years of bioengineering research. Comput Methods Programs Biomed 106546
Romero-Méndez R, Berjano E (2017) An analytical solution for radiofrequency ablation with a cooled cylindrical electrode. Math Probl Eng 2017:9021616
Tofig BJ, Lukac P, Nielsen JM, Hansen ESS, Tougaard RS, Jensen HK, Nielsen JC, Kristiansen SB (2019) Radiofrequency ablation lesions in low-, intermediate-, and normal-voltage myocardium: an in vivo study in a porcine heart model. Europace 21:1919–1927
Yan S, Gu K, Wu X, Wang W (2020) Computer simulation study on the effect of electrode–tissue contact force on thermal lesion size in cardiac radiofrequency ablation. Int J Hyperth 37:37–48
Gu K, Yan S, Wu X (2022) Effect of anisotropy in myocardial electrical conductivity on lesion characteristics during radiofrequency cardiac ablation: a numerical study. Int J Hyperthermia 39:120–133
A Petras, Z Moreno Weidmann, M Echeverria Ferrero, M Leoni, JM Guerra, L Gerardo-Giorda (2022) Impact of the electrode tip shape on catheter performance in cardiac radiofrequency ablation. Heart Rhythm O2
Sánchez-Muñoz EJ, Berjano E, González-Suárez A (2022) Computer simulations of consecutive radiofrequency pulses applied at the same point during cardiac catheter ablation: Implications for lesion size and risk of overheating. Comput Methods Programs Biomed 220:106817
Glazer ES, Curley SA (2011) Non-invasive radiofrequency ablation of malignancies mediated by quantum dots, gold nanoparticles and carbon nanotubes. Ther Deliv 2:1325–1330
Shenoi MM, Shah NB, Griffin RJ, Vercellotti GM, Bischof JC (2011) Nanoparticle preconditioning for enhanced thermal therapies in cancer. Nanomedicine 6:545–563
Hossain SMC, Ferdows M, Bangalee MZI, Alam MS (2022) Two-phase bio-nanofluid flow through a bifurcated artery with magnetic field interaction. Int J Thermofluids 15:100194
Hossain SMC, Zhang X, Liu Z, Haider Z, Memon K, Panhwar F, Mbogba MK, Hu P, Zhao G (2018) Evaluation effect of magnetic field on nanofluid flow through a deformable bifurcated arterial network. Int Commun Heat Mass Transfer 98:239–247
Singh M, Ma R, Zhu L (2021) Theoretical evaluation of enhanced gold nanoparticle delivery to PC3 tumors due to increased hydraulic conductivity or recovered lymphatic function after mild whole body hyperthermia. Med Biol Eng Compu 59:301–313
Moran CH, Wainerdi SM, Cherukuri TK, Kittrell C, Wiley BJ, Nicholas NW, Curley SA, Kanzius JS, Cherukuri P (2009) Size-dependent joule heating of gold nanoparticles using capacitively coupled radiofrequency fields. Nano Res 2:400–405
Elliott AM, Shetty AM, Wang J, Hazle JD, Stafford RJ (2010) Use of gold nanoshells to constrain and enhance laser thermal therapy of metastatic liver tumours. Int J Hyperthermia 26:434–440
Tamarov KP, Osminkina LA, Zinovyev SV, Maximova KA, Kargina JV, Gongalsky MB, Ryabchikov Y, Al-Kattan A, Sviridov AP, Sentis M, Ivanov AV, Nikiforov VN, Kabashin AV, Timoshenko VY (2014) Radio frequency radiation-induced hyperthermia using Si nanoparticle-based sensitizers for mild cancer therapy. Sci Rep 4:7034
DT Nguyen, WS Tzou, L Zheng, W Barham, JL Schuller, B Shillinglaw, RA Quaife, WH Sauer (2016) Enhanced radiofrequency ablation with magnetically directed metallic nanoparticles. Circ Arrhythm Electrophysiol 9
Alvarez SS, Huerta LFE, Vargas AV, López J, Silva JG, González CA (2016) Characterization of breast cancer radiofrequency ablation assisted with magnetic nanoparticles: in silico and in vitro study. J Electromagn Anal Appl 8:1–7
McWilliams BT, Wang H, Binns VJ, Curto S, Bossmann SH, Prakash P (2017) Experimental investigation of magnetic nanoparticle-enhanced microwave hyperthermia. J Funct Biomater 8:21
García-Jimeno S, Ortega-Palacios R, Cepeda-Rubio MF, Vera A, Leija-Salas L, Estelrich J (2012) Improved thermal ablation efficacy using magnetic nanoparticles: a study in tumor phantoms. Progress Electromagn Res 128:229–248
Tang Y, Flesch RC, Jin T (2017) Numerical investigation of temperature field in magnetic hyperthermia considering mass transfer and diffusion in interstitial tissue. J Phys D Appl Phys 51:035401
Shao YL, Arjun B, Leo HL, Chua KJ (2017) Nano-assisted radiofrequency ablation of clinically extracted irregularly-shaped liver tumors. J Therm Biol 66:101–113
Beyk J, Tavakoli H (2019) Selective radiofrequency ablation of tumor by magnetically targeting of multifunctional iron oxide-gold nanohybrid. J Cancer Res Clin Oncol 145:2199–2209
Yue K, Yu C, Lei Q, Luo Y, Zhang X (2014) Numerical simulation of effect of vessel bifurcation on heat transfer in the magnetic fluid hyperthermia. Appl Therm Eng 69:11–18
Kandala SK, Liapi E, Whitcomb LL, Attaluri A, Ivkov R (2019) Temperature-controlled power modulation compensates for heterogeneous nanoparticle distributions: a computational optimization analysis for magnetic hyperthermia. Int J Hyperthermia 36:115–129
Sadeghi-Goughari M, Jeon S, Kwon H-J (2020) Magnetic nanoparticles-enhanced focused ultrasound heating: size effect, mechanism, and performance analysis. Nanotechnology 31:245101
Cheong JKK, Popov V, Alchera E, Locatelli I, Alfano M, Menichetti L, Armanetti P, Maturi M, Franchini MC, Ooi EH, Chiew YS (2021) A numerical study to investigate the effects of tumour position on the treatment of bladder cancer in mice using gold nanorods assisted photothermal ablation. Comput Biol Med 138:104881
Pefanis G, Maniotis N, Tsiapla A-R, Makridis A, Samaras T, Angelakeris M (2022) Numerical simulation of temperature variations during the application of safety protocols in magnetic particle hyperthermia. Nanomaterials 12:554
Manthe RL, Foy SP, Krishnamurthy N, Sharma B, Labhasetwar V (2010) Tumor Ablation and nanotechnology. Mol Pharm 7:1880–1898
Chen D, Tang Q, Li X, Zhou X, Zang J, Xue WQ, Xiang JY, Guo CQ (2012) Biocompatibility of magnetic Fe3O4 nanoparticles and their cytotoxic effect on MCF-7 cells. Int J Nanomedicine 7:4973–4982
Y Stasiuk, V Maksymenko, M Sychyk (2020) Mathematical modeling of radiofrequency ablation during open-heart surgery. Arch Electr Eng 423–431–423–431
González-Suárez A, Trujillo M, Burdío F, Andaluz A, Berjano E (2014) Could the heat sink effect of blood flow inside large vessels protect the vessel wall from thermal damage during RF-assisted surgical resection? Med Phys 41:083301
Zorbas G, Samaras T (2014) Simulation of radiofrequency ablation in real human anatomy. Int J Hyperth 30:570–578
Consiglieri L (2013) An analytical solution for a bio-heat transfer problem. Int J Bio-Sci Bio-Technol 5:267–278
Huang HW (2013) Influence of blood vessel on the thermal lesion formation during radiofrequency ablation for liver tumors. Med Phys 40:073303
Pennes HH (1948) Analysis of tissue and arterial blood temperatures in the resting human forearm. J Appl Physiol 1:93–122
Trujillo M, Berjano E (2013) Review of the mathematical functions used to model the temperature dependence of electrical and thermal conductivities of biological tissue in radiofrequency ablation. Int J Hyperth 29:590–597
Shao YL, Leo HL, Chua KJ (2018) Studying of the thermal performance of a hybrid cryo-RFA treatment of a solid tumor. Int J Heat Mass Transf 122:410–420
Ooi EH, Ooi ET (2021) Unidirectional ablation minimizes unwanted thermal damage and promotes better thermal ablation efficacy in time-based switching bipolar radiofrequency ablation. Comput Biol Med 137:104832
Barnoon P, Ashkiyan M (2020) Magnetic field generation due to the microwaves by an antenna connected to a power supply to destroy damaged tissue in the liver considering heat control. J Magn Magn Mater 513:167245
Barnoon P, Bakhshandehfard F (2021) Thermal management in a biological tissue in order to destroy tissue under local heating process. Case Stud Therm Eng 26:101105
Singh S, Melnik R (2020) Domain heterogeneity in radiofrequency therapies for pain relief: a computational study with coupled models. Bioengineering 7:35
Wang Z, Zhao G, Wang T, Yu Q, Su M, He X (2015) Three-dimensional numerical simulation of the effects of fractal vascular trees on tissue temperature and intracelluar ice formation during combined cancer therapy of cryosurgery and hyperthermia. Appl Therm Eng 90:296–304
Pérez JJ, González-Suárez A, Nadal E, Berjano E (2020) Thermal impact of replacing constant voltage by low-frequency sine wave voltage in RF ablation computer modeling. Comput Methods Programs Biomed 195:105673
Yan S, Wu X, Wang W (2016) A simulation study to compare the phase-shift angle radiofrequency ablation mode with bipolar and unipolar modes in creating linear lesions for atrial fibrillation ablation. Int J Hyperthermia 32:231–238
González-Suárez A, Trujillo M, Koruth J, d’Avila A, Berjano E (2014) Radiofrequency cardiac ablation with catheters placed on opposing sides of the ventricular wall: computer modelling comparing bipolar and unipolar modes. Int J Hyperthermia 30:372–384
Zhang X, Zheng L, Suleiman K, Shu C (2021) Combined cryosurgery and cold-responsive drug-loaded nanoparticles to enhance deep-lying tumor therapy: a mathematical model. Int J Heat Mass Transf 165:120663
Patankar S (2018) Numerical heat transfer and fluid flow. Taylor & Francis. https://doi.org/10.1201/9781482234213
Amestoy PR, Duff IS, L’Excellent JY (2000) Multifrontal parallel distributed symmetric and unsymmetric solvers. Comput Methods Appl Mech Eng 184:501–520
Amritkar A, de Sturler E, Świrydowicz K, Tafti D, Ahuja K (2015) Recycling Krylov subspaces for CFD applications and a new hybrid recycling solver. J Comput Phys 303:222–237
Knavel EM, Brace CL (2013) Tumor ablation: common modalities and general practices. Tech Vasc Interv Radiol 16:192–200
Funding
This work was partially supported by the Ministry of Science and Technology, Government of the People’s Republic of Bangladesh, and the Centennial Research Grant, University of Dhaka, Dhaka, Bangladesh.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The text "0.17em" has been removed in equations 1, 3, 6, 7, 8, 10, 11, 13, 14.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hossain, S.M.C., Zakaria, J.B., Ferdows, M. et al. Computer simulation-based nanothermal field and tissue damage analysis for cardiac tumor ablation. Med Biol Eng Comput 62, 1549–1567 (2024). https://doi.org/10.1007/s11517-024-03017-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-024-03017-y