Abstract
Purpose
With antibiotic resistance (ABR) portrayed as an increasing burden to human health, this study reviews how and to what extent toxicological impacts from antibiotic use are included in LCAs and supplement this with two novel approaches to include ABR, a consequence of antibiotic use, into the LCA framework.
Methods
We review available LCA studies that deal with toxicological aspects of antibiotics to evaluate how these impacts from antibiotics have been characterized. Then, we present two novel approaches for including ABR-related impacts in life cycle impact assessments (LCIAs). The first approach characterizes the potential for ABR enrichment in the environmental compartment as a mid-point indicator, based on minimum selective concentrations for pathogenic bacteria. The second approach attributes human health impacts as an endpoint indictor, using quantitative relationships between the use of antibiotics and human well-being.
Results and discussion
Our findings show that no LCA study to date have accounted for impacts related to ABR. In response, we show that our novel mid-point indicator approach could address this by allowing ABR impacts to be characterized for environmental compartments. We also establish cause-effect pathways between antibiotic use, ABR, and human well-being that generate results which are comparable with USEtox and most endpoint impact assessment approaches for human toxicology.
Conclusions
Our proposed methods show that currently overlooked impacts from ABR enrichment in the environment could be captured within the LCA framework as a robust characterization methodology built around the established impact model USEtox. Substantial amounts of currently unavailable data are, however, needed to calculate emissions of antibiotics into the environment, to develop minimum selective concentrations for non-pathogenic bacteria, and to quantify potential human health impacts from AB use.
Similar content being viewed by others
1 Introduction
Antibiotic (AB) substances are used for treating bacterial infections by killing or inhibiting growth of these organisms (Davies and Davies 2010; Kümmerer 2009). The term AB is broad and envelops hundreds of different compounds, of which close to 300 are classified as important for human medicine and are categorized into 30 + groups according to their origin and mode of action (World Health Organization 2019). ABs have become our primary tool for treating and preventing the proliferation of pathogenic bacterial diseases in a wide range of settings, including human medicine, livestock (van den Bogaard and Stobberingh 1999), and aquaculture farms (Sapkota et al. 2008), as well as in agriculture to control for bacterial diseases in plants (Stockwell and Duffy 2012). They are the primary treatment for pneumonia, tuberculosis and gastrointestinal infections, diseases that historically are thought to have been responsible for 30% of all human deaths, but they are also essential for post-surgical care (Fair and Tor 2014). Inappropriate use of ABs and their environmental release may, however, result in negative consequences (in a concentration dependent context) in the environmental compartment as they can: (a) infer toxic effects on several living organisms (Carlsson et al. 2009) and (b) modify microbial community compositions and affect ecological functions (Costanzo et al. 2005; Grenni et al. 2018). Additionally, negative effects to humans include: (c) indiscriminately killing both pathogenic and non-pathogenic bacteria, including bacterial communities that fill useful biological functions (Jernberg et al. 2010; Lange et al. 2016); (d) induce side effects in humans (Wypych and Marsland 2018); and (e) promote the development of antibiotic resistant genes (Jernberg et al. 2010; Pérez-Cobas et al. 2013).
Of the abovementioned impacts, antibiotic resistance (ABR) development in pathogenic bacteria is seen as the most foreboding for human wellbeing, due to the central role of ABs in modern medicine (World Health Organization 2014). Bacteria can develop resistance to ABs either through mutations or by acquisition of resistance genes from other bacteria through different modes of horizontal gene transfer even at low concentrations (i.e., ng/L to few μg/L; Cabello 2006; Grace 2015; Bengtsson-Palme and Larsson 2016; Jutkina et al. 2018; Klein et al. 2018).
ABR genes have existed for millennia (D’costa et al. 2011), but the current use of tens of thousands of tonnes of ABs each year has resulted in substantial releases of ABs into the environment (Van Boeckel et al. 2015; Robinson et al. 2016), thereby generating large areas for interactions between ABs and bacteria which can lead selection for AB resistance genes in environmental bacteria (Cabello 2006; Mathew et al. 2007; Rizzo et al. 2013; Larsson 2014; Xiong et al. 2015; Cabello et al. 2016; Chuah et al. 2016; Larsson et al. 2018; Osman et al. 2018). There is a growing body of literature connecting ABs released into the environment with the development of ABR in bacterial communities (Heinemann 1999; Wright 2007; Larsson 2014) and an increased frequency of ABR genes in environmental compartments (Finley et al. 2013), yet the links between environmental ABR bacteria and the impacts to human health are not fully understood. The collection of genes coding for ABR present in the environment can be viewed as a pool of available genetic material which can be transferred between bacteria and is commonly referred to as “the resistome” (D’Costa et al. 2006; Wright 2007; Surette and Wright 2017). Models have been developed for correlating anthropogenic AB emissions and the resistance development in the environment based on abiotic parameters (Amos et al. 2015), as well as relationships between AB use in food animal production and human exposure to ABR pathogens (van Bunnik and Woolhouse 2017). Nonetheless, it remains difficult to establish useful dose-response relationships between AB use and the associated impacts, since causalities between AB use, resistance development, and transmission are difficult to pinpoint (Price et al. 2015).
Despite the overwhelming human health benefits gained from using pharmaceuticals like ABs, it is imperative to assess the negative impacts from emissions of these substances to better improve regulation and manage impacts. Life cycle assessment (LCA), among other environmental frameworks, has been used to assess impacts related to the use of ABs. LCA details the environmental impacts related to a product’s or service’s life cycle. In LCA, human and ecosystem impacts from the release of chemicals are generally captured by toxicological impact categories. Most of these toxicological impact assessment methodologies build upon available laboratory toxicity data and extrapolation methods assigning fate, effect, and exposure pathways to chemical agents. Depending upon scope, freshwater ecotoxicity, marine ecotoxicity, and/or cancer and non-cancer-related human toxicity (European Commission 2010) are either estimated at an intermediary point in the underlying impact pathway by midpoint indicators (e.g. number of cancer or non-cancer disease cases in humans or potentially affected fraction of species in the aquatic environment; PAF m3 kg−1), or at the end of the impact pathway as endpoint indicators (e.g. disability adjusted life-years (DALY) or potentially disappeared fraction of species to change in concentration (PDF m3 kg−1) (Hauschild and Huijbregts 2015).
In this study, we first review (Sec. 3.1) how impacts from AB use and ABR have been characterized among published LCAs. We then propose two novel impact characterization models to capture ABR in LCA (Sec. 3.2) and discuss their respective strengths and weaknesses. Conclusively (Sec. 4), we summarize the outcomes to suggest best practices for AB use in LCA.
2 Methodology
2.1 Review of AB use in LCA literature
Relevant literature on previous LCA studies incorporating AB or pharmaceuticals was screened using web of science on 10 March 2021. The search used the phrase “TS = (“LCA” OR “LCIA” OR “life cycle assessment” OR “life cycle analysis” OR “life cycle inventory assessment” OR USEtox) AND TS = (antimicr* OR antibio* OR pharmaceutical* OR micropoll*))” while delimiting the search to English-language articles spanning the years 2008–2020. Search denominators and methodology overview is given in the supplementary information (Fig. S1). The search generated 266 articles that were targeted for screening, of which 80 passed a title screening. Another 37 were rejected following abstract screening. Of remaining 43 articles read in full, 27 did not characterize ABs and were excluded. Thus, 16 articles are included in the review, with the addition of the study by Henriksson et al. (2015) that had been identified prior to screening, and are summarized in Table 1. Figures were designed using RStudio, Inc, Version 1.1.423 and Microsoft PowerPoint 2016.
2.2 Proposing novel approaches to include ABR in LCA
Potential impacts of ABs reaching the environment are separated between toxicological impacts and resistance development. Toxicological impacts can be captured in the current toxicological impact model USEtox, applying a three-step approach to derive characterization factors (CFs) for toxic substances applied in the LCA, considering fate, exposure, and effect data (Fantke et al. 2017; Rosenbaum et al. 2011). For impacts related to resistance development, we choose to target: (1) ABR development in the environment as a midpoint indicator by sourcing effect data related to concentrations of ABs where resistance development can occur based on the risk assessment methodology developed by (Rico et al. 2017), and (2) human health impacts as a result from AB use by suggesting a linear dose-response model based on statistical correlation connecting AB use, resistance development and human health impacts. This was accomplished by sourcing data from veterinary and medical literature while limiting the scope to the EU due to data scarcity.
3 Results and discussion
3.1 Findings of the review
Seventeen LCA-related articles deal with ABs, of which two consider indirect toxic impacts related to AB production and transportation (Stone et al. 2010, 2011), three calculate freshwater ecotoxicity CFs for ABs and use them in LCAs (Muñoz et al. 2008; Henriksson et al. 2015; Li et al. 2019), two only calculate CFs for ABs (Alfonsín et al. 2014; Ortiz de García et al. 2017) and eight use available CFs for ABs to conduct LCAs (Muñoz et al. 2009; Hospido et al. 2010; Igos et al. 2012, 2013; Lorenzo-Toja et al. 2016; Rahman et al. 2018; Tarpani and Azapagic 2018; Tarpani et al. 2020). Meanwhile, Morais et al. (2013) compare the uncertainty and variability of characterization results at various pH using the USEtox scientific consensus model V1.01 (Rosenbaum et al. 2008), and Emara et al. 2018 compare AB-related CFs using different impact assessment methodologies. An overview of reviewed articles is presented in Table 1. The articles were published from 2008 and onwards, the same year as the USEtox consensus model was developed. Of the thirteen studies that carried out life cycle inventory assessments (LCIAs), ten evaluated wastewater treatment plant interventions and three animal farming. The two studies by Munoz et al. (2008, 2009) use both EDIP 97 (Potting and Hauschild 2006) and USES-LCA (Huijbregts et al. 2000) for LCIA, with EDIP 97 and USES-LCA 2.0 characterization methodologies respectively thereby characterizing impacts at both mid-point and endpoint. Stone et al. (2010) use ReCiPe 2008 (Goedkoop et al. 2013) that promotes USES-LCA 2.0 characterization methodology for toxicological impacts. Meanwhile, Stone et al. 2011 use EcoIndicator99 v2.06 (Goedkoop and Spriensma 2001) and Igos et al. (2012) EDIP 97 and EDIP 2003, as well as ReCiPe 2008 combined with USEtox. Igos et al. (2013) use EDIP2003 and ReCiPe 2008 combined with USEtox. Hospido et al. (2010) declares using CLM 2 baseline 2000 for midpoint impact assessment (Guinée et al. 2002). Henriksson et al. (2015), Tarpani and Azapagic (2018), and Tarpani et al. (2020) all characterize freshwater ecotoxicity using USEtox V1.01, while Lorenzo-Toja et al. (2016) characterize emissions using USES-LCA 2.0. The two last studies, Rahman et al. (2018) and Li et al. (2019), perform LCIA with TRACI 2.1, where USEtox is the proposed toxicological characterization methodology. Four studies deal with more than one toxicological characterization method as the focus of these studies is to evaluate characterization results or LCIA methodologies rather than performing LCAs.
Overall, the scope and methodologies vary substantially among studies, as do calculated CFs for ABs. Eleven studies apply USEtox methodology for impact characterizations, of which four establish CFs and seven carry out full LCAs. Among these, Alfonsín et al. (2014) characterize four ABs for both USEtox and USES-LCA. Lorenzo-Toja et al. (2016) utilize these USES-LCA CFs, while Tarpani and Azapagic (2018) and Tarpani et al. (2020) use the USEtox CFs from Alfonsín et al. (2014) for LCAs of wastewater treatment plants (WWTPs). Muñoz et al. (2008) rank the toxicity for 97 pollutants, create seven new CFs for antibiotics, and apply these in an LCA of WWTP. These CFs are subsequently used by Muñoz et al. (2009) and Hospido et al. (2010) in other LCAs of WWTPs. Henriksson et al. (2015) and Li et al. (2019) also generate novel CFs for ABs using the USEtox methodology (V1.01 and V2.0 respectively) and use them for their respective LCAs. Meanwhile, Morais et al. (2013) investigate how pH variation influence USEtox fate modelling of agents and create novel CFs for six ABs. Ortiz de García et al. (2017) calculate CFs for seven additional ABs, and Emara et al. (2018) compare available impact assessment methodologies and CFs for ABs and other agents.
Of the six studies generating novel freshwater ecotoxicity CFs for ABs, five present fate, exposure, and effect factors in their respective supplementary information. Two of these (Henriksson et al. 2015; Ortiz de García et al. 2017) also detail AB’s source toxicity data, but derive their effect factors somewhat differently. Ortiz de García et al. (2017) prioritized chronic toxicity data, as recommended by Fantke et al. (2017), while Henriksson et al. (2015) use both acute and chronic toxicity data.
To date, 40 antibiotic agents have been characterized for freshwater ecotoxicity impact with the USEtox methodology (Fig. 1; data available in supplementary information, Table S1). For some ABs that were characterized more than once, large variations exist (e.g. 3.2E + 1 PAF m3 per day and kg emitted−1 to 1.06E + 7 PAF m3 per day and kg emitted Amoxicillin), while 24 out of 40 antibiotics only were characterized once.
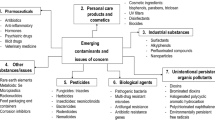
Impact pathway overview of AB from an LCIA perspective. (1) AB use data is reported as DDDs per 1000 inhabitants per day (DIDs) in respective EU country in the ECDC database (accessed 2020-09-19). (2) AB use data within the EU region reported as tonnes per year in (European Medicines Agency 2017). (3) Assessed with current fate models in USEtox. (4) No correlation between veterinary use of 3GC and resistance development in the human healthcare sector. (European Centre for Disease Prevention and Control (ECDC), European Food Safety Authority (EFSA), European Medicines Agency (EMA) 2017). (5) Correlation between veterinary use of 3GC and resistance development in the food-animal sector. (European Centre for Disease Prevention and Control (ECDC), European Food Safety Authority (EFSA), European Medicines Agency (EMA) 2017). (6) Correlation between human consumption of 3GC and resistance development in human health care sector. (European Centre for Disease Prevention and Control (ECDC), European Food Safety Authority (EFSA), European Medicines Agency (EMA) 2017). (7) Proposed characterization factor in this paper, based on minimum inhibitory concentrations (MIC) of ABs; predictions of ABR development is used as a comparative endpoint. (8) Connecting the ABR present in the environmental compartment to AB treatment failure in the human and veterinary sector; no quantitative data is available for this pathway. (9) These steps are aggregated describing the effect to human health from resistance developed. (10) Cassini et al. (2019) assessment of treatment failure attributed to ABR can be found for the 16 most common pathogen-resistance combinations in Europe. Loss of human lives and prolonged hospitalizations as an effect are assessed within the same report. (11) No quantitative data available on impacts to veterinary medicine from ABR zoonosis. (12) No quantitative data available. (13) Innes et al. (2019) report an economic impact models from of enrofloxacin use and impacts from Campylobacter, Salmonella, and E. coli bacteria as externalities from AB use, which reaches US$ 2200 per kg enrofloxacin used. The model might accommodate calculations for 3GC in the EU as well. (14) A rational for establishing nutritional losses needs to be settled on. We would argue that there are highly variable regional differences across the world. In high-income regions, nutrients are easily substituted from another food source in contrast to low-income regions. However, antibiotic use strategies surely vary between small-holder animal husbandry and industrial-scale farming in the latter regions (no use vs. some use respectively). (15) Ecotoxicological modelling according to USEtox, damage to the ecosystem from increased AB concentrations in the environment is characterized as freshwater ecotoxicity impacts. (16) Weak evidence for damage to ecosystem from ABR (Eckert et al. 2019). (17) End-point measurement of ecotoxicological effects, no clear ecosystem effect from ABR
Despite novel contributions of AB CFs using USEtox, only 40 of the over 300 ABs deemed critically important for human medicine have been characterized for freshwater ecotoxicity (Fantke et al. 2017; World Health Organization 2019). Moreover, the USEtox V2.01 database presents 23 readily available human health impacts for ABs, but only four of these have CFs for human toxicity attributed, the rest are defined as either “n.a” or “0”, which implies toxicity data are labelled as “neglected” (USEtox® organic substances database 2.01 [built 10-July-2017]). An additional nine ABs are characterized for human health impacts among the reviewed studies (see Table 2 based on data from Emara et al. 2018). The CFs from Ortiz de García et al. (2017) are reported as “human toxicity potential – total” (an aggregation of both carcinogenic and non-carcinogenic impact), yet the toxicological input data label all of the characterized ABs as non-carcinogenic (NC) and they are therefore labelled as HTP-NC in Table 2.
To summarize, the use of ABs and the environmental release of AB residues may result in ecotoxicological impacts on animals and humans, changes in microbial communities in ecosystems and humans, and resistance development. Ecotoxicological impacts are addressed in several LCA studies using different LCIA methodologies. Most of the reviewed studies look at freshwater ecotoxicity using USEtox, but conclude up to six orders of magnitude difference in CFs for some ABs. The cause for inconsistencies in freshwater ecotoxicity CFs remains unclear since the underlying toxicity data used for calculating the effect factors remain unavailable. However, Morais et al. (2013) show that CFs are sensitive to differences in abiotic degradation rates as well as ecotoxicological effect (EC50) data, which generally are sourced from different empirical experiments, as no standardized database for such data is available for ABs. Nonetheless, the chemical properties and experimental data on ABs that support the CFs remain inconsistent across literature. Greater efforts are therefore needed towards generating further modelling and experimental data for some compounds, as well as completing and harmonizing datasets of toxicological properties that could support effect factors to yield robust CFs.
Based on our review, we conclude that the most severe knowledge gaps include the evaluation of potential human health impacts pathways from AB use, resistance development in the environment, and human health impacts associated to ABR. Four LCA studies included impacts from ABs on human health, but no LCA study to date that is assessing potential human health impacts has tried to capture the consequences of ABR. So far the only impacts considered are direct toxicity without addressing ABR, which is briefly mentioned by Igos et al. (2012) and Emara et al. (2018). As described by Ashbolt et al. (2013), resistance genes which propagate in the environment and become a human health issue adhere to different pathways than ecotoxicological impacts and will therefore require a different impact assessment approach. Since ABs act as a causative agent for ABR development, spread of resistant bacteria can subsequently occur in the environment and be transmitted to humans. Both latter steps cannot be assessed through physiochemical fate models because bacteria are the main carriers of these resistance genes and they propagate through complex biological interactions. As such, disease transmission and subsequent impacts on human health are not assessed using the exposure and effect pathways currently included in the USEtox model (Eq. 1). Without relevant pathways to capture the extent of ABR impacts, these are possibly greatly underestimated in LCAs.
3.2 Two proposed approaches for addressing ABR in LCA
Since no cause-effect pathway exists for the impacts of ABR development in LCIA methodology, we below present two novel approaches that could potentially allow for ABR impacts to be quantified using causal relationships: (1) the use of minimum selective concentration (MSC) distributions to characterize ABR enrichment in the environment as a mid-point impact; and (2) the correlation between ABs used on regional scale with human health impacts caused by ABR, quantified as DALYs per kg of AB used as an endpoint impact.
The first approach, modelling of ABR enrichment in the environment, uses the USEtox® methodology as a starting point, as it is the framework recommended by both the Society of Environmental Toxicology and Chemistry (SETAC) and the Joint Research Centre (European Commission 2010). In USEtox, Fate factors capture the physiochemical properties of agents and predict their estimated distribution in environment compartments; exposure factors calculate bioavailability to aquatic organisms or exposure pathways for humans, while effect factors benchmark the actual toxicity of a compound, generally based upon laboratory studies (Eq. 1 describes human impact characterization and Eq. 3 describes ecotoxicological characterization).
Again, this approach is aimed at capturing toxicological effects of ABs, and does not prescribe how to incorporate ABR impacts.
3.2.1 Approach 1: characterizing ABR enrichment in the environment (mid-point)
Approach 1 attempts to quantify the enrichment of resistance genes in environmental bacteria based on environmental fate models for ABs and theoretical minimum selective concentration (MSC) distributions as a mid-point impact, similar to USEtox’s ecotoxicity impacts.
The proposed characterization model is based on the methodology developed by Rico et al. (2017), where MSCs are inferred from minimum inhibitory concentrations (MIC) for pathogenic bacteria obtained from the EUCAST database (European Committee on Antimicrobial Susceptibility Testing 2020). In their study, MSCs were extrapolated from MICs by applying a flat extrapolation factor of 10. These extrapolation factors are derived as the mean MIC/MSC ratio obtained in experimental studies (Gullberg et al. 2011; Liu et al. 2011), but refinements of this extrapolation factor should be implemented as soon as further experimental or modelling data become available. Such improvements should account for differences between broad-spectrum and selective antibiotics, considering their mode of action in bacteria.
MSC data for each antibiotic are used to fit normal distributions to the log-transformed MSC data, similarly to the species sensitivity distribution approach used in ecotoxicological impact characterization (Posthuma et al. 2001). In an analogous manner, the MSC distributions could be used to extrapolate the hazardous concentration that will promote the development of ABR in 50% of bacteria (HC50), which can be calculated as the geometric mean of the MSC data. A difference to ecotoxicity characterization methodology in USEtox is that HC50 values are generated from the geometric mean of chronic EC50 or LC50 values (effect concentration for 50% of tested organisms and lethal concentration of 50% of tested organisms respectively) for aquatic organisms from several trophic levels (Fantke et al. 2017). A chronic endpoint is preferred as the chemical fate and exposure calculations are performed following a steady-state approach, so estimated environmental concentrations resemble chronic exposure (Guinée and Heijungs 1993). The use of EC50 or LC50 values, as opposed to a no observed effect concentration (NOEC) or lowest observed effect concentration (LOEC), is mainly supported by the statistical robustness of the 50% response level (Crane and Newman 2000; Larsen and Hauschild 2007). In the proposed approach, the MSCs approximate the chronic resistance LOEC for bacteria, which are based on thousands of data points compiled in the EUCAST database rather than on a single dose-response experiment, so a sufficient statistical robustness is assumed for this value as representative for a given bacterial taxon. Furthermore, the number of bacteria that is included in the EUCAST database is large (> 8) for the most commonly used antibiotics (Bengtsson-Palme and Larsson 2016). Questionable is how representative the pathogenic bacteria included in the EUCAST database are for bacterial communities in the environment. In this regard, Bengtsson-Palme and Larsson (2016) demonstrate a weak link between taxonomic divergence and sensitivity to antibiotics, and the study by Tello et al. (2012) finds no significant difference in sensitivity between pathogenic bacteria that inhabit human bodies exclusively and those that have been reported to also inhabit environmental compartments. Thus, the EUCAST database presents itself as a useful proxy for estimating the susceptibility of environmental communities to antibiotic pressure.
Similarly to the formula established by Jolliet et al. (2003) for the effect factor calculation for ecotoxicity, the effect factor for ABR enrichment in environmental bacteria (EFABR) can be calculated as:
EFABR: ABR effect factor for a given environmental compartment e.g. freshwater ecosystems (PAF m3 kg−1).
HC50: geometric mean of MSCs for bacteria (kg m−3).
In ecotoxicity assessments, the effect factor relates to the change in PAF as a result of increases in contaminant concentration. In the proposed ABR enrichment assessment, this will refer to the change in the fraction of bacterial populations that acquire a significant increase of resistance genes due to a unit increase of AB exposure concentration. Analogous to the ecotoxicity assessment, it is based on a linear extrapolation from the HC50 down to HC0 (slope of 0.5), and assumes that the acquisition of resistance at the community level increases with AB concentration.
Finally, the ABR characterization factor (PAF m3 day per kg emitted) can be calculated as
where the fate factor describes the distribution of chemicals in the environment and the exposure factor describes the bioavailable fraction of chemicals that could cause harm to freshwater organisms (Fantke et al. 2017), thus utilizing the established modelling framework USEtox for characterizing distribution of ABs in the environment while only modifying the effect factor.
Following the methodology described above, ABR-HC50 values were generated for 14 ABs to replace ecotoxicological HC50 for USEtox input data (Table S5). The USEtox calculations were set up in the USEtox® 2.1 [built 19-Oct-2017] interface software (available at https://usetox.org/), selecting freshwater emission ecotoxicity and applying default USEtox setting environment. ABR enrichment characterization factors could subsequently be generated in harmony with USEtox 2.1 (Table 3).
These results show that applying MSC-based HC50 values for ABs enables us to derive characterizations that fit the formerly established LCA framework, thereby complementing existing freshwater ecotoxicity impacts with ABR specific impacts. It should be clarified that the CFs generated by this model serve as comparative units of impact related to the resistance HC50 for bacteria at the community level, and not as a representation of resistance development dynamics following a concentration gradient, which could theoretically generate selection for resistance in bacteria at low concentrations, as well as remove resistance at high concentrations (e.g. killing bacteria). A strength of this approach is that all MIC data can be sourced from the EUCAST database, thus removing variations in HC50 values due to different data sourcing, as highlighted for ecotoxicological data above.
Finally, a point on the ecological relevance of this approach should be raised. The LCA framework accounts for emissions under steady-state conditions (Guinée and Heijungs 1993), while AB emissions can be influenced by pharmacokinetics and environmental processes, and ABR development depend on the exposure level as well as on the exposure duration (Ashbolt et al. 2013). This implies that the applicability of this model serves better for systems with continuous emissions than systems with erratic AB use (e.g., WWTPs vs. aquaculture farms), but may be under-representing exposure scenarios that are prolonged in long periods. Additionally, events related to proliferation of resistance genes following ABR development, across species and exposure to humans, are not captured within this model. Such quantifications would be highly dependent on the exposure level and duration, and the bacteria present in the environment, which would need to account for more complex pathways. Connecting ABR enrichment in the environment to human health impacts (8 in Fig. 2) by incorporating other methods is currently being explored (Ashbolt et al. 2013; Ben et al. 2019), but is hampered by a lack of relevant data on how AB concentrations influence resistance development in human pathogenic bacteria and quantitative pathways describing environmental exposure to ABR. Hence, below we explore an alternative approach relating the use of ABs to human health impacts from ABR, which goes beyond the explanation of mechanistic relationships and the quantitative determination of each of these pathways.
3.2.2 Approach 2: characterizing human health impacts for ABR (endpoint)
Our alternative approach for establishing linear dose-response relationships between AB use and ABR consequences for human well-being is conceptualized in Fig. 2. Ideally, one would quantify each pathway individually, but data scarcity currently forces us to exercise a generalized mass balance approach where only pathways 1, 2, 4, 6, 9, and 10 are aggregated into one pathway (Fig. 2). Our proposed linear dose-response model assumes that any use of ABs will contribute to resistance development, which allows us to circumvent the shortcomings in data connecting environmental ABR to human health impacts. This implies a loss of ecological relevance, but enables quantification of potential impacts from AB use at regional scales. Data sourced to support the approach are presented in supplementary information (Tables S2, S3, and S4 in supplementary information).
The relationship between AB use and ABR development is inferred by the Joint Interagency Antimicrobial Consumption and Resistance Analysis (JIACRA) report, which presents logistic regression models correlating use of 21 different ABs from five classes in human and food-animal production in the EU and resistance development in five human pathogens (Salmonella spp., Campylobacter coli, C. jejuni, Escherichia coli, and Enterococci) (European Centre for Disease Prevention and Control (ECDC), European Food Safety Authority (EFSA), and European Medicines Agency (EMA) 2017). This report calculates odds ratios based on logistic regression analysis of AB use data and resistance development data to suggest statistically correlated associations between human and animal consumption of antibiotics, and resistance development in selected human pathogens. Odds ratios are explained by Szumilas (2010, p227) as the representation of “the chance that an outcome will occur given a particular exposure compared to the odds of the outcome occurring in the absence of that exposure”.
In LCA, the endpoint of toxicological impact to humans is expressed as disability adjusted life years (DALY), a metric that accounts for the years lost due to premature mortality and productive life due to disability, and is globally scalable (Murray and Lopez 1994). We therefore argue that the common unit for ABR impacts to human health would be the same, given that it is a well-established concept in LCA’s cause-effect endpoint pathways. Data available on the impacts to human health have been published by Cassini et al. (2019), who produced an extensive report on the human health impacts from AB-resistant pathogens within the EU health care system, attributing DALYs to 16 pathogen-ABR combinations.
We subsequently use the impact pathway between AB use and DALYs to account for AB use in human and veterinary medicine respectively (1 and 2 in Fig. 2) in the EU, by establishing a causal relationship between AB use and ABR development (4 and 6 in Fig. 2) together with the impacts caused by the subsequent failure to treat infections due to ABR (9 and 10 in Fig. 2). We argue that the use and effect pathways should be parameterized according to the region of interest (country or continental scale), since availability and enforcement of local and regional policy will arguably shape the use and misuse patterns of ABs at each level (Laxminarayan and Malani 2007; Søgaard Jørgensen et al. 2020).
To build a model for expressing DALYs as a product of AB use, we rely on published odds ratio data from the JIACRA report (given that there is a significant correlation (e.g. CI does not cross 1 and p < 0.05)) to express a correlation coefficient between the use and resistance development for the investigated AB as
where
∂x,p,sector,reg = correlation coefficient explaining the relationship between use in the investigated sector (human or veterinary) and resistance development in pathogen p to antibiotic x in the investigated region.
ORx,sector,reg = odds ratio implying the strength of association between use of AB x and resistance development for each pathogen p in the investigated sector and region.
Since odds ratio values range between 0 to infinity, we express this coefficient as the square root of ln OR to not suggest an overrepresentation of the odds for resistance development in a particular sector. This correlation coefficient is subsequently used to imply an effect from AB use on resistance development, expressed as
where
ABFx,p,reg = total resistance developed in pathogen p from use of antibiotic x in the investigated region (resistance per kg year−1).
ABUx,hum,reg = total use of antibiotic x in human health sector in the investigated region (kg year−1).
∂x,p,hum,reg = correlation coefficient explaining relationship between human use and resistance development in pathogen p to antibiotic x in the investigated region.
ABUx,vet,reg = total use of antibiotic x in veterinary sector in the investigated region (kg year−1).
∂x,vet,region = correlation coefficient explaining relationship between veterinary sector use and resistance development in pathogen p to antibiotic x in the investigated region.
Next, the pathways between ABF to ABR related impacts need to be defined (9 in Fig. 2). This step needs to be aggregated with the subsequent effect; loss of lives, and prolonged hospitalization (10 in Fig. 2), here expressed as
DALYx,p,reg = disability adjusted life years attributed to resistance to AB x in pathogen p per region and year.
This gives us a mass balance approach attributing DALYs per kg AB used in the investigated region expressed as
To demonstrate our proposed cause-effect pathway, we allocate DALYs to the use of 3rd-generation cephalosporin (3GC) in EU, a group of beta-lactam antibiotics to which 18 ABs belong. This class of ABs is classified as critically important for human medicine (World Health Organization 2019), yet is still used within food-animal production to some extent (European Medicines Agency 2019). 3GC resistance is also among the top contributors to pathogen-ABR related mortalities in the EU (Cassini et al. 2019). Following the pathways of Fig. 2, we initially establish quantities of 3GC used in the EU for 2015. According to the ECDC Database (accessed 2020-09-17), close to 270 tonnes of 3GC were used for human treatment (both community and hospital use) in 2015 (Table S2), while the European Medicines Agency (2017) reports 13.9 tonnes 3GC used in animal husbandry that same year, totalling about 284 tonnes annually.
Data are available on odds ratios from the JIACRA report (European Centre for Disease Prevention and Control (ECDC), European Food Safety Authority (EFSA), European Medicines Agency (EMA) 2017) for human consumption of 3rd- and 4th-generation cephalosporin antibiotics (3GC) and resistance development in human pathogen E. coli. Note that use of 3rd-generation and 4th-generation cephalosporins is reported as a sum, but will be addressed as 3GC in this example for simplicity. The reported odds ratio for this specific AB-pathogen combination is 1.94 (CI 1.47–2.54, p-value < 0.001), which implies that odds are 94% for resistance to develop in E. coli for each increased defined daily dose of 3GC in the human sector. For the veterinary sector, however, the report shows no statistically significant correlation between animal consumption of 3GC and resistance development in the human pathogen E. coli (odds ratio 4.13 CI 0.78–21.08, p-value < 0.094), and ∂x,vet,region will hence be accounted for as “0”.
Cassini et al. (2019) report that the most critical pathogen resistance related–infections to human health is 3GC resistant Escherichia coli. This pathogen caused a median number of 37.2 DALYs per 100,000 population reported in 2015; 191 883 DALYs across Europe this year given a population of 515.8 million. We input data into our model Eq. 7 according to Eqs. 4, 5, and 6:
which yields the following for our pathogen-resistance combination E. coli infections resistant to 3GC example (Eq. 8):
To put this in perspective, we compare our 0.873 DALYs kg−1 AB with the single available characterization of a cephalosporin-class AB, Cefaclor, a 2nd-generation cephalosporin, characterized by Ortiz de García et al. (2017) using USEtox methodology (i.e. non-homologous methodology as to the case above). Ortiz de García et al. (2017) report that the median attributed DALYs are 5.48*10−8 DALY per kgemitted as non-carcinogenic impact (ranging from 8.62*10−12 DALY per kgemitted to 1.98*10−8 DALY per kgemitted depending on emission compartment selected).
This example shows that causal relationships are possible to infer between AB use and DALYs, but overlooks several important aspects and suffers from data scarcity. Nonetheless, we manage to establish a CFABR for 3GC that associates seven orders of magnitude higher DALYs per kg of AB compared to a CF for a related AB which only considers direct toxicity impacts on humans. It should be noted, that 3GC is the only AB with enough data available to describe this pathway in a European setting currently. For instance, Cassini et al. (2019) do attribute DALYs to another pathogen resistant to 3GC, but there is no available odds ratio for this combination in the JIACRA report (European Centre for Disease Prevention and Control (ECDC), European Food Safety Authority (EFSA), European Medicines Agency (EMA) 2017) and characterizing additional ABs using this linear dose-response concept will require substantial data collection at regional levels. However, as data are continuously being generated and reported, we would expect that the coverage of this approach could be expanded in the future (Limmathurotsakul et al. 2019).
Our endpoint approach is designed to characterize AB use in both human health and veterinary sectors, to account for total use of antibiotics within a region following the One Health concept, acknowledging that ABs can promote ABR regardless of sector. Ideally, refining Eq. 5 to include emissions of ABs at a production stage would improve the model even further, but data on the amounts of ABs emitted during production are largely nonexistent, while they are reported to be substantial in some areas (Larsson 2014; el Balkiny 2014). Despite that this dose-response concept is an oversimplification of the complex cause-effect pathways connecting AB use, resistance development, dissemination, and human health impacts, we still had to aggregate stages in the pathway. Also, considering the limited data availability on ABR-related human impacts, only 16 pathogen-resistance combinations are available from Cassini et al. (2019), which limits the applicability of this approach. ABR frequencies and damage to human health caused by economic and nutritional losses from livestock mortalities are neither considered in our example (11–14 in Fig. 2), though Innes et al. (2019) have proposed a model to account for economic losses in a US setting which could possibly be included at further development of this model. Additional economic costs from prolonged hospitalizations due to resistant infections is neither included in our model, which is focusing on health impacts, but a similar approach could possibly be included using life cycle costing (Estevan and Schaefer 2017). Moreover, we limit ourselves to a European setting where AB use could be expected to be fairly well regulated, including proper reporting on and administration of drugs, destruction of excess drugs, full treatment cycles of patients and animals, and possible preliminary screenings for ABR genes. The current practical applicability to LCA of this suggested approach could be questioned since there is no ability to compartmentalize emissions and suggest impacts related to various environments. The assumptions made for the linear dose-response concept completely disregard the beneficial aspects of AB use since many lives are saved each year by these pharmaceuticals and modern medicine relies upon functional antibiotics, but the reasoning of human health benefits holds true for the many other chemicals as well, and could be discussed with a broader audience. Conclusively, applying this type of simplified linear dose-response concept for AB use while circumventing stochastic dynamics of ABR development and the contribution of resistance from the environmental compartment will imply statistical inference without causality.
Since there is no available methodology to extrapolate how environmental ABR impacts human health in an LCA context, we had to create two separate pathways, one prospective method which looks at the onset of ABR in environmental bacteria using the established characterization model USEtox, and a second retrospective method based on statistical correlations between AB use and human health impacts. Since these models are based on different assumptions with little commonality, they express different strengths and shortcomings that need to be considered before implementation. We view these two novel AB characterization methodologies as steppingstones to further refinements and discussions on the holistic assessment of ABs and resistance development in LCA.
4 Conclusions
ABs have been assumed to contribute to ecotoxicity and human toxicity in seventeen LCAs, but the latter impact category is sparsely characterized. Moreover, ABR impacts as a consequence of AB use have not yet been accounted for in LCA, which suggests that the full impacts of AB use in LCAs are severely underestimated. In response, we present two approaches that acknowledge these impacts and that can be readily included in existing impact assessment models to generate characterization factors for ABR enrichment in the environment at a mid-point level, and a correlation between AB use and DALYs for endpoint impacts. The mid-point characterization approach for ABR enrichment in the environment provides a robust comparative model for assessing AB use or removal from wastewater, agriculture, or industrial processes. Further development of this methodology would benefit from refining the current MIC to MSC extrapolations since a fair amount of AB MIC data are available. For the endpoint approach, we use 3GC as an example to prove the concept of our theory, but few causal relationships and data limitations challenge the practical usefulness of this approach at present. We would therefore recommend caution when interpreting human health impacts from ABs in LCA studies until more holistic methodologies and better data become available. Future LCAs including ABs should ideally adopt a One Health approach and could benefit from complementary environmental risk assessments, allowing for the dynamics of AB use and emission in all relevant sectors to be accounted for.
Change history
09 August 2021
A Correction to this paper has been published: https://doi.org/10.1007/s11367-021-01950-w
References
Alfonsín C, Hospido A, Omil F, Moreira MT, Feijoo G (2014) PPCPs in wastewater - update and calculation of characterization factors for their inclusion in LCA studies. J Clean Prod 83:245–255. https://doi.org/10.1016/j.jclepro.2014.07.024
Amos GC, Gozzard E, Carter CE, Mead A, Bowes MJ, Hawkey PM, Zhang L, Singer AC, Gaze WH, Wellington EMH (2015) Validated predictive modelling of the environmental resistome. ISME J 9:1467–1476. https://doi.org/10.1038/ismej.2014.237
Ashbolt NJ, Amézquita A, Backhaus T, Borriello P, Brandt KK, Collignon P, Coors A, Finley R, Gaze WH, Heberer T, Lawrence JR, Larsson DGJ, McEwen SA, Ryan JJ, Schönfeld J, Silley P, Snape JR, Van den Eede C, Topp E (2013) Human health risk assessment (HHRA) for environmental development and transfer of antibiotic resistance. Environ Health Perspect 121:993–1001. https://doi.org/10.1289/ehp.1206316
Barceló D, Petrovic M, eds. (2011) The Ebro river basin. Springer Science & Business Media.
Ben Y, Fu C, Hu M, Liu L, Wong MH, Zheng C (2019) Human health risk assessment of antibiotic resistance associated with antibiotic residues in the environment: A review. Environ Res 169:483–493. https://doi.org/10.1016/j.envres.2018.11.040
Bengtsson-Palme J, Larsson DGJ (2016) Concentrations of antibiotics predicted to select for resistant bacteria: proposed limits for environmental regulation. Environ Int 86:140–149. https://doi.org/10.1016/j.envint.2015.10.015
Cabello FC (2006) Heavy use of prophylactic antibiotics in aquaculture: a growing problem for human and animal health and for the environment. Environ Microbiol 8:1137–1144. https://doi.org/10.1111/j.1462-2920.2006.01054.x
Cabello FC, Godfrey HP, Buschmann AH, Dölz HJ (2016) Aquaculture as yet another environmental gateway to the development and globalisation of antimicrobial resistance. Lancet Infect Dis 16:e127–e133. https://doi.org/10.1016/S1473-3099(16)00100-6
Carlsson G, Örn S, Larsson DGJ (2009) Effluent from bulk drug production is toxic to aquatic vertebrates. Environ Toxicol Chem 28:2656. https://doi.org/10.1897/08-524.1
Cassini A, Högberg LD, Plachouras D et al (2019) Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: a population-level modelling analysis. Lancet Infect Dis 19:56–66. https://doi.org/10.1016/S1473-3099(18)30605-4
Chuah LO, Effarizah ME, Goni AM, Rusul G (2016) Antibiotic Application and Emergence of Multiple Antibiotic Resistance (MAR) in Global Catfish Aquaculture. Curr Environ Heal reports 3:118–127. https://doi.org/10.1007/s40572-016-0091-2
Costanzo SD, Murby J, Bates J (2005) Ecosystem response to antibiotics entering the aquatic environment. Mar Pollut Bull 51:218–223. https://doi.org/10.1016/j.marpolbul.2004.10.038
Crane M, Newman MC (2000) What level of effect is a no observed effect? Environ Toxicol Chem 19:516–519. https://doi.org/10.1002/etc.5620190234
D’Costa VM, King CE, Kalan L, Morar M, Sung WWL, Schwarz C, Froese D, Zazula G, Calmels F, Debruyne R, Golding GB, Poinar HN, Wright GD (2011) Antibiotic resistance is ancient. Nature 477:457–461. https://doi.org/10.1038/nature10388
D’Costa VM, McGrann KM, Hughes DW, Wright GD (2006) Sampling the antibiotic resistome. Science 311:374–377. https://doi.org/10.1126/science.1120800
Davies J, Davies D (2010) Origins and evolution of antibiotic resistance. Microbiol Mol Biol Rev 74:417–433. https://doi.org/10.1128/MMBR.00016-10
Dobbins LL, Usenko S, Brain RA, Brooks BW (2009) Probabilistic ecological hazard assessment of parabens using Daphnia magna and Pimephales promelas. Environ Toxicol Chem 28:2744–2753. https://doi.org/10.1897/08-523.1
Eckert EM, Quero GM, Di Cesare A, Manfredini G, Mapelli F, Borin S, Fontaneto D, Luna GM, Corno G (2019) Antibiotic disturbance affects aquatic microbial community composition and food web interactions but not community resilience. Mol Ecol 28:1170–1182. https://doi.org/10.1111/mec.15033
el Balkiny H (2014) Determination of veterinary pharmaceuticals in production wastewater by TLC-densitometry. Anal Chem Lett 4:319–328. https://doi.org/10.1080/22297928.2014.925823
Emara Y, Lehmann A, Siegert MW, Finkbeiner M (2018) Modeling pharmaceutical emissions and their toxicity-related effects in life cycle assessment (LCA): a review. Integr Environ Assess Manag 15:6–18. https://doi.org/10.1002/ieam.4100
Estevan H, Schaefer B (2017) Life Cycle Costing - state of the art report. ICLEI – Local Gov Sustain Eur Secr 50. Available at https://sppregions.eu/fileadmin/user_upload/Life_Cycle_Costing_SoA_Report.pdf
European Centre for Disease Prevention and Control (ECDC), European Food Safety Authority (EFSA), European Medicines Agency (EMA) (2017) ECDC/EFSA/EMA second joint report on the integrated analysis of the consumption of antimicrobial agents and occurrence of antimicrobial resistance in bacteria from humans and food-producing animals – Joint Interagency Antimicrobial Consumption and Resistance Analysis (JIACRA) Report. EFSA Journal 2017;15(7):4872, 135 pp. https://doi.org/10.2903/j.efsa.2017.4872
European Commission (2010) Joint Research Centre - Institute for Environment and Sustainability: International Reference Life Cycle Data System (ILCD) Handbook - review schemes for Life Cycle Assessment. EUR 24710 EN. Luxembourg. Publications Office of the European Union; 2010. https://doi.org/10.2788/39791
European Medicines Agency (2017) Sales of veterinary antimicrobial agents in 30 European countries in 2015: trends from 2010 to 2015. Seventh ESVAC report. EMA/184855/2017
European Medicines Agency (2019) Sales of veterinary antimicrobial agents in 31 European countries in 2017: trends from 2010 to 2017. Ninth ESVAC Report. EMA/294674/2019
European Committee on Antimicrobial Susceptibility Testing (2020) Data from the EUCAST MIC distribution website. http://www.eucast.org. Accessed 11 Nov 2020
Fantke P (ed.), Bijster M, Guignard C, Hauschild M, Huijbregts M, Jolliet O, Kounina A, Magaud V, Margni M, McKone T, Posthuma L, Rosenbaum RK, van de Meent D, van Zelm R (2017) USEtox® 2.0 Documentation (Version 1). http://usetox.org
Fair RJ, Tor Y (2014) Antibiotics and bacterial resistance in the 21st century. Perspect Medicin Chem 25–64. https://doi.org/10.4137%2FPMC.S14459
Fent, K, Weston AA, Caminada D (2006) Ecotoxicology of human pharmaceuticals. Aquat. Toxicol. 76: 122-159. https://doi.org/10.1016/j.aquatox.2005.09.009
Finley RL, Collignon P, Larsson DGJ, Mcewen SA, Li XZ, Gaze WH, Reid-Smith R, Timinouni M, Graham DW, Topp E (2013) The scourge of antibiotic resistance: the important role of the environment. Clin Infect Dis 57:704–710. https://doi.org/10.1093/cid/cit355
Goedkoop M, Heijungs R, Huijbregts M, De Schryver A, Struijs JV, Van Zelm R (2013) A life cycle impact assessment method which comprises harmonised category indicators at the midpoint and the endpoint level. First edition (version 1.08). The Hague, Ministry of VROM.
Goedkoop M, Spriensma R (2001) The Eco-indicator 99 - a damage oriented method for life cycle impact assessment. PRé Consult b.v, Amersfoort, Netherlands
Grace D (2015) Review of evidence on antimicrobial resistance and animal agriculture in developing countries. Evidence on Ddemand, UK. https://doi.org/10.12774/eod_cr.june2015.graced
Grenni P, Ancona V, Caracciolo AB (2018) Ecological effects of antibiotics on natural ecosystems: a review. Microchem J 136:25–39. https://doi.org/10.1016/j.microc.2017.02.006
Guinée J, Heijungs R (1993) A proposal for the classification of toxic substances within the framework of life cycle assessment of products. Chemosphere 26:1925–1944. https://doi.org/10.1016/0045-6535(93)90086-K
Guinée JB, Gorrée M, Heijungs R, Huppes G, Kleijn R, de Koning A, van Oers L, Sleeswijk AW, Sangwon S, Udo de Haes HA, de Bruijn JA, van Duin R, Huijbregts MA (2002) Handbook on life cycle assessment: operational guide to the ISO standards. Kluwer Academic Publishers, Dordrecht
Gullberg E, Cao S, Berg OG, Ilbäck C, Sandegren L, Hughes D, Andersson DI (2011) Selection of resistant bacteria at very low antibiotic concentrations. PLoS Pathog 7:1–9. https://doi.org/10.1371/journal.ppat.1002158
Hauschild MZ, Huijbregts MAJ (2015) Life cycle impact assessment - the complete world of life cycle assessment. Springer, Netherlands, Dordrecht
Heinemann JA (1999) How antibiotics cause antibiotic resistance. Drug Discov Today 4:72–79. https://doi.org/10.1016/S1359-6446(98)01294-X
Henriksson PJG, Rico A, Zhang W, Ahmad-Al-Nahid S, Newton R, Phan LT, Zhang Z, Jaithiang J, Dao HM, Phu TM, Little DC, Murray FJ, Satapornvanit K, Liu L, Liu Q, Haque MM, Kruijssen F, De Snoo GR, Heijungs R, Van Bodegom PM, Guinée JB (2015) Comparison of Asian aquaculture products by use of statistically supported life cycle assessment. Environ Sci Technol 49:14176–14183. https://doi.org/10.1021/acs.est.5b04634
Hospido A, Carballa M, Moreira M, Omil F, Lema JM, Feijoo G (2010) Environmental assessment of anaerobically digested sludge reuse in agriculture : potential impacts of emerging micropollutants. Water Res 44:3225–3233. https://doi.org/10.1016/j.watres.2010.03.004
Huijbregts MA, Thissen U, Guinée JB, Jager T, Kalf D, Van de Meent D, Ragas AM, Sleeswijk AW, Reijnders L (2000) Priority assessment of toxic substances in life cycle assessment. Part I: calculation of toxicity potentials for 181 substances with the nested multi-media fate, exposure and effects model USES–LCA. Chemosphere 1;41(4):541–73. https://doi.org/10.1016/S0045-6535(00)00030-8
Iannacone J, Alvariño L (2009) Aquatic risk assessment of seven pharmaceutical products on Daphia magna. Ecol Apl 8:71. https://doi.org/10.21704/rea.v8i1-2.384
Igos E, Benetto E, Venditti S, Köhler C, Cornelissen A (2013) Comparative and integrative environmental assessment of advanced wastewater treatment processes based on an average removal of pharmaceuticals Elorri Igos, Enrico Benetto, Silvia Venditti, Christian Köhler. Water Sci Technol 67:387–394. https://doi.org/10.2166/wst.2012.581
Igos E, Benetto E, Venditti S, Kohler C, Cornelissen A, Moeller R, Biwer A (2012) Is it better to remove pharmaceuticals in decentralized or conventional wastewater treatment plants? A life cycle assessment comparison. Sci Total Environ 438:533–540. https://doi.org/10.1016/j.scitotenv.2012.08.096
Innes GK, Randad PR, Korinek A, Davis MF, Price LB, So AD, Heaney CD (2019) External societal costs of antimicrobial resistance in humans attributable to antimicrobial use in livestock. Annu Rev Public Health 41:141–157. https://doi.org/10.1146/annurev-publhealth-040218-043954
Isidori M, Lavorgna M, Nardelli A, Parrella A, Previtera L, Rubino M (2005) Ecotoxicity of naproxen and its phototransformation products. Sci Total Environ 348:93–101. https://doi.org/10.1016/j.scitotenv.2004.12.068
Jernberg C, Löfmark S, Edlund C, Jansson JK (2010) Long-term impacts of antibiotic exposure on the human intestinal microbiota. Microbiology 156:3216–3223. https://doi.org/10.1099/mic.0.040618-0
Jolliet O, Margni M, Charles R, Humbert S, Payet J, Rebitzer G, Rosenbaum R (2003) IMPACT 2002+: a new life cycle impact assessment methodology. Int J Life Cycle Assess 8:324–330. https://doi.org/10.1007/BF02978505
Jutkina J, Marathe NP, Flach CF, Larsson DGJ (2018) Antibiotics and common antibacterial biocides stimulate horizontal transfer of resistance at low concentrations. Sci Total Environ 616–617:172–178. https://doi.org/10.1016/j.scitotenv.2017.10.312
Klein EY, Van Boeckel TP, Martinez EM, Pant S, Gandra S, Levin SA, Goossens H, Laxminarayan R (2018) Global increase and geographic convergence in antibiotic consumption between 2000 and 2015. Proc Natl Acad Sci 201717295. https://doi.org/10.1073/pnas.1717295115
Kümmerer K (2009) Antibiotics in the aquatic environment - a review - part I. Chemosphere 75:417–434. https://doi.org/10.1016/j.chemosphere.2008.11.086
Lange K, Buerger M, Stallmach A, Bruns T (2016) Effects of antibiotics on gut microbiota. Dig Dis 34:260–268. https://doi.org/10.1159/000443360
Larsen HF, Hauschild M (2007) GM-troph: a low data demand ecotoxicity effect indicator for use in LCIA. Int J Life Cycle Assess 12:79–91. https://doi.org/10.1065/lca2006.12.288
Larsson DGJ (2014) Antibiotics in the environment. Ups J Med Sci 119:108–112. https://doi.org/10.3109/03009734.2014.896438
Larsson DGJ, Andremont A, Bengtsson-Palme J, Brandt KK, de Roda Husman AM, Fagerstedt P, Fick J, Flach CF, Gaze WH, Kuroda M, Kvint K, Laxminarayan R, Manaia CM, Nielsen KM, Plant L, Ploy MC, Segovia C, Simonet P, Smalla K, Snape J, Topp E, van Hengel AJ, Verner-Jeffreys DW, Virta MPJ, Wellington EM, Wernersson AS (2018) Critical knowledge gaps and research needs related to the environmental dimensions of antibiotic resistance. Environ Int 117:132–138. https://doi.org/10.1016/j.envint.2018.04.041
Laxminarayan R, Malani A (2007) Extending the cure: policy responses to the growing threat of antibiotic resistance. Earthscan.
Li Y, Zhang S, Zhang W, Xiong W, Ye Q, Hou X, Wang C, Wang P (2019) Life cycle assessment of advanced wastewater treatment processes: Involving 126 pharmaceuticals and personal care products in life cycle inventory. J Environ Manage 238:442–450. https://doi.org/10.1016/j.jenvman.2019.01.118
Limmathurotsakul D, Sandoe JAT, Barrett DC, Corley M, Hsu LY, Mendelson M, Collignon P, Laxminarayan R, Peacock SJ, Howard P (2019) ‘Antibiotic footprint’ as a communication tool to aid reduction of antibiotic consumption. J Antimicrob Chemother 1–6. https://doi.org/10.1093/jac/dkz185
Liu A, Fong A, Becket E, Yuan J, Tamae C, Medrano L, Maiz M, Wahba C, Lee C, Lee K, Tran KP, Yang H, Hoffman RM, Salih A, Miller JH (2011) Selective advantage of resistant strains at trace levels of antibiotics: a simple and ultrasensitive color test for detection of antibiotics and genotoxic agents. Antimicrob Agents Chemother 55:1204–1210. https://doi.org/10.1128/AAC.01182-10
Lorenzo-Toja Y, Alfonsín C, Amores MJ, Aldea X, Marin D, Moreira MT, Feijoo G (2016) Beyond the conventional life cycle inventory in wastewater treatment plants. Sci Total Environ 553:71–82. https://doi.org/10.1016/j.scitotenv.2016.02.073
Mathew AG, Cissell R, Liamthong S (2007) Antibiotic Resistance in Bacteria Associated with Food Animals: A United States Perspective of Livestock Production. Foodborne Pathog Dis 4:115–133. https://doi.org/10.1089/fpd.2006.0066
Morais SA, Delerue-Matos C, Gabarrell X (2013) Accounting for the dissociating properties of organic chemicals in LCIA: an uncertainty analysis applied to micropollutants in the assessment of freshwater ecotoxicity. J Hazard Mater 248–249:461–468. https://doi.org/10.1016/j.jhazmat.2013.01.002
Muñoz I, José Gómez M, Molina-Díaz A, Huijbregts MAJ, Fernández-Alba AR, García-Calvo E (2008) Ranking potential impacts of priority and emerging pollutants in urban wastewater through life cycle impact assessment. Chemosphere 74:37–44. https://doi.org/10.1016/j.chemosphere.2008.09.029
Muñoz I, Rodríguez A, Rosal R, Fernández-Alba AR (2009) Life cycle assessment of urban wastewater reuse with ozonation as tertiary treatment. A focus on toxicity-related impacts. Sci Total Environ 407:1245–1256. https://doi.org/10.1016/j.scitotenv.2008.09.029
Murray CJL, Lopez AD (1994) Quantifying disability: data, methods and results. Bull World Health Organ 72:481–494
Ortiz de García S, García-Encina PA, Irusta-Mata R (2017) The potential ecotoxicological impact of pharmaceutical and personal care products on humans and freshwater, based on USEtoxTM characterization factors. A Spanish case study of toxicity impact scores. Sci Total Environ 609:429–445. https://doi.org/10.1016/j.scitotenv.2017.07.148
Ortiz de García SA, Pinto Pinto G, García-Encina PA, Irusta-Mata R (2014) Ecotoxicity and environmental risk assessment of pharmaceuticals and personal care products in aquatic environments and wastewater treatment plants. Ecotoxicology 23:1517–1533. https://doi.org/10.1007/s10646-014-1293-8
Osman KM, Kappell AD, Elhadidy M, Elmougy F, El-Ghany WAA, Orabi A, Mubarak AS, Dawoud TM, Hemeg HA, Moussa IMI, Hessain AM, Yousef HMY (2018) Poultry hatcheries as potential reservoirs for antimicrobial-resistant Escherichia coli: A risk to public health and food safety. Sci Rep 8:1–14. https://doi.org/10.1038/s41598-018-23962-7
Pérez-Cobas AE, Artacho A, Knecht H, Ferrús ML, Friedrichs A, Ott SJ, Moya A, Latorre A, Gosalbes MJ (2013) Differential effects of antibiotic therapy on the structure and function of human gut microbiota. PLoS One 8. https://doi.org/10.1371/journal.pone.0080201
Posthuma L, Suter II GW, Traas TP (2001) Species sensitivity distributions in ecotoxicology. CRC Press. https://doi.org/10.1201/9781420032314
Potting J, Hauschild MZ (2006) Spatial differentiation in life cycle impact assessment - the EDIP2003 methodology. Int J LCA 1:11–13. https://doi.org/10.1065/lca2006.04.014
Price LB, Koch BJ, Hungate BA (2015) Ominous projections for global antibiotic use in food-animal production. Proc Natl Acad Sci U S A 112:5554–5555. https://doi.org/10.1073/pnas.1505312112
Rahman SM, Eckelman MJ, Onnis-Hayden A, Gu AZ (2018) Comparative life cycle assessment of advanced wastewater treatment processes for removal of chemicals of emerging concern. Environ Sci Technol 52:11346–11358. https://doi.org/10.1021/acs.est.8b00036
Rico A, Jacobs R, Van den Brink PJ, Tello A (2017) A probabilistic approach to assess antibiotic resistance development risks in environmental compartments and its application to an intensive aquaculture production scenario. Environ Pollut 231:918–928. https://doi.org/10.1016/j.envpol.2017.08.079
Rico A, Phu TM, Satapornvanit K, Min J, Shahabuddin AM, Henriksson PJG, Murray FJ, Little DC, Dalsgaard A, Van den Brink PJ (2013) Use of veterinary medicines, feed additives and probiotics in four major internationally traded aquaculture species farmed in Asia. Aquaculture 412–413:231–243. https://doi.org/10.1016/j.aquaculture.2013.07.028
Rizzo L, Manaia C, Merlin C, Schwartz T, Dagot C, Ploy MC, Michael I, Fatta-Kassinos D (2013) Urban wastewater treatment plants as hotspots for antibiotic resistant bacteria and genes spread into the environment: A review. Sci Total Environ 447:345–360. https://doi.org/10.1016/j.scitotenv.2013.01.032
Rico A, Van den Brink PJ (2014) Probabilistic risk assessment of veterinary medicines applied to four major aquaculture species produced in Asia. Sci Total Environ 468–469:630–641. https://doi.org/10.1016/j.scitotenv.2013.08.063
Robinson TP, Bu DP, Carrique-Mas J, Fèvre EM, Gilbert M, Grace D, Hay SI, Jiwakanon J, Kakkar M, Kariuki S, Laxminarayan R, Lubroth J, Magnusson U, Thi Ngoc P, Van Boeckel TP, Woolhouse MEJ (2016) Antibiotic resistance is the quintessential One Health issue. Trans R Soc Trop Med Hyg 110:377–380. https://doi.org/10.1093/trstmh/trw048
Rosenbaum RK, Bachmann TM, Gold LS, Huijbregts MAJ, Jolliet O, Juraske R, Koehler A, Larsen HF, MacLeod M, Margni M, McKone TE, Payet J, Schuhmacher M, Van De Meent D, Hauschild MZ (2008) USEtox - the UNEP-SETAC toxicity model: recommended characterisation factors for human toxicity and freshwater ecotoxicity in life cycle impact assessment. Int J Life Cycle Assess 13:532–546. https://doi.org/10.1007/s11367-008-0038-4
Rosenbaum RK, Huijbregts MAJ, Henderson AD, Margni M, McKone TE, Van De Meent D, Hauschild MZ, Shaked S, Li DS, Gold LS, Jolliet O (2011) USEtox human exposure and toxicity factors for comparative assessment of toxic emissions in life cycle analysis: sensitivity to key chemical properties. Int J Life Cycle Assess 16:710–727. https://doi.org/10.1007/s11367-011-0316-4
Santos LHMLM, Araújo AN, Fachini A, Pena A, Delerue-Matos C, M.C.B.S.M. Montenegro (2010) Ecotoxicological aspects related to the presence of pharmaceuticals in the aquatic environment. J Hazard Mater 175:45–95. https://doi.org/10.1016/j.jhazmat.2009.10.100
Sapkota A, Sapkota AR, Kucharski M, Burke J, McKenzie S, Walker P, Lawrence R (2008) Aquaculture practices and potential human health risks: current knowledge and future priorities. Environ Int 34:1215–1226. https://doi.org/10.1016/j.envint.2008.04.009
Søgaard Jørgensen P, Folke C, Henriksson PJG, Malmros K, Troell M, Zorzet A (2020) Coevolutionary governance of antibiotic and pesticide resistance. Trends Ecol Evol 35:484–494. https://doi.org/10.1016/j.tree.2020.01.011
Stockwell VO, Duffy B (2012) Use of antibiotics in plant agriculture. Rev sci tech Off int Epiz 31:199–210. https://doi.org/10.20506/rst.31.1.2104
Stone JJ, Aurand KR, Dollarhide CR, Jinka R, Thaler RC, Clay DE, Clay SA (2011) Determination of environmental impacts of antimicrobial usage for US Northern Great Plains swine-production facilities: a life-cycle assessment approach. Int J Life Cycle Assess 16:27–39. https://doi.org/10.1007/s11367-010-0241-y
Stone JJ, Dollarhide CR, Jinka R, Thaler RC, Hostetler CE, Clay DE (2010) Life cycle assessment of a modern northern great plains U.S. swine production facility. Environ Eng Sci 27:1009–1018. https://doi.org/10.1089/ees.2010.0051
Surette MD, Wright GD (2017) Lessons from the environmental antibiotic resistome. Annu Rev Microbiol 71:309–329. https://doi.org/10.1146/annurev-micro-090816-093420
Szumilas M (2010) Explaining odds ratios. J Can Acad Child Adolesc Psychiatry 19:227–229 (PMID: 20842279)
Tarpani RRZ, Alfonsín C, Hospido A, Azapagic A (2020) Life cycle environmental impacts of sewage sludge treatment methods for resource recovery considering ecotoxicity of heavy metals and pharmaceutical and personal care products. J Environ Manage 260. https://doi.org/10.1016/j.jenvman.2019.109643
Tarpani RRZ, Azapagic A (2018) Life cycle environmental impacts of advanced wastewater treatment techniques for removal of pharmaceuticals and personal care products (PPCPs) 215:258–272. https://doi.org/10.1016/j.jenvman.2018.03.047
Tello A, Austin B, Telfer TC (2012) Selective pressure of antibiotic pollution on bacteria of importance to public health. Environ Health Perspect 120:1100–1106. https://doi.org/10.1289/ehp.1104650
Terasaki M, Makino M, Tatarazako N, (2009). Acute toxicity of parabens and their chlorinated by-products with Daphnia magna and Vibrio fischeri bioassays. J. Appl. Toxicol. 29:242–247. http://dx.doi.org/10.1002/jat.1402
van Boeckel TP, Brower C, Gilbert M, Grenfell BT, Levin SA, Robinson TP, Teillant A, Laxminarayan R (2015) Global trends in antimicrobial use in food animals. Proc Natl Acad Sci 112:5649–5654. https://doi.org/10.1073/pnas.1503141112
van Bunnik BAD, Woolhouse MEJ (2017) Modelling the impact of curtailing antibiotic usage in food animals on antibiotic resistance in humans. R Soc Open Sci 4. https://doi.org/10.1098/rsos.161067
van den Bogaard AE, Stobberingh EE (1999) Antibiotic usage in animals. Drugs 58:589–607. https://doi.org/10.2165/00003495-199958040-00002
WHO (2014) Antimicrobial resistance: global report on surveillance. World Health Organization
World Health Organization (2019) Critically important antimicrobials for human medicine, 6th revision
Wright GD (2007) The antibiotic resistome: the nexus of chemical and genetic diversity. Nat Rev Microbiol 5:175–186. https://doi.org/10.1038/nrmicro1614
Wypych TP, Marsland BJ (2018) Antibiotics as instigators of microbial dysbiosis: implications for asthma and allergy. Trends Immunol 39:697–711. https://doi.org/10.1016/j.it.2018.02.008
Xiong W, Sun Y, Zhang T, Ding X, Li Y, Wang M, Zeng Z (2015) Antibiotics, Antibiotic Resistance Genes, and Bacterial Community Composition in Fresh Water Aquaculture Environment in China. Microb Ecol 70:425–432. https://doi.org/10.1007/s00248-015-0583-x
Acknowledgements
This work was undertaken as part of the CGIAR Research Programs on Fish Agri-Food Systems (FISH) led by WorldFish and on Climate Change, Agriculture and Food Security (CCAFS).These programs are supported by contributors to the CGIAR Trust Fund.
Funding
P. J. G. Henriksson is partially funded by FORMAS SeaWin project (2016-00227) and partially funded by FORMAS Inequality and the Biosphere project (2020-00454). A. Rico is supported by a Ramón y Cajal grant provided by the Spanish Ministry of Science and Innovation (RYC2019-028132-I). Open access funding provided by Stockholm University.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Matthias Finkbeiner.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to mistakes in the formulas.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nyberg, O., Rico, A., Guinée, J.B. et al. Characterizing antibiotics in LCA—a review of current practices and proposed novel approaches for including resistance. Int J Life Cycle Assess 26, 1816–1831 (2021). https://doi.org/10.1007/s11367-021-01908-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11367-021-01908-y