Abstract
We investigated the associations of plasma neurofilament light (NfL), glial fibrillary acidic protein (GFAP), and total tau (t-tau) with markers of cerebral small vessel disease (SVD) and with incident dementia. We also investigated whether associations of NfL, GFAP, and t-tau with incident dementia were explained by SVD. Data are from a random subsample (n = 1069) of the population-based AGES-Reykjavik Study who underwent brain MRI and in whom plasma NfL, GFAP, and t-tau were measured at baseline (76.1 ± 5.4 years/55.9% women/baseline 2002–2006/follow-up until 2015). A composite SVD burden score was calculated using white matter hyperintensity volume (WMHV), subcortical infarcts, cerebral microbleeds, and large perivascular spaces. Dementia was assessed in a 3-step process and adjudicated by specialists. Higher NfL was associated with a higher SVD burden score. Dementia occurred in 225 (21.0%) individuals. The SVD burden score significantly explained part of the association between NfL and incident dementia. WMHV mostly strongly contributed to the explained effect. GFAP was not associated with the SVD burden score, but was associated with WMHV, and WMHV significantly explained part of the association between GFAP and incident dementia. T-tau was associated with WMHV, but not with incident dementia. In conclusion, the marker most strongly related to SVD is plasma NfL, for which the association with WMHV appeared to explain part of its association with incident dementia. This study suggests that plasma NfL may reflect the contribution of co-morbid vascular disease to dementia. However, the magnitude of the explained effect was relatively small, and further research is required to investigate the clinical implications of this finding.
Similar content being viewed by others
Introduction
Blood-based biomarkers for dementia risk will advance our ability to better understand the heterogeneous pathogenesis underlying dementia and its subtypes [1]. Neurofilament light (NfL), glial fibrillary acidic protein (GFAP), and total tau (t-tau) are promising fluid biomarkers with the potential for identifying pathological processes underlying dementia [1]. Brain NfL is a cytoskeletal component primarily of large myelinated axons that may reflect axonal damage [2, 3]; brain GFAP is an intermediate filament-III protein responsible for the cytoskeletal structure of astrocytes that is upregulated upon astrocyte activation [4, 5]; and brain t-tau is a microtubule-associated protein that regulates cytoskeletal dynamics of neurons that may reflect neurodegeneration [6]. The processes reflected by these fluid biomarkers, including neuronal damage, axon loss, demyelination, and astrogliosis (i.e., astrocyte activation), have also been associated with cerebral vascular damage [7, 8].
Higher plasma levels of NfL [9, 10] and GFAP [9, 11] have consistently been associated with a higher risk of all-cause dementia [10, 11] and Alzheimer’s disease dementia [9,10,11]. Some [9,10,11,12], but not all [10], studies have found an association between higher plasma t-tau levels and a higher risk of all-cause dementia [10, 12] or Alzheimer’s disease dementia [9, 10, 12]. The interpretation of higher circulating levels of NfL, GFAP, and t-tau, however, is still under investigation. Some population-based studies, but not all [13, 14], suggest that these biomarkers may be associated with underlying cerebral small vessel disease (SVD) [9, 15,16,17,18], which could either be co-morbid [19] or contributing to the dementia syndrome [20].
Here, we hypothesize that plasma levels of NfL, GFAP, and t-tau, rather than being causally related to SVD, reflect partly similar or overlapping mechanisms that play an important role in the pathogenesis of dementia. Therefore, we evaluated the associations of plasma NfL, GFAP, and t-tau to SVD markers, including white matter hyperintensity volume (WMHV), subcortical infarcts, cerebral microbleeds, and large perivascular spaces in a large population-based cohort. In addition, we investigated the question as to whether these plasma biomarkers are associated with the total burden of SVD, or individual SVD markers, and whether total or individual SVD burden explained the associations between the plasma biomarkers and incident dementia.
Methods
Study design
We used data from the Age, Gene/Environment Susceptibility (AGES)-Reykjavik Study. The AGES-Reykjavik Study is a longitudinal, population-based cohort study originating from the Reykjavik Study, as described previously in detail [21]. The Reykjavik Study was initiated in 1967 and included individuals born between 1907 and 1935 from the Reykjavik area. Between 2002 and 2006, 5764 randomly chosen surviving participants of the Reykjavik Study were examined for the AGES-Reykjavik Study. Among those participants with an MRI (n = 4811), a random sample of 1200 was selected for the measurement of NfL, GFAP, and t-tau as a part of the MarkVCID project [22]. Characteristics among individuals included in the substudy and those in the original cohort were comparable (Supplementary Table 1). The study was approved by the National Bioethics Committee in Iceland (approval number: VSN-00–063) and by the National Institute on Aging Intramural Institutional Review Board. All participants gave written informed consent.
Plasma biomarkers NfL, GFAP, and t-tau
Fasting blood samples were collected and processed in accordance with established guidelines [23]. Plasma tubes were inverted 5 to 10 times and centrifuged for 10 min at 2000 × g within 1 h of collection. Five hundred microliter aliquots were transferred to polypropylene tubes and samples were places into − 80° freezer within 2 h of collection. Plasma samples were shipped to the Laboratory for Clinical Biochemistry Research at the University of Vermont, which has a strong quality assurance program for assays and is equipped with Simoa HD-1 Analzyer (Quanterix). Plasma levels of NfL, GFAP, and t-tau were measured using the Simoa Neurology 4-Plex Kit on a Simoa HD-1 Analyzer (Quanterix). Analytical ranges and inter-assay coefficients of variance are provided in Supplementary Table 2. A certified laboratory technician, blinded to diagnostic and ethnic groups, performed all assays between November and December 2019 using a single batch of reagents.
Brain MRI measures
All eligible participants were offered high-resolution 1.5 T MRI (Signa Twin-Speed; General Electric Medical Systems). A standardized imaging protocol was used, as described previously [24, 25]. This protocol included the following sequences: 3-dimensional spoiled-gradient recalled T1-weighted, proton density/T2-weighted fast-spin echo, fluid-attenuated inversion recover (FLAIR), and T2a-weighted gradient-echo type echo-planer image (GRE-EPI). All images were acquired to give full brain coverage with slices angled parallel to the anterior commissure-posterior commissure line to give reproducible image views in the oblique-axial plane. We evaluated the following four markers of SVD: WMHV, subcortical infarcts, cerebral microbleeds, and large perivascular spaces. The identification of these markers was made in accordance with expert guidance that provided definitions and neuroimaging standards for markers and consequences of SVD [26]. Total brain parenchyma volume (TBV) and WMHV were computed automatically with a previously described image analysis pipeline [27] and were expressed as the percentage of total intracranial volume. Quality checks were done after tissue classification, as described in detail previously [27]. In brief, quality control consisted of visual inspection of a verification image for each subject including 14 a priori selected slice locations from each of the pulse sequences (T1, PD, T2, FLAIR), evenly distributed across the entire brain in the axial, coronal, and sagittal planes. Unsuccessful tissue classification that could not be rescued by repeated processing or manual editing occurred in 53 cases, mostly due to severe motion artifacts. These scans were excluded from the analytical sample. Other lesions were evaluated by trained radiographers using a standardized protocol [24, 25, 28]. Subcortical infarcts were defined as brain parenchyma defects not extending into the cortex, with a minimum diameter of 4 mm and a signal intensity equal to cerebrospinal fluid on all pulse sequences (T2-weighted, proton density–weighted, and FLAIR), and surrounded by an area of high intensity on FLAIR images and without evidence of hemosiderin on T2a-weighted GRE-EPI sequence [25]. Cerebral microbleeds were defined as focal areas of signal void visible on the T2a-weighted GRE-EPI sequence [24]. Large perivascular spaces were defined as defects on the subcortical area without a rim or area of high signal intensity on FLAIR and without evidence of hemosiderin on the T2a-weighted GRE-EPI sequence [28]. The total number of large perivascular spaces was based on the presence in the basal ganglia complex, along the paths of the perforating lenticulostriate arteries, and in white matter along the paths of the perforating medullary arteries [28]. Information on reproducibility of the process, including the image acquisition and the automatic pipeline, is provided in detail elsewhere [27]. For the volumetric markers, reproducibility was performed in 32 subjects and yielded an interclass correlation 0.98 for both TBV and WMHV [27]. For the other markers, intra- and inter-observer reliability was based on 2 ratings within a 6-month interval and indicated good reliability. Intra-observer reliability was 0.89 and 0.93 for subcortical infarcts [29], 0.75 and 0.73 for cerebral microbleeds [30], and 0.88 and 0.93 for large perivascular spaces [28], respectively. Inter-observer reliability was 0.76 for subcortical infarcts [29], 0.70 for cerebral microbleeds [30], and 0.66 for large perivascular spaces, respectively [28].
Incident all-cause dementia
Incident all-cause dementia was assessed at the follow-up examination (2007–2011) using a 3-step procedure, as described previously [31]. This was the same assessment used for the ascertainment of prevalent all-cause dementia at the baseline examination performed by the same panel of professionals [32]. In brief, the Mini-Mental State Examination and the Digit Symbol Substitution Test were administered to all participants. Individuals who screened positive based on a combination of these tests (< 24 on the Mini-Mental State Examination or < 8 on the Digit Symbol Substitution Test) were administered a diagnostic battery of neuropsychological tests. Based on performance on the Trails B and the Rey Auditory Verbal Learning Test, a subset of these individuals (Auditory Verbal Learning test ≤ 18 or Trails B ≥ 8 for the ratio of time taken for Trails B/Trails A corrected for the number correct: (time trails B/number correct Trails B)/(time Trails A/number correct Trails A)) underwent a proxy interview and were examined by a neurologist. A consensus diagnosis, based on the Diagnostic and Statistical Manual of Mental Disorders 4th edition criteria, was made by a panel of experts including a geriatrician, a neurologist, a neuropsychologist, and a neuroradiologist. In addition, all participants were continuously followed up for dementia diagnosis through vital statistics, hospital records, and the nursing and home-based Resident Assessment Instrument [33]. Follow-up for dementia ended October 4, 2015.
Covariates
Education level (primary, secondary, and college/university) and smoking history (never, former, current) were assessed by questionnaire. Medication use was assessed by questionnaire and from medication bottles brought to the clinic. Blood pressure, body mass index, and lipid levels were measured using standardized protocols [21]. We defined diabetes as a self-reported history of diabetes, use of blood glucose–lowering drugs, or a fasting blood glucose level of ≥ 7.0 mmol/l. Stroke (i.e., symptomatic brain infarct or hemorrhage) prevalent at baseline was obtained from medical records. Incident strokes that occurred between the baseline and follow-up examination were adjudicated by a dementia neurologist, a stroke neurologist, and a neuroradiologist.
Analytical sample
Of the 1200 individuals in this biomarker substudy, 6 participants had missing data on one or more of the plasma biomarkers and another 8 did not have specific MRI images needed for assessment of cerebral microbleeds. Missing data on plasma biomarkers was due to technical reasons, including missing sample (n = 1), insufficient volume available (n = 3), and invalid result (n = 2). In addition, we excluded 10 participants with missing data on covariates. In the remaining 1176 participants, 107 were excluded because of a diagnosis of dementia at baseline (n = 47) or because of missing data on incident dementia (n = 60). The final study sample included 1069 participants (Supplementary Fig. 1). Participants excluded from the biomarker substudy sample were older, less educated, and were more likely to have hypertension or type 2 diabetes compared to those included in the analysis (Supplementary Table 3).
Statistical analysis
We summarized the four markers of SVD into a composite sum score (range 0–4) to reflect burden of SVD (SVD burden score) as done previously [34]. One point per SVD marker was assigned based on the following cut-offs: for WMHV highest quartile versus lowest three quartiles; and for subcortical infarcts, cerebral microbleeds, and large perivascular spaces, presence (i.e., ≥ 1 lesion(s)) versus absence). In all analyses, the SVD burden score was analyzed on a continuous scale to enhance the statistical power of our analysis, as done previously [34, 35]. We also evaluated the SVD burden score on an ordinal scale. Plasma biomarkers were transformed using a natural logarithm (i.e., base-e log) to normalize their skewed distribution.
The statistical analysis proceeded in three stages. First, to evaluate the relation between plasma biomarkers and the SVD burden score, we used linear regression to estimate regression coefficients (betas) and 95% confidence intervals (95%CIs) for the association of plasma NfL, GFAP, and t-tau with the SVD burden score. Second, to evaluate the association between plasma biomarkers and incident dementia, we used Cox regression to estimate hazard ratios (HRs) and 95% CIs for the association of plasma NfL, GFAP, and t-tau with incident dementia using time-in-study as the time scale. Follow-up time was calculated from the AGES-Reykjavik baseline examination (2002–2006) to incidence of dementia, death, or end of follow-up (October 4, 2015), whichever came first. The proportional hazard assumption was assessed by visual inspection of Kaplan–Meier curves (Supplementary Fig. 2). Third, to investigate whether the SVD burden score explained the association of plasma NfL, GFAP, and t-tau with incident dementia (if any), we entered the SVD burden score as a covariate in the biomarker-dementia models. We did not consider the SVD burden score to be on the putative causal pathway of the plasma biomarkers leading to dementia, and we, therefore, did not do a formal mediation analysis. To quantify the degree to which the SVD burden score attenuated the association of plasma biomarkers with incident dementia, we calculated the explained effects. The explained effects were calculated as the multiplied effects of plasma biomarkers and brain MRI markers and brain MRI markers and incident dementia, adjusted for the plasma biomarkers [36]. The calculation of the explained effect is summarized in Supplementary Fig. 3. We used bootstrapping (10,000 samples) to calculate bias-corrected 95% CIs for the explained effects.
All analyses were adjusted for age and sex (model 1) and additionally for education level, smoking history, diabetes status, body mass index, total cholesterol-to-HDL cholesterol ratio, use of lipid-modifying medication, systolic blood pressure, and use of antihypertensive medication (model 2). These covariates were selected on the basis of their biological plausibility, since they are known to be associated with SVD [37] or dementia [38]. Data on the association between plasma NfL, GFAP, and t-tau and the covariates included in model 2 is still limited [39]. However, these covariates are known to be associated with the neurodegenerative mechanisms that are presumed to be reflected by plasma levels of NfL, GFAP, and t-tau [40, 41].
We performed several sensitivity analyses. First, we repeated the analyses for each of the individual SVD markers separately. Second, to minimize potential confounding or mediating effects by TBV or stroke, we repeated the analysis additionally adjusting for TBV and baseline stroke or incident stroke during follow-up. Third, to investigate the effect of the definition of WMHV, we evaluated WMHV expressed on a continuous scale and WMHV expressed as higher versus lower than the median.
Results
The mean age of the participants at baseline was 76.1 (SD: 5.4) and 55.9% were female. Overall, 21.0% of the participants developed incident dementia after a mean follow-up of 8.7 (SD: 3.5) years. Table 1 shows the characteristics of the study population and by tertiles of plasma NfL. Characteristics by tertiles of plasma GFAP and t-tau are provided in the Supplementary Material (Supplementary Tables 4 and 5). In general, participants with the highest compared to the lowest two tertiles of plasma NfL were older, more often female, had a worse cardiovascular risk profile and were more likely to have a stroke (Table 1). For instance, there was an increase in age from the lowest tertile to the highest tertile of plasma NfL.
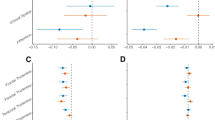
A higher plasma NfL and a higher t-tau were associated with a higher SVD burden score (Fig. 1). A higher plasma NfL and GFAP were associated with a higher risk of dementia after adjustment for potential confounders (Fig. 2, model 2).
Associations between plasma NfL, GFAP, and t-tau and the SVD burden scorea. Betas are expressed per natural log-transformed pg/ml higher plasma NfL, GFAP, or t-tau. Model 1 adjusted for age and sex. Model 2 additionally adjusted for education level, diabetes status, smoking history, body mass index, total cholesterol-to-HDL cholesterol ratio, use of lipid-modifying medication, systolic blood pressure, and use of antihypertensive medication. Abbreviations: SVD, cerebral small vessel disease; NfL, neurofilament light; GFAP, glial fibrillary acidic protein; t-tau, total tau. aSVD burden score was calculated by assigning one point per cerebral small vessel disease marker based on the following cut-offs (range 0–4): WMHV highest quartile vs lowest three quartiles, and for subcortical infarcts, cerebral microbleeds, and large perivascular spaces presence vs absence
Associations between plasma NfL, GFAP, and t-tau and incident dementia with and without adjustment for the SVD burden scorea. Hazard ratios for incident dementia are expressed per natural log-transformed pg/ml higher plasma NfL, GFAP, or t-tau. Model 1 adjusted for age and sex. Model 2 additionally adjusted for education level, diabetes status, smoking history, body mass index, total cholesterol-to-HDL cholesterol ratio, use of lipid-modifying medication, systolic blood pressure, and use of antihypertensive medication. Models 1 and 2 represent the total effect, and model 2 + adjustment for the SVD burden score represents the direct effect. Total and direct effect are defined in Supplementary Fig. 3. Abbreviations: NfL, neurofilament light; GFAP, glial fibrillary acidic protein; t-tau, total tau; SVD, cerebral small vessel disease. aSVD burden score was calculated by assigning one point per cerebral small vessel disease marker based on the following cut-offs (range 0–4): WMHV highest quartile vs lowest three quartiles, and for subcortical infarcts, cerebral microbleeds, and large perivascular spaces presence vs absence
When we additionally adjusted the association between plasma NfL and incident dementia for the SVD burden score, the association attenuated but remained statistically significant (Fig. 2, model 3). The SVD burden score statistically significantly explained part of the association between plasma NfL and dementia (HR 1.07 (95% CI 1.02; 1.15)) (Table 2). The association between plasma GFAP and incident dementia was not explained by the SVD burden score (Fig. 2, model 3, and Table 2).
Sensitivity analysis
The analyses with the SVD burden score modelled on an ordinal scale showed a linear increase for the risk of dementia for a higher SVD burden score (Supplementary Table 6). In addition, plasma NfL, but not GFAP and t-tau, increased linearly for a higher SVD burden score (Supplementary Table 7). The non-linear association between plasma GFAP and t-tau and the SVD burden score is in accordance with the non-significant finding of the explained effect by the SVD burden score of the associations between plasma GFAP and t-tau and incident dementia. Additionally adjusting the association between the plasma biomarkers and incident dementia for the SVD burden score on an ordinal scale yielded results similar to those obtained when we additionally adjusted for the SVD burden score on a continuous scale (Supplementary Fig. 4). A higher plasma NfL was associated with a higher WMHV and presence of subcortical infarcts; only WMHV explained part of the association of plasma NfL with incident dementia (Supplementary Fig. 5 and 6 and Supplementary Table 8). A higher plasma GFAP was only associated with WMHV, and similar to plasma NfL, WMHV explained part of the association of plasma GFAP with dementia (Supplementary Figs. 5 and 6 and Supplementary Table 8). Plasma t-tau was associated with a higher WMHV, but not with any of the other markers of SVD (Supplementary Fig. 5). Results were similar when we additionally adjusted for TBV or prevalent or incident stroke (Supplementary Fig. 7 to 10 and Supplementary Table 9 and 10). Results were similar using WMHV on a continuous scale, or using WMHV expressed as higher versus lower than the median, instead of comparing those in the highest quartile of WMHV to those in the lowest three quartiles (Supplementary Figs. 11 and 12 and Supplementary Tables 11).
Discussion
In this study, a higher plasma NfL was associated with a higher total SVD burden score. The SVD burden score statistically significantly explained part of the association between plasma NfL and incident dementia. Of the different components of the SVD burden score, WMHV was the strongest component as it drove the attenuation of the association between NfL and incident dementia. Plasma GFAP was not associated with the SVD burden score, but was associated with WMHV, which significantly explained part of the association between GFAP and incident dementia. Plasma t-tau was not linearly associated with a higher SVD burden score, but was associated with WMHV. Plasma t-tau was not associated with incident dementia. Together these results suggest that these plasma biomarkers are differentially associated with markers of SVD and burden of SVD. The biomarker most strongly related to SVD is plasma NfL whose association with WMHV appeared to partly explain its association with incident dementia. Our study also suggests that “burden of SVD” is less important as an explaining factor, as having subcortical infarcts, cerebral microbleeds, and large perivascular spaces did not contribute significantly to the NfL–dementia association.
Most data on SVD comes from studies on WMHV. With the exception of one study [16] (n = 1362), these studies were relatively small (n < 300) [15,16,17] or did not adjust for cardiovascular risk factors [9, 13, 15, 17]. Consistent with our study findings, most of these studies (including the largest study [16]), but not all [9, 13], found that WMHV was associated with a higher plasma NfL [9, 15, 16], GFAP [16, 17], but not with t-tau [9, 13, 16]. Consistent with our findings, cerebral microbleeds measured in 3 community-based studies of individuals with an average age around 75 year and with sample sizes n = 712 or less were not associated with plasma NfL [14, 15], GFAP [17], or t-tau [14]. One large study including 3680 individuals with an average age of 55 years [18] did find a significant association of t-tau with cerebral microbleeds. The reasons for this inconsistent finding may reflect the younger age of that cohort compared to the other cohorts, the larger sample size or differences in MRI sequences. We extend the results of these previous studies in several ways: we compared and took account of multiple vascular lesions in the brain and examined the contribution of the burden of SVD to the association of plasma NfL, GFAP, and t-tau with incident dementia.
This study suggests that plasma levels of NfL, but not GFAP, may reflect the contribution of co-morbid vascular disease in the brain to dementia. Plasma GFAP may potentially be related to other mechanisms that have direct neurotoxic effects that were not evaluated in the present study, including amyloid pathology [42, 43]. Activated astrocytes, with high expression of GFAP, are found to surround amyloid plaques in Alzheimer’s disease [5]. Other mechanisms that might play a role are large vessel disease [44] and oxidative stress [45]. Additionally, our results suggest that plasma NfL, GFAP, and t-tau are differentially associated with markers of SVD. Possibly, these plasma biomarkers may be more likely to reflect diffuse cerebral damage due to white matter hyperintensities as compared to the focal damage due to subcortical infarcts, cerebral microbleeds, and large perivascular spaces [8]. However, this study is the first to explore multiple vascular lesions in the brain in relation to plasma NfL, GFAP, and t-tau, and the specific clinical consequences of the SVD lesion types are not fully understood. In addition, the magnitude of the explained effects was relatively small, and therefore, the clinical implications of these biomarkers in identifying the pathological processes underlying dementia are unclear. Further study is needed to clarify these issues.
In this study, plasma t-tau was associated with WMHV, but we did not observe an association between plasma t-tau and incident dementia. This may suggest that plasma t-tau may be a marker of WMHV, but that it is not specific to the neuropathology underlying dementia. The role of plasma t-tau as a biomarker of dementia risk is less clearly established than those of plasma NfL and GFAP. Consistent with our study findings, a previous population-based study [10] that included 4444 individuals did not find an association between plasma t-tau and incident dementia. In contrast, two other studies (n = 1453 [12] and n = 1327 [9]) found an association between a higher plasma t-tau and a higher risk of dementia. The reasons for these inconsistent findings are not fully clear, but may be due to differences in adjustment for potential confounders (adjustment for sociodemographic factors only [9] vs extensive adjustment for sociodemographic and cardiovascular risk factors [10, 12]). Furthermore, it is possible that plasma levels of t-tau may be less useful as markers for dementia risk because it may not accurately reflect levels in the cerebrospinal fluid, as suggested previously [46, 47]. This may be due to peripheral degradation of t-tau into undetectable fragments [46], or, alternatively, secretion of t-tau in other organs than the brain, including the kidney and skeletal muscle [47].
Key strengths of this study include the large population-based sample, the comprehensive assessment of multiple biomarkers measured in plasma and on brain MRI, and the extensive characterization of participants, which enabled us to adjust for a series of potential confounders.
This study has several limitations. First, the plasma biomarkers NfL, GFAP, and t-tau were measured at the baseline examination only, and, therefore, we cannot investigate the temporality of levels of these plasma biomarkers. Possibly, accumulative data about the plasma levels of these biomarkers across the life course may be a stronger determinant of dementia risk, and may be more strongly related to the total burden of SVD. Second, although we adjusted for a large series of potential confounders, we cannot exclude the possibility of residual confounding. For example, it is possible that SVD explains part of the association between plasma NfL and incident dementia because plasma levels of NfL are also known to increase with normal aging [3]. Third, some of the biomarkers investigated may be more strongly related to pathology specific to dementia subtypes (i.e., Alzheimer’s disease dementia or vascular dementia). However, we did not investigate associations with specific dementia type, and this requires further study. In addition, plasma phosphorylated tau (p-tau) and amyloid-beta may be more specific to the brain pathology in dementia as compared to plasma NfL, GFAP, and t-tau [6], but these biomarkers were not available in the present study. Fourth, individuals excluded in the present study due to missing data were older, less educated, and had a worse cardiovascular risk profile compared to those included in the analysis. This may have led to an underestimation of the reported findings due to lower variation in biomarkers and lower incidence of dementia. Fifth, the study population consisted mostly of Caucasian individuals, and the results may therefore not apply to other ethnic groups. Sixth, in this study, some cases of incident dementia were identified through medical records and vital statistics. We cannot exclude the possibility that this approach had a lower sensitivity and specificity compared to the 3-step procedure used during the clinical baseline and follow-up examination and the nursing and home-based Resident Assessment Instrument.
In conclusion, the plasma biomarker most strongly related to SVD is NfL whose association with WMHV appeared to partly explain its association with incident dementia. This study suggests that plasma NfL may reflect the contribution to dementia of co-morbid vascular disease, particularly of WMHV. However, the magnitude of the explained effect was relatively small, and further research is required to investigate the clinical implications of these findings.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Teunissen CE, Verberk IMW, Thijssen EH, Vermunt L, Hansson O, Zetterberg H, van der Flier WM, Mielke MM, Del Campo M. Blood-based biomarkers for Alzheimer’s disease: towards clinical implementation. Lancet Neurol. 2022;21:66–77. https://doi.org/10.1016/S1474-4422(21)00361-6.
Khalil M, Teunissen CE, Otto M, Piehl F, Sormani MP, Gattringer T, Barro C, Kappos L, Comabella M, Fazekas F, et al. Neurofilaments as biomarkers in neurological disorders. Nat Rev Neurol. 2018;14:577–89. https://doi.org/10.1038/s41582-018-0058-z.
Gaetani L, Blennow K, Calabresi P, Di Filippo M, Parnetti L, Zetterberg H. Neurofilament light chain as a biomarker in neurological disorders. J Neurol Neurosurg Psychiatry. 2019;90:870–81. https://doi.org/10.1136/jnnp-2018-320106.
Middeldorp J, Hol EM. GFAP in health and disease. Prog Neurobiol. 2011;93:421–43. https://doi.org/10.1016/j.pneurobio.2011.01.005.
Yang Z, Wang KK. Glial fibrillary acidic protein: from intermediate filament assembly and gliosis to neurobiomarker. Trends Neurosci. 2015;38:364–74. https://doi.org/10.1016/j.tins.2015.04.003.
Jack CR Jr, Bennett DA, Blennow K, Carrillo MC, Dunn B, Haeberlein SB, Holtzman DM, Jagust W, Jessen F, Karlawish J, et al. NIA-AA Research Framework: toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 2018;14:535–62. https://doi.org/10.1016/j.jalz.2018.02.018.
van Sloten TT, Sedaghat S, Carnethon MR, Launer LJ, Stehouwer CDA. Cerebral microvascular complications of type 2 diabetes: stroke, cognitive dysfunction, and depression. Lancet Diabetes Endocrinol. 2020;8:325–36. https://doi.org/10.1016/S2213-8587(19)30405-X.
Wardlaw JM, Smith C, Dichgans M. Small vessel disease: mechanisms and clinical implications. Lancet Neurol. 2019;18:684–96. https://doi.org/10.1016/S1474-4422(19)30079-1.
Rajan KB, Aggarwal NT, McAninch EA, Weuve J, Barnes LL, Wilson RS, DeCarli C, Evans DA. Remote blood biomarkers of longitudinal cognitive outcomes in a population study. Ann Neurol. 2020;88:1065–76. https://doi.org/10.1002/ana.25874.
de Wolf F, Ghanbari M, Licher S, McRae-McKee K, Gras L, Weverling GJ, Wermeling P, Sedaghat S, Ikram MK, Waziry R, et al. Plasma tau, neurofilament light chain and amyloid-beta levels and risk of dementia; a population-based cohort study. Brain. 2020;143:1220–32. https://doi.org/10.1093/brain/awaa054.
Gonzales MM, Wiedner C, Wang CP, Liu Q, Bis JC, Li Z, Himali JJ, Ghosh S, Thomas EA, Parent DM, et al. A population-based meta-analysis of circulating GFAP for cognition and dementia risk. Ann Clin Transl Neurol. 2022;9:1574–85. https://doi.org/10.1002/acn3.51652.
Pase MP, Beiser AS, Himali JJ, Satizabal CL, Aparicio HJ, DeCarli C, Chene G, Dufouil C, Seshadri S. Assessment of plasma total tau level as a predictive biomarker for dementia and related endophenotypes. JAMA Neurol. 2019;76:598–606. https://doi.org/10.1001/jamaneurol.2018.4666.
Marks JD, Syrjanen JA, Graff-Radford J, Petersen RC, Machulda MM, Campbell MR, Algeciras-Schimnich A, Lowe V, Knopman DS, Jack CR Jr, et al. Comparison of plasma neurofilament light and total tau as neurodegeneration markers: associations with cognitive and neuroimaging outcomes. Alzheimers Res Ther. 2021;13:199. https://doi.org/10.1186/s13195-021-00944-y.
McCarter SJ, Lesnick TG, Lowe VJ, Rabinstein AA, Przybelski SA, Algeciras-Schimnich A, Ramanan VK, Jack CR, Petersen RC, Knopman DS, et al. Association between plasma biomarkers of amyloid, tau, and neurodegeneration with cerebral microbleeds. J Alzheimers Dis. 2022;87:1537–47. https://doi.org/10.3233/JAD-220158.
Dittrich A, Ashton NJ, Zetterberg H, Blennow K, Simren J, Geiger F, Zettergren A, Shams S, Machado A, Westman E, et al. Plasma and CSF NfL are differentially associated with biomarker evidence of neurodegeneration in a community-based sample of 70-year-olds. Alzheimers Dement (Amst). 2022;14:e12295. https://doi.org/10.1002/dad2.12295.
Fohner AE, Bartz TM, Tracy RP, Adams HHH, Bis JC, Djousse L, Satizabal CL, Lopez OL, Seshadri S, Mukamal KJ, et al. Association of serum neurofilament light chain concentration and MRI findings in older adults: the cardiovascular health study. Neurology. 2022;98:e903–11. https://doi.org/10.1212/WNL.0000000000013229.
Shir D, Graff-Radford J, Hofrenning EI, Lesnick TG, Przybelski SA, Lowe VJ, Knopman DS, Petersen RC, Jack CR Jr, Vemuri P, et al. Association of plasma glial fibrillary acidic protein (GFAP) with neuroimaging of Alzheimer’s disease and vascular pathology. Alzheimers Dement (Amst). 2022;14:e12291. https://doi.org/10.1002/dad2.12291.
Romero JR, Demissie S, Beiser A, Himali JJ, DeCarli C, Levy D, Seshadri S. Relation of plasma beta-amyloid, clusterin, and tau with cerebral microbleeds: Framingham Heart Study. Ann Clin Transl Neurol. 2020;7:1083–91. https://doi.org/10.1002/acn3.51066.
Zlokovic BV, Gottesman RF, Bernstein KE, Seshadri S, McKee A, Snyder H, Greenberg SM, Yaffe K, Schaffer CB, Yuan C, et al. Vascular contributions to cognitive impairment and dementia (VCID): a report from the 2018 National Heart, Lung, and Blood Institute and National Institute of Neurological Disorders and Stroke Workshop. Alzheimers Dement. 2020;16:1714–33. https://doi.org/10.1002/alz.12157.
Rensma SP, van Sloten TT, Launer LJ, Stehouwer CDA. Cerebral small vessel disease and risk of incident stroke, dementia and depression, and all-cause mortality: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2018;90:164–73. https://doi.org/10.1016/j.neubiorev.2018.04.003.
Harris TB, Launer LJ, Eiriksdottir G, Kjartansson O, Jonsson PV, Sigurdsson G, Thorgeirsson G, Aspelund T, Garcia ME, Cotch MF, et al. Age, Gene/Environment Susceptibility-Reykjavik Study: multidisciplinary applied phenomics. Am J Epidemiol. 2007;165:1076–87. https://doi.org/10.1093/aje/kwk115.
Wilcock D, Jicha G, Blacker D, Albert MS, D’Orazio LM, Elahi FM, Fornage M, Hinman JD, Knoefel J, Kramer J, et al. MarkVCID cerebral small vessel consortium: I. Enrollment, clinical, fluid protocols. Alzheimers Dement. 2021;17:704–15. https://doi.org/10.1002/alz.12215.
O’Bryant SE, Gupta V, Henriksen K, Edwards M, Jeromin A, Lista S, Bazenet C, Soares H, Lovestone S, Hampel H, et al. Guidelines for the standardization of preanalytic variables for blood-based biomarker studies in Alzheimer’s disease research. Alzheimers Dement. 2015;11:549–60. https://doi.org/10.1016/j.jalz.2014.08.099.
Sveinbjornsdottir S, Sigurdsson S, Aspelund T, Kjartansson O, Eiriksdottir G, Valtysdottir B, Lopez OL, van Buchem MA, Jonsson PV, Gudnason V, et al. Cerebral microbleeds in the population based AGES-Reykjavik study: prevalence and location. J Neurol Neurosurg Psychiatry. 2008;79:1002–6. https://doi.org/10.1136/jnnp.2007.121913.
Scher AI, Gudmundsson LS, Sigurdsson S, Ghambaryan A, Aspelund T, Eiriksdottir G, van Buchem MA, Gudnason V, Launer LJ. Migraine headache in middle age and late-life brain infarcts. JAMA. 2009;301:2563–70. https://doi.org/10.1001/jama.2009.932.
Wardlaw JM, Smith EE, Biessels GJ, Cordonnier C, Fazekas F, Frayne R, Lindley RI, O’Brien JT, Barkhof F, Benavente OR, et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. 2013;12:822–38. https://doi.org/10.1016/S1474-4422(13)70124-8.
Sigurdsson S, Aspelund T, Forsberg L, Fredriksson J, Kjartansson O, Oskarsdottir B, Jonsson PV, Eiriksdottir G, Harris TB, Zijdenbos A, et al. Brain tissue volumes in the general population of the elderly: the AGES-Reykjavik study. Neuroimage. 2012;59:3862–70. https://doi.org/10.1016/j.neuroimage.2011.11.024.
Ding J, Sigurethsson S, Jonsson PV, Eiriksdottir G, Charidimou A, Lopez OL, van Buchem MA, Guethnason V, Launer LJ. Large perivascular spaces visible on magnetic resonance imaging, cerebral small vessel disease progression, and risk of dementia: the Age. Gene/Environment Susceptibility-Reykjavik Study JAMA Neurol. 2017;74:1105–12. https://doi.org/10.1001/jamaneurol.2017.1397.
Sigurdsson S, Aspelund T, Kjartansson O, Gudmundsson E, Jonsson PV, van Buchem MA, Gudnason V, Launer LJ. Cerebrovascular risk-factors of prevalent and incident brain infarcts in the general population: the AGES-Reykjavik Study. Stroke. 2022;53:1199–206. https://doi.org/10.1161/STROKEAHA.121.034130.
Ding J, Sigurdsson S, Garcia M, Phillips CL, Eiriksdottir G, Gudnason V, van Buchem MA, Launer LJ. Risk factors associated with incident cerebral microbleeds according to location in older people: the Age, Gene/Environment Susceptibility (AGES)-Reykjavik Study. JAMA Neurol. 2015;72:682–8. https://doi.org/10.1001/jamaneurol.2015.0174.
Vonk JMJ, Greving JP, Gudnason V, Launer LJ, Geerlings MI. Dementia risk in the general population: large-scale external validation of prediction models in the AGES-Reykjavik study. Eur J Epidemiol. 2021;36:1025–41. https://doi.org/10.1007/s10654-021-00785-x.
Saczynski JS, Sigurdsson S, Jonsdottir MK, Eiriksdottir G, Jonsson PV, Garcia ME, Kjartansson O, Lopez O, van Buchem MA, Gudnason V, et al. Cerebral infarcts and cognitive performance: importance of location and number of infarcts. Stroke. 2009;40:677–82. https://doi.org/10.1161/STROKEAHA.108.530212.
Morris JN, Hawes C, Fries BE, Phillips CD, Mor V, Katz S, Murphy K, Drugovich ML, Friedlob AS. Designing the national resident assessment instrument for nursing homes. Gerontologist. 1990;30:293–307. https://doi.org/10.1093/geront/30.3.293.
Rensma SP, van Sloten TT, Ding J, Sigurdsson S, Stehouwer CDA, Gudnason V, Launer LJ. Type 2 diabetes, change in depressive symptoms over time, and cerebral small vessel disease: longitudinal data of the AGES-Reykjavik Study. Diabetes Care. 2020;43:1781–7. https://doi.org/10.2337/dc19-2437.
Zhou TL, Rensma SP, van der Heide FCT, Henry RMA, Kroon AA, Houben A, Jansen JFA, Backes WH, Berendschot T, Schouten J, et al. Blood pressure variability and microvascular dysfunction: the Maastricht Study. J Hypertens. 2020;38:1541–50. https://doi.org/10.1097/HJH.0000000000002444.
Rijnhart JJM, Twisk JWR, Eekhout I, Heymans MW. Comparison of logistic-regression based methods for simple mediation analysis with a dichotomous outcome variable. BMC Med Res Methodol. 2019;19:19. https://doi.org/10.1186/s12874-018-0654-z.
Hakim AM. Small vessel disease. Front Neurol. 2019;10:1020. https://doi.org/10.3389/fneur.2019.01020.
Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, Brayne C, Burns A, Cohen-Mansfield J, Cooper C, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396:413–46. https://doi.org/10.1016/S0140-6736(20)30367-6.
Barro C, Chitnis T, Weiner HL. Blood neurofilament light: a critical review of its application to neurologic disease. Ann Clin Transl Neurol. 2020;7:2508–23. https://doi.org/10.1002/acn3.51234.
Song R, Xu H, Dintica CS, Pan KY, Qi X, Buchman AS, Bennett DA, Xu W. Associations between cardiovascular risk, structural brain changes, and cognitive decline. J Am Coll Cardiol. 2020;75:2525–34. https://doi.org/10.1016/j.jacc.2020.03.053.
Lamar M, Boots EA, Arfanakis K, Barnes LL, Schneider JA. Common brain structural alterations associated with cardiovascular disease risk factors and Alzheimer’s dementia: future directions and implications. Neuropsychol Rev. 2020;30:546–57. https://doi.org/10.1007/s11065-020-09460-6.
Stocker H, Beyer L, Perna L, Rujescu D, Holleczek B, Beyreuther K, Stockmann J, Schottker B, Gerwert K, Brenner H. Association of plasma biomarkers, p-tau181, glial fibrillary acidic protein, and neurofilament light, with intermediate and long-term clinical Alzheimer’s disease risk: Results from a prospective cohort followed over 17 years. Alzheimers Dement. 2022. https://doi.org/10.1002/alz.12614.
Scheltens P, De Strooper B, Kivipelto M, Holstege H, Chetelat G, Teunissen CE, Cummings J, van der Flier WM. Alzheimer’s disease. Lancet. 2021;397:1577–90. https://doi.org/10.1016/S0140-6736(20)32205-4.
Heshmatollah A, Fani L, Koudstaal PJ, Ghanbari M, Ikram MA, Ikram MK. Plasma beta-amyloid, total-tau, and neurofilament light hain levels and the risk of stroke: a prospective population-based study. Neurology. 2022;98:e1729–37. https://doi.org/10.1212/WNL.0000000000200004.
Teleanu DM, Niculescu AG, Lungu II, Radu CI, Vladacenco O, Roza E, Costachescu B, Grumezescu AM, Teleanu RI. An overview of oxidative stress, neuroinflammation, and neurodegenerative diseases. Int J Mol Sci. 2022;23(11):593. https://doi.org/10.3390/ijms23115938.
Mattsson N, Zetterberg H, Janelidze S, Insel PS, Andreasson U, Stomrud E, Palmqvist S, Baker D, Tan Hehir CA, Jeromin A, et al. Plasma tau in Alzheimer disease. Neurology. 2016;87:1827–35. https://doi.org/10.1212/WNL.0000000000003246.
Planche V, Bouteloup V, Pellegrin I, Mangin JF, Dubois B, Ousset PJ, Pasquier F, Blanc F, Paquet C, Hanon O, et al. Validity and performance of blood biomarkers for Alzheimer disease to predict dementia risk in a large clinic-based cohort. Neurology. 2022. https://doi.org/10.1212/WNL.0000000000201479.
Funding
The AGES-Reykjavik Study was supported by the Icelandic Heart Association, Intramural Research Program at the National Institute on Aging (grant numbers N01-AG-12100 and HHSN271201200022C), the Althingi (the Icelandic Parliament), and the Icelandic Centre for Research (RANNIS) (grant number 141101–051). The measurement of fluid markers was funded by the National Institute of Neurological Disorders and Stroke under the MarkVCID consortium (UH3 NS100605, UF1 NS125513). TVS is supported by the Netherlands Organization for Health Research and Development (ZonMW) Veni research grant (grant number 916.19.074) and a Diabetes Fonds Junior Fellowship grant (grant number 2021.81.004), and TVS and AVG are supported by a Dutch Heart Foundation research grant (grant number 2018T025). CLS is supported by the National Institute on Ageing (P30 AG066546, R01 AG059727).
Author information
Authors and Affiliations
Contributions
AVG and TVS developed the statistical analysis. AVG, TVS, and LL drafted the manuscript. CS, SS, RT, VG, and LL contributed to the design of the study, data collection, and assessments. All authors critically reviewed the manuscript for important intellectual content and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
van Gennip, A.C.E., Satizabal, C.L., Tracy, R.P. et al. Associations of plasma NfL, GFAP, and t-tau with cerebral small vessel disease and incident dementia: longitudinal data of the AGES-Reykjavik Study. GeroScience 46, 505–516 (2024). https://doi.org/10.1007/s11357-023-00888-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11357-023-00888-1