Abstract
Fine particulate matter (PM2.5) has been the primary air pollutant and the fourth leading risk factor for disease and death in the world. Exposure to PM2.5 is related to activation of the NOD-like receptor family pyrin domain containing 3 (NLRP3) inflammasome, but the mechanism of PM2.5 affecting the NLRP3 inflammasome is still unclear. Previous studies have shown that PM2.5 can cause alterations in adenosine triphosphate (ATP), and an increase in extracellular ATP and a decrease in intracellular ATP can trigger the activation process of the NLRP3 inflammasome. Therefore, we emphasize that ATP changes may be the central link and key mechanism of PM2.5 exposure that activates the NLRP3 inflammasome. This review briefly elucidates and summarizes how PM2.5 acts on ATP and subsequently further impacts the NLRP3 inflammasome. Investigation of ATP changes due to exposure to PM2.5 may be essential to regulate NLRP3 inflammasome activation and treat inflammation-related diseases such as coronavirus disease 2019 (COVID-19).
Graphical abstract

Similar content being viewed by others
Introduction
Fine particulate (PM2.5) has become the main contributor to air pollution and the fourth leading risk factor for death and disability in the world (GBD C 2020; WHO 2016; Xu et al. 2020). PM2.5 compositions mainly include inorganic salts, carbon-containing substances such as persistent organic pollutants, metal elements, including lead and cadmium, which are adsorbed and adhered to the surface (Samek et al. 2017; Xie et al. 2019; Zhang et al. 2013); Zhao et al. 2019). The proportion of each component in PM2.5 is related to factors such as source, region, climate, season, and formation pattern (Samek et al. 2017; Xie et al. 2019; Zhang et al. 2013); Zhao et al. 2019). Furthermore, they can absorb a large number of toxic and harmful substances, such as heavy metals and persistent organic pollutants due to their large specific surface area and deposit in the respiratory tract and pass through the alveoli into the blood system due to their small size, and subsequently disperse and accumulate in various tissues and organs of the human body through the circulatory system (Shou et al. 2019; Sun et al. 2020; Wei and Tang 2018). Therefore, the toxicity and health effects of PM2.5 depend not only on the components and concentrations, but also on their unique physical and chemical properties, such as a Fenton reaction of heavy metals that can produce intracellular reactive oxygen species (ROS), and population susceptibility (Zeng et al. 2020).
The NOD-like receptor family pyrin domain containing 3 (NLRP3) inflammasome is a complex composed of NLRP3, apoptosis-associated speck-like protein (ASC) and inactive caspase-1 precursor, which can be activated by a series of substances such as PM2.5 and adenosine triphosphate (ATP, an intracellular basic energy unit), and biological processes including potassium (K+) efflux, calcium (Ca2+) and sodium (Na+) influx, mitochondrial damage, and lysosome destabilization and rupture, etc. (Liu et al. 2020). Activation of the NLRP3 inflammasome is the key innate immune pathway responsible for producing active caspase-1 and interleukin-1β(IL-1β) involved in the sterile inflammatory response (Liu et al. 2018a). Mitochondria as the center of biological energy of cells plays an important role in airborne particulate matter-induced immunotoxicity (Sharma et al. 2021). Although several studies have suggested that there is an association between PM2.5 exposure and NLRP3 inflammasome activation, the underlying mechanisms are still unknown (Cheng et al. 2020; Duan et al. 2019; Jia et al. 2021; Niu et al. 2021; Wang et al. 2020a). Furthermore, several reports showed that there is an association between PM2.5 exposure and decreased intracellular ATP (Duan et al. 2019; Jin et al. 2019a; Jin et al. 2019b; Ning et al. 2019). In addition, extracellular ATP has been confirmed as an activator of the NLRP3 inflammasome (Hudson et al. 2019; Jiang et al. 2017; Wang et al. 2013). Therefore, ATP may mediate the relationship between PM2.5 exposure and activation of the NLRP3 inflammasome. However, there is a critical gap in understanding the mechanism referring to PM2.5 exposure and activation of the NLRP3 inflammasome.
In this review, we briefly summarize the essential potential role of ATP in the NLRP3 inflammasome activation process triggered by exposure to PM2.5(Fig. 1 and Table 1). This study may shed light on the strategy to treat PM2.5-induced ATP-dependent NLRP3 inflammasome-related inflammatory response and diseases (Fig. 2).
The mediation role of ATP alterations in the association between exposure to PM2.5 and activation of the NLRP3 inflammasome. Exposure to PM2.5 can induce ATP alterations. In addition, both PM2.5 exposure and ATP alteration can activate the NLRP3 inflammasome. Both exposure to PM2.5 and activation of NLRP3 inflammasome are related to COVID-19. Therefore, the review explores the mediation role of ATP alteration in the association of PM2.5 exposure, the NLRP3 inflammasome activation, and their related COVID-19
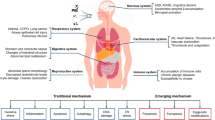
The potential ATP mediated pathway of PM2.5 exposure on NLRP3 inflammasome activation. Exposure to PM2.5 induce intracellular ATP decrease, which is linked with K+ efflux, Ca2+ influx, lysosome rupture, mitochondria disfunction, endoplasmic reticulum stress, and subsequently activate NLRP3 inflammasome
PM2.5 exposure and ATP alteration
Previous studies have shown that PM2.5 can lead to intracellular mitochondrial dysfunction and subsequently weaken mitochondrial respiration and reduce ATP production (Ku et al. 2016; Miao et al. 2019; Park et al. 2021). For example, exposure to haze, the dose of PM2.5 can reduce ATP production in the lungs of rats, decrease the activity of malate dehydrogenase and citrate synthase [critical enzymes in the tricarboxylic acid (TCA) cycle], and attenuate the expression of mitochondrial respiration chain genes such as UQCRI1 and NDUFS2(Jin et al. 2019a). ATP levels decrease significantly with increasing seasonal exposure to PM2.5, which is regulated by PPARa in a dose-dependent manner and is accompanied by cardiac damage in Sprague Dawley rats (Jin et al. 2019b). PM2.5 exposure can cause mitochondrial damage, such as mitochondrial vacuolation and rupture of the mitochondrial membrane in type II alveolar epithelial cells, and accompany a decrease in ATP levels as evidence of energy metabolism disorders (Ning et al. 2019). Li et al. reported that exposure to PM2.5 led to a decrease in Na+/K+-ATPase and Ca2+-ATPase, which can inhibit the catalysis and decomposition process of ATP and subsequently suppress the influx of K+ and the efflux of Ca2+, respectively (Li et al. 2015a). Fu et al. reported that exposure to PM2.5 can up-regulate ATP citrate lyase (ACLY), which will inevitably decrease the level of ATP (Li et al. 2015a). A recent study demonstrated that PM2.5 exposure inhibited sATP synthesis in BEAS-2B cells and down-regulated four enzymes responsible for ATP production, including ATP5F, COX7A, NDUF, and UQCR(Duan et al. 2020). Taken together, exposure to PM2.5 will cause a decrease in cellular ATP.
ATP alteration and NLRP3 inflammasome activation
It is well-known that ATP stores energy in the form of high-energy phosphate bonds and the hydrolysis of the bonds provides a large amount of free energy to drive the metabolic reaction of various cells. ATP can be synthesized during cellular respiration, either in the cytoplasm during glycolysis or in the mitochondria via the TCA cycle and the electron transport system in the presence of oxygen. The biological effect of ATP on the NLRP3 inflammasome depends on its intracellular and extracellular flow (Fig. 3). Specifically, ATP release from intracellular to extracellular can activate the NLRP3 inflammasome (Asgari et al. 2013). In other words, elevated extracellular ATP (ATP exposure) or decreased intracellular ATP (ATP efflux) may be the key step to ultimately activate the NLRP3 inflammasome (Nomura et al. 2015; Wang et al. 2013).
The process of ATP alteration activating the NLRP3 inflammasome. Both elevated extracellular ATP (ATP exposure) or decreased intracellular ATP (ATP efflux) can activate P2X7 receptor and open hemichannels such as pannexin-1 and connexin-43 in the cellular membrane, which result in various biological processes including mitochondria damage, lysosome rupture, and endoplasmic reticulum stress, and subsequently oxidative stress and inflammatory response, and finally activate the NLRP3 inflammasome
It should be noted that extracellular ATP can trigger the P2X7 membrane receptor to activate the NLRP3 inflammasome and subsequently secrete mature caspase-1 and IL-1β (Amores-Iniesta et al. 2017; Baron et al. 2015; Chen et al. 2013; Di Virgilio et al. 2017; Hudson et al. 2019; Jiang et al. 2017; Liu et al. 2018a; Pelegrin and Surprenant 2006). Blocking ATP hydrolysis by MCC950 can inhibit the activation and formation of the NLRP3 inflammasome (Coll et al. 2019). The P2X7 receptor, pannexin-1, and connexin-43 hemichannels function as ATP-gated ion channels to permeate and transfer Na+, K+, and Ca2+, and further influence NLRP3 inflammasome activation (Cymer et al. 2020; Huang et al. 2019; Karmakar et al. 2016; Mugisho et al. 2018; Mugisho et al. 2019; Parzych et al. 2017; Tonkin et al. 2018; Wang et al. 2020b; Yang et al. 2019). Activated P2X7 receptors triggered by extracellular ATP can recruit the pannexin-1 gap junction protein to form a larger pore channel, subsequently accelerating K+ efflux and Ca2+ influx, and further activating the NLRP3 inflammasome (Chakfe et al. 2002; Dubyak 2007; He et al. 2016; Hudson et al. 2019; Liu et al. 2018a; Mariathasan et al. 2006; Riteau et al. 2012; Surprenant et al. 1996). Down-regulation of the Na+/K+-ATPase and Ca2+-ATPase pump by stimuli such as PM2.5 and leptospiral glycolipoprotein activates the NLRP3 inflammasome (Geng et al. 2006; Guo et al. 2017; Lacroix-Lamande et al. 2012; Li et al. 2015a). Several studies confirm that both K+ efflux (low intracellular K+) and Ca2+ influx (high intracellular Ca2+) can trigger the NLRP3 inflammasome activated by various stimuli such as particulate matter and bacterial toxins (Liu et al. 2020; Munoz-Planillo et al. 2013; Petrilli et al. 2007; Suadicani et al. 2006).
There are a variety of additional ways, such as ROS over generation, mitochondrial deoxyribonucleic acid (DNA) damage, lysosome rupture, and endoplasmic reticulum stress, mediating the process of activation of NLRP3 inflammasomes with ATP. For example, Zhang et al. demonstrated that ATP activates the NLRP3 inflammasome in a ROS-dependent manner (Zhang et al. 2015). Macrophage treatment with ATP leads to the rapid generation of ROS, while the application of the diphenyleneiodonium nicotinamide adenine dinucleotide phosphate (NADPH) oxidase inhibitor can effectively inhibit the activation of the caspase 1-related NLRP3 inflammasome mediated by ATP (Martinon 2010). Extracellular macrophages treated with ATP induce ROS production and subsequently process and secrete pro-inflammatory cytokines, including IL-1β and interleukin-18(IL-18)(Cruz et al. 2007). Additionally, ATP treatments stimulate the generation of mitochondrial ROS (mROS), cause caspase-1 cleavage, and trigger activation of the NLRP3 inflammasome to release IL-1β and IL-18 in astrocytes (Alfonso-Loeches et al. 2014). Excessive levels of ATP acting on the cell membrane increase ROS as NADPH oxidase-dependent O2•− production in cells and trigger activation of the NLRP3 inflammasome (Abais et al. 2015). Inhibition of LPS-ATP-induced ROS production and endothelial cell pyroptosis by neferine can block the ROS/NLRP3/Caspase-1 signaling pathway (Tang et al. 2019a).
ATP plays a pivotal role in maintaining the cellular powerhouse position of mitochondria (Yu and Bennett 2016). The imbalance of intracellular and extracellular ATP will seriously impact the normal physical function of cells and the body. In other words, mitochondrial homeostasis is indispensable for normal metabolic circuits and signaling pathways based on mitochondrial metabolism. Extracellular ATP-induced mitochondrial dysfunction and disruption, such as loss of mitochondrial membrane potential and mitochondrial fragmentation, which can result in mitochondrial DNA damage and trigger activation of the extracellular ATP-induced NLRP3 inflammasome (Shimada et al. 2012; Sutterwala et al. 2014; Zhong et al. 2018).
In addition, ATP-driven destabilization or rupture of the lysosome leads to the release of the lysosome content to the cytoplasm through cathepsin B, which participates in the activation process of the NLRP3 inflammasome. For example, the activation of the NLRP3 inflammasome in the pathology of pneumococcal meningitis depends on the production of ATP, the destabilization of lysosome, and the activation of cathepsin B (Hoegen et al. 2011). Nigericin, an activator of the NLRP3 inflammasome, results in decreased cellular ATP and subsequently causes membrane permeabilization of the lysosome and activation of the NLRP3 inflammasome (Heid et al. 2013). Uptake of particulates such as silica crystals and aluminum salt leads to acidification, swelling, and rupture of the lysosome, and subsequent activation of the NLRP3 inflammasome (Hornung et al. 2008). While inhibition of phagosomal acidification or cathepsin B alters NLRP3 activation, indicating that lysosome destabilization plays a role in regulating NLRP3 inflammasome activation.
PM2.5 exposure and NLRP3 inflammasome activation
The potential molecular mechanisms of PM2.5 exposure on human health include the inflammatory response, oxidative stress, and genotoxicity (Byun et al. 2016; Chen et al. 2020; Guan et al. 2016). Additionally, oxidative stress is closely related to the inflammatory response and plays an important role in inflammatory processes (Lugrin et al. 2014). Several studies found that exposure to PM2.5 can initiate the process of NLRP3 inflammasome activation and associated inflammation-related diseases (Hu et al. 2021; Xiong et al. 2021). PM2.5 exposure may lead to increased endogenous carbon dioxide (CO2), suicidal death of erythrocytes (accompanied by loss of circulating red blood cells, hypoxia, anemia, and dysfunction of the vascular endothelium), and activated NF-kB through ligands for toll-like receptors and, subsequently, the NLRP3 inflammasome (Liu et al. 2018b; Nguyen et al. 2009; Zappulla 2008). A recent study indicated that PM2.5 promotes the NLRP3/caspase-1 pathway to further induce pulmonary inflammation (Jia et al. 2021). Furthermore, PM2.5 induces intracellular ROS and subsequently triggers lung injury such as lung inflammation and fibrosis, inhibition of blood vessel formation, and cornea inflammation by activating the NLRP3 inflammasome (Niu et al. 2021; Shen et al. 2019; Wang et al. 2020a; Zheng et al. 2018). In addition, exposure to PM2.5 leads to cardiac dysfunction and injury, which are mediated by macrophage polarization and activation of the NLRP3 inflammasome in mice with apolipoprotein E-/- (Du et al. 2019). Exposure to PM2.5 induces abnormal electrocardiogram alteration (ECG) and increased inflammatory cell and fibrosis, which may be due to activation of the NLRP3 inflammasome (Duan et al. 2019). PM2.5 from the pig house activates the TLR4/MyD88 pathway to induce ROS production and further trigger the NLRP3 inflammasome in alveolar macrophages (Tang et al. 2019b). After exposure to PM2.5 from Nrf2−/− and WT mice for 9 weeks, there were obvious depressive-like responses and the NLRP3 signaling pathway was more activated in Nrf2−/− mice than in WT mice (Chu et al. 2019). There were many activators, such as PM2.5, ATP, bacteria, and viruses, that trigger the activation of the NLRP3 inflammasome (Kelley et al. 2019; Liu et al. 2020; Liu et al. 2018b). However, the underlying mechanism of PM2.5 exposure to activation of the NLRP3 inflammasome is still unclear.
Mediation of ATP in PM2.5 exposure and NLRP3 inflammasome activation
Cellular stimulation driven by environmental or endogenous particles such as PM2.5, silica, and uric acid can trigger extracellular delivery of intracellular ATP (intracellular ATP decrease) and subsequent activation of the ligand (ATP)-gated/sensitive ionotropic P2X7 membrane receptor at the cell surface (Baron et al. 2015; Gombault et al. 2012; Riteau et al. 2012). Previous studies demonstrated that exposure to PM2.5 can inhibit Na+/K+-ATPase and Ca2+-ATPase activities and induce alveolar macrophages to produce ROS, which may indicate that ATP mediates the process of generation of ROS induced by PM2.5 and then activates the NLRP3 inflammasome (Li et al. 2015b). Additionally, extracellular ATP triggers the activation of the NLRP3 inflammasome and subsequently the maturation of IL-1β, which is consistent with the decrease in intracellular ATP driven by exposure to PM2.5 and complications of activation of the NLRP3 inflammasome (Amores-Iniesta et al. 2017; Jiang et al. 2017; Ning et al. 2019; Niu et al. 2021; Jia et al. 2021). Although some of the participants, such as the PM2.5, ATP, and NLRP3 inflammasomes, presented in different previous different studies, did not highlight the mediated and pivotal role of ATP in the association between PM2.5 exposure and activation of the NLRP3 inflammasome. Taken together, although ATP is related to several activators and regulators of the NLRP3 inflammasome, its direct key role in the process of exposure to PM2.5 activating the NLRP3 inflammasome needs further confirmation.
Association among PM2.5, NLRP3 inflammasome, and COVID-19
The great interest in the link between PM2.5, the NLRP3 inflammasome and COVID-19 arises with the COVID-19 pandemic in the world. A recent study demonstrated that PM2.5 and the air quality index were positively related to daily new cases of COVID-19 in Milan, Italy (Zoran et al. 2020). Each 1μg/m3 increase in PM2.5 is related to a 15% increase in COVID-19 death in the USA (Wu et al. 2020). A 10 μg/m3 elevation in PM2.5 was associated with a 2.24% (95% CI: 1.02 to 3.46) increase in daily confirmed cases in China (Zhu et al. 2020). In addition, both short- and long-term exposure to PM2.5 causes an increase in the incidence of lethal COVID-19(Mehmood et al. 2020). What is more, the NLRP3 inflammasome plays an important role in the pathogenesis of COVID-19 infection (Freeman and Swartz 2020; Shah 2020; van den Berg and Te 2020). An increase in diabetes complications in patients with COVID-19 is partly attributed to overactivation of the NLRP3 inflammasome (Bertocchi et al. 2020). NLRP3 inflammasome blocker drugs, such as MCC950 and Colchicine, may provide a promising treatment strategy for patients with COVID-19 infection (Paniri and Akhavan-Niaki2020). These studies may indicate that ATP-regulating drugs may be a potential treatment for patients with COVID-19.
Conclusion and future perspectives
In summary, exposure to PM2.5 can lead to decreased intracellular ATP (ATP efflux). Both elevated extracellular ATP and decreased intracellular ATP derived from particles such as PM2.5 and crystals can activate the NLRP3 inflammasome through several approaches such as K+ efflux, Ca2+ influx, ROS, mitochondrial DNA damage, lysosome destabilization and rupture. Meanwhile, exposure to PM2.5 can trigger the activation process of the NLRP3 inflammasome. However, the critical and central role of ATP in the procedure of environmental stimuli such as exposure to PM2.5 and activation of the NLRP3 inflammasome was ignored in previous studies. Understanding the roles and regulatory mechanisms of ATP alteration initiated by exposure to particulate substances in the effect of activation of the NLRP3 inflammasome is essential to develop potential treatment approaches against NLRP3-related inflammatory symptoms and diseases such as COVID-19.
This study serves as a catalyst for the role of ATP in future studies, which remain inadequate molecular mechanisms of PM2.5-driven ATP transfer and regulation and subsequent activation of the NLRP3 inflammasome. ATP-associated ion channels in the cellular membrane, such as P2X7 receptors, pannexin-1, and connexin-43, play an important role in various biological processes such as the inflammatory response, oxidative stress, and genotoxicity. Exploring the underlying molecular mechanisms of ATP transfer and regulation at the cellular level is crucial to maintaining body homeostasis and biological function. Identifying specific drugs or candidate genes for ATP-related disorders may provide novel strategies to prevent and treat a host of inflammatory diseases driven by ATP alterations.
Data availability
Please contact author for data requests.
Change history
08 February 2022
A Correction to this paper has been published: https://doi.org/10.1007/s11356-022-19090-5
Abbreviations
- PM2.5 :
-
fine particulate matter
- NLRP3:
-
NOD-like receptor family pyrin domain containing 3
- ATP:
-
adenosine triphosphate
- COVID-19:
-
coronavirus disease 2019
- PAHs:
-
polycyclic aromatic hydrocarbons
- ASC:
-
apoptosis-associated speck-like protein
- K+ :
-
potassium
- Ca2+ :
-
calcium
- Na+ :
-
sodium
- IL-1β:
-
interleukin-1β
- IL-18:
-
interleukin-18
- TCA:
-
tricarboxylic acid
- ROS:
-
reactive oxygen species
- NADPH:
-
nicotinamide adenine dinucleotide phosphate
- DNA:
-
deoxyribonucleic acid
References
Abais JM, Xia M, Zhang Y, Boini KM, Li PL (2015) Redox regulation of NLRP3 inflammasomes: ROS as trigger or effector? Antioxid Redox Signal 22(13):1111–1129. https://doi.org/10.1089/ars.2014.5994
Alfonso-Loeches S, Urena-Peralta JR, Morillo-Bargues MJ, Oliver-De LCJ, Guerri C (2014) Role of mitochondria ROS generation in ethanol-induced NLRP3 inflammasome activation and cell death in astroglial cells. Front Cell Neurosci 8:216. https://doi.org/10.3389/fncel.2014.00216
Amores-Iniesta J, Barbera-Cremades M, Martinez CM, Pons JA, Revilla-Nuin B, Martinez-Alarcon L et al (2017) Extracellular ATP Activates the NLRP3 Inflammasome and Is an Early Danger Signal of Skin Allograft Rejection. Cell Rep 21(12):3414–3426. https://doi.org/10.1016/j.celrep.2017.11.079
Asgari E, Le Friec G, Yamamoto H, Perucha E, Sacks SS, Kohl J et al (2013) C3a modulates IL-1beta secretion in human monocytes by regulating ATP efflux and subsequent NLRP3 inflammasome activation. Blood 122(20):3473–3481. https://doi.org/10.1182/blood-2013-05-502229
Baron L, Gombault A, Fanny M, Villeret B, Savigny F, Guillou N, Panek C, le Bert M, Lagente V, Rassendren F, Riteau N, Couillin I (2015) The NLRP3 inflammasome is activated by nanoparticles through ATP, ADP and adenosine. Cell Death Dis 6:e1629. https://doi.org/10.1038/cddis.2014.576
Bertocchi I, Foglietta F, Collotta D, Eva C, Brancaleone V, Thiemermann C, Collino M (2020) The hidden role of NLRP3 inflammasome in obesity-related COVID-19 exacerbations: Lessons for drug repurposing. Br J Pharmacol 177(21):4921–4930. https://doi.org/10.1111/bph.15229
Byun HM, Colicino E, Trevisi L, Fan T, Christiani DC, Baccarelli AA (2016) Effects of Air Pollution and Blood Mitochondrial DNA Methylation on Markers of Heart Rate Variability. J Am Heart Assoc 5(4):e003218. https://doi.org/10.1161/JAHA.116.003218
Chakfe Y, Seguin R, Antel JP, Morissette C, Malo D, Henderson D, Séguéla P (2002) ADP and AMP induce interleukin-1beta release from microglial cells through activation of ATP-primed P2X7 receptor channels. J Neurosci 22(8):3061–3069. https://doi.org/10.1523/JNEUROSCI.22-08-03061.2002
Chen K, Zhang J, Zhang W, Zhang J, Yang J, Li K, He Y (2013)ATP-P2X4 signaling mediates NLRP3 inflammasome activation: a novel pathway of diabetic nephropathy. Int J Biochem Cell Biol 45(5):932–943. https://doi.org/10.1016/j.biocel.2013.02.009
Chen S, Li D, Wu X, Chen L, Zhang B, Tan Y, Yu D, Niu Y, Duan H, Li Q, Chen R, Aschner M, Zheng Y, Chen W (2020) Application of cell-based biological bioassays for health risk assessment of PM2.5 exposure in three megacities, China. Environ Int 139:105703. https://doi.org/10.1016/j.envint.2020.105703
Cheng Z, Huo X, Dai Y, Lu X, Hylkema MN, Xu X (2020) Elevated expression of AhR and NLRP3 link polycyclic aromatic hydrocarbon exposure to cytokine storm in preschool children. Environ Int 139:105720. https://doi.org/10.1016/j.envint.2020.105720
Chu C, Zhang H, Cui S, Han B, Zhou L, Zhang N, Su X, Niu Y, Chen W, Chen R, Zhang R, Zheng Y (2019) Ambient PM2.5 caused depressive-like responses through Nrf2/NLRP3 signaling pathway modulating inflammation. J Hazard Mater 369:180–190. https://doi.org/10.1016/j.jhazmat.2019.02.026
Coll RC, Hill JR, Day CJ, Zamoshnikova A, Boucher D, Massey NL, Chitty JL, Fraser JA, Jennings MP, Robertson AAB, Schroder K (2019) MCC950 directly targets the NLRP3 ATP-hydrolysis motif for inflammasome inhibition. Nat Chem Biol 15(6):556–559. https://doi.org/10.1038/s41589-019-0277-7
Cruz CM, Rinna A, Forman HJ, Ventura AL, Persechini PM, Ojcius DM (2007) ATP activates a reactive oxygen species-dependent oxidative stress response and secretion of proinflammatory cytokines in macrophages. J Biol Chem 282(5):2871–2879. https://doi.org/10.1074/jbc.M608083200
Cymer M, Brzezniakiewicz-Janus K, Bujko K, Thapa A, Ratajczak J, Anusz K, Tracz M, Jackowska-Tracz A, Ratajczak MZ, Adamiak M (2020)Pannexin-1 channel "fuels" by releasing ATP from bone marrow cells a state of sterile inflammation required for optimal mobilization and homing of hematopoietic stem cells. Purinergic Signal 16(3):313–325. https://doi.org/10.1007/s11302-020-09706-1
Dai MY, Chen FF, Wang Y, Wang MZ, Lv YX, Liu RY (2020) Particulate matters induce acute exacerbation of allergic airway inflammation via the TLR2/NF-κB/NLRP3 signaling pathway. Toxicol Lett 321:146–154. https://doi.org/10.1016/j.toxlet.2019.12.013
Di Virgilio F, Dal Ben D, Sarti AC, Giuliani AL, Falzoni S (2017) The P2X7 Receptor in Infection and Inflammation. Immunity 47(1):15–31. https://doi.org/10.1016/j.immuni.2017.06.020
Du X, Jiang S, Zeng X, Zhang J, Pan K, Song L et al (2019) Fine particulate matter-induced cardiovascular injury is associated with NLRP3 inflammasome activation in Apo E(-/-) mice. Ecotoxicol Environ Saf 174:92–99. https://doi.org/10.1016/j.ecoenv.2019.02.064
Duan S, Wang N, Huang L, Zhao Y, Shao H, Jin Y, Zhang R, Li C, Wu W, Wang J, Feng F (2019) NLRP3 inflammasome activation is associated with PM2.5 -induced cardiac functional and pathological injury in mice. Environ Toxicol 34(11):1246–1254. https://doi.org/10.1002/tox.22825
Duan S, Zhang M, Sun Y, Fang Z, Wang H, Li S, Peng Y, Li J, Li J, Tian J, Yin H, Yao S, Zhang L (2020) Mechanism of PM2.5-induced human bronchial epithelial cell toxicity in central China. J Hazard Mater 396:122747. https://doi.org/10.1016/j.jhazmat.2020.122747
Dubyak GR (2007) Go it alone no more--P2X7 joins the society of heteromeric ATP-gated receptor channels. Mol Pharmacol 72(6):1402–1405. https://doi.org/10.1124/mol.107.042077
Freeman TL, Swartz TH (2020) Targeting the NLRP3 Inflammasome in Severe COVID-19. Front Immunol 11:1518. https://doi.org/10.3389/fimmu.2020.01518
Fu Y, Lu R, Cui J, Sun H, Yang H, Meng Q, Wu S, Aschner M, Li X, Chen R (2019) Inhibition of ATP citrate lyase (ACLY) protects airway epithelia from PM2.5-induced epithelial-mesenchymal transition. Ecotoxicol Environ Saf 167:309–316. https://doi.org/10.1016/j.ecoenv.2018.10.033
GBD C (2020) Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396(10258):1223–1249. https://doi.org/10.1016/S0140-6736(20)30752-2
Geng H, Meng Z, Zhang Q (2006) In vitro responses of rat alveolar macrophages to particle suspensions and water-soluble components of dust storm PM(2.5). Toxicol in Vitro 20(5):575–584. https://doi.org/10.1016/j.tiv.2005.09.015
Gombault A, Baron L, Couillin I (2012) ATP release and purinergic signaling in NLRP3 inflammasome activation. Front Immunol 3:414. https://doi.org/10.3389/fimmu.2012.00414
Guan L, Rui W, Bai R, Zhang W, Zhang F, Ding W (2016) Effects of Size-Fractionated Particulate Matter on Cellular Oxidant Radical Generation in Human Bronchial Epithelial BEAS-2B Cells. Int J Environ Res Public Health 13(5):483. https://doi.org/10.3390/ijerph13050483
Guo Z, Hong Z, Dong W, Deng C, Zhao R, Xu J, Zhuang G, Zhang R (2017) PM2.5-Induced Oxidative Stress and Mitochondrial Damage in the Nasal Mucosa of Rats. Int J Environ Res Public Health 14(2):134. https://doi.org/10.3390/ijerph14020134
He Y, Hara H, Nunez G (2016) Mechanism and Regulation of NLRP3 Inflammasome Activation. Trends Biochem Sci 41(12):1012–1021. https://doi.org/10.1016/j.tibs.2016.09.002
Heid ME, Keyel PA, Kamga C, Shiva S, Watkins SC, Salter RD (2013) Mitochondrial reactive oxygen species induces NLRP3-dependent lysosomal damage and inflammasome activation. J Immunol 191(10):5230–5238. https://doi.org/10.4049/jimmunol.1301490
Hoegen T, Tremel N, Klein M, Angele B, Wagner H, Kirschning C, Pfister HW, Fontana A, Hammerschmidt S, Koedel U (2011) The NLRP3 inflammasome contributes to brain injury in pneumococcal meningitis and is activated through ATP-dependent lysosomal cathepsin B release. J Immunol 187(10):5440–5451. https://doi.org/10.4049/jimmunol.1100790
Hornung V, Bauernfeind F, Halle A, Samstad EO, Kono H, Rock KL, Fitzgerald KA, Latz E (2008) Silica crystals and aluminum salts activate the NALP3 inflammasome through phagosomal destabilization. Nat Immunol 9(8):847–856. https://doi.org/10.1038/ni.1631
Hu T, Zhu P, Liu Y, Zhu H, Geng J, Wang B, Yuan G, Peng Y, Xu B (2021) PM2.5 induces endothelial dysfunction via activating NLRP3 inflammasome. Environ Toxicol 36:1886–1893. https://doi.org/10.1002/tox.23309
Huang Y, Mao Z, Zhang Z, Obata F, Yang X, Zhang X, Huang Y, Mitsui T, Fan J, Takeda M, Yao J (2019) Connexin43 Contributes to Inflammasome Activation and Lipopolysaccharide-Initiated Acute Renal Injury via Modulation of Intracellular Oxidative Status. Antioxid Redox Signal 31(16):1194–1212. https://doi.org/10.1089/ars.2018.7636
Hudson G, Flannigan KL, Venu V, Alston L, Sandall CF, MacDonald JA et al (2019) Pregnane X Receptor Activation Triggers Rapid ATP Release in Primed Macrophages That Mediates NLRP3 Inflammasome Activation. J Pharmacol Exp Ther 370(1):44–53. https://doi.org/10.1124/jpet.118.255679
Jia H, Liu Y, Guo D, He W, Zhao L, Xia S (2021) PM2.5-induced pulmonary inflammation via activating of the NLRP3/caspase-1 signaling pathway. Environ Toxicol 36(3):298–307. https://doi.org/10.1002/tox.23035
Jiang S, Zhang Y, Zheng JH, Li X, Yao YL, Wu YL, Song SZ, Sun P, Nan JX, Lian LH (2017) Potentiation of hepatic stellate cell activation by extracellular ATP is dependent on P2X7R-mediated NLRP3 inflammasome activation. Pharmacol Res 117:82–93. https://doi.org/10.1016/j.phrs.2016.11.040
Jin X, Su H, Ding G, Sun Z, Li Z (2019a) Exposure to ambient fine particles causes abnormal energy metabolism and ATP decrease in lung tissues. Chemosphere 224:29–38. https://doi.org/10.1016/j.chemosphere.2019.02.116
Jin X, Xue B, Ahmed RZ, Ding G, Li Z (2019b) Fine particles cause the abnormality of cardiac ATP levels via PPARa-mediated utilization of fatty acid and glucose using in vivo and in vitro models. Environ Pollut 249:286–294. https://doi.org/10.1016/j.envpol.2019.02.083
Juliana C, Fernandes-Alnemri T, Kang S, Farias A, Qin F, Alnemri ES (2012) Non-transcriptional priming and deubiquitination regulate NLRP3 inflammasome activation. J Biol Chem. 287(43):36617–36622. PMID: 22948162. https://doi.org/10.1074/jbc.M112.407130
Karmakar M, Katsnelson MA, Dubyak GR, Pearlman E (2016) Neutrophil P2X7 receptors mediate NLRP3 inflammasome-dependent IL-1β secretion in response to ATP. Nat Commun 7:10555. https://doi.org/10.1038/ncomms10555
Kelley N, Jeltema D, Duan Y, He Y (2019) The NLRP3 Inflammasome: An Overview of Mechanisms of Activation and Regulation. Int J Mol Sci 20(13):E3328. https://doi.org/10.3390/ijms20133328
Ku T, Ji X, Zhang Y, Li G, Sang N (2016) PM2.5, SO2 and NO2co-exposure impairs neurobehavior and induces mitochondrial injuries in the mouse brain. Chemosphere 163:27–34. https://doi.org/10.1016/j.chemosphere.2016.08.009
Kurashima Y, Amiya T, Nochi T, Fujisawa K, Haraguchi T, Iba H, Tsutsui H, Sato S, Nakajima S, Iijima H, Kubo M, Kunisawa J, Kiyono H (2012) Extracellular ATP mediates mast cell-dependent intestinal inflammation through P2X7 purinoceptors. Nat Commun 3:1034. PMID: 22948816. https://doi.org/10.1038/ncomms2023
Lacroix-Lamande S, D'Andon MF, Michel E, Ratet G, Philpott DJ, Girardin SE et al (2012) Downregulation of the Na/K-ATPase pump by leptospiral glycolipoprotein activates the NLRP3 inflammasome. J Immunol 188(6):2805–2814. https://doi.org/10.4049/jimmunol.1101987
Li R, Kou X, Geng H, Xie J, Tian J, Cai Z, Dong C (2015a) Mitochondrial damage: an important mechanism of ambient PM2.5 exposure-induced acute heart injury in rats. J Hazard Mater 287:392–401. https://doi.org/10.1016/j.jhazmat.2015.02.006
Li R, Kou X, Geng H, Xie J, Yang Z, Zhang Y, Cai Z, Dong C (2015b) Effect of ambient PM(2.5) on lung mitochondrial damage and fusion/fission gene expression in rats. Chem Res Toxicol 28(3):408–418. https://doi.org/10.1021/tx5003723
Liu D, Zeng X, Li X, Mehta JL, Wang X (2018a) Role of NLRP3 inflammasome in the pathogenesis of cardiovascular diseases. Basic Res Cardiol 113(1):5. https://doi.org/10.1007/s00395-017-0663-9
Liu Q, Zhang D, Hu D, Zhou X, Zhou Y (2018b) The role of mitochondria in NLRP3 inflammasome activation. Mol Immunol 103:115–124. https://doi.org/10.1016/j.molimm.2018.09.010
Liu D, Zeng X, Li X, Cui C, Hou R, Guo Z, Mehta JL, Wang X (2020) Advances in the molecular mechanisms of NLRP3 inflammasome activators and inacativators. Biochem Pharmacol 175:113863. https://doi.org/10.1016/j.bcp.2020.113863
Lugrin J, Rosenblatt-Velin N, Parapanov R, Liaudet L (2014) The role of oxidative stress during inflammatory processes. Biol Chem 395(2):203–230. https://doi.org/10.1515/hsz-2013-0241
Mariathasan S, Weiss DS, Newton K, McBride J, O'Rourke K, Roose-Girma M, Lee WP, Weinrauch Y, Monack DM, Dixit VM (2006) Cryopyrin activates the inflammasome in response to toxins and ATP. Nature 440(7081):228–232. https://doi.org/10.1038/nature04515
Martinon F (2010) Signaling by ROS drives inflammasome activation. Eur J Immunol 40(3):616–619. https://doi.org/10.1002/eji.200940168
Mehmood K, Saifullah, Iqbal M, Abrar MM (2020) Can exposure to PM2.5 particles increase the incidence of coronavirus disease 2019 (COVID-19)? Sci Total Environ 741:140441. https://doi.org/10.1016/j.scitotenv.2020.140441
Miao X, Li W, Niu B, Li J, Sun J, Qin M, Zhou Z (2019) Mitochondrial dysfunction in endothelial cells induced by airborne fine particulate matter (<2.5 μm). J Appl Toxicol 39(10):1424–1432. https://doi.org/10.1002/jat.3828
Mugisho OO, Green CR, Kho DT, Zhang J, Graham ES, Acosta ML, Rupenthal ID (2018) The inflammasome pathway is amplified and perpetuated in an autocrine manner through connexin43 hemichannel mediated ATP release. Biochim Biophys Acta Gen Subj 1862(3):385–393. https://doi.org/10.1016/j.bbagen.2017.11.015
Mugisho OO, Rupenthal ID, Paquet-Durand F, Acosta ML, Green CR (2019) Targeting connexin hemichannels to control the inflammasome: the correlation between connexin43 and NLRP3 expression in chronic eye disease. Expert Opin Ther Targets 23(10):855–863. https://doi.org/10.1080/14728222.2019.1673368
Munoz-Planillo R, Kuffa P, Martinez-Colon G, Smith BL, Rajendiran TM, Nunez G (2013) K(+) efflux is the common trigger of NLRP3 inflammasome activation by bacterial toxins and particulate matter. Immunity 38(6):1142–1153. https://doi.org/10.1016/j.immuni.2013.05.016
Nguyen TT, Föller M, Lang F (2009) Tin triggers suicidal death of erythrocytes. J Appl Toxicol 29(1):79–83. https://doi.org/10.1002/jat.1390
Ning X, Ji X, Li G, Sang N (2019) Ambient PM2.5 causes lung injuries and coupled energy metabolic disorder. Ecotoxicol Environ Saf 170:620–626. https://doi.org/10.1016/j.ecoenv.2018.12.028
Niu L, Li L, Xing C, Luo B, Hu C, Song M, Niu J, Ruan Y, Sun X, Lei Y (2021) Airborne particulate matter (PM2.5) triggers cornea inflammation and pyroptosis via NLRP3 activation. Ecotoxicol Environ Saf 207:111306. https://doi.org/10.1016/j.ecoenv.2020.111306
Nomura J, So A, Tamura M, Busso N (2015) Intracellular ATP Decrease Mediates NLRP3 Inflammasome Activation upon Nigericin and Crystal Stimulation. J Immunol 195(12):5718–5724. https://doi.org/10.4049/jimmunol.1402512
Paniri A, Akhavan-Niaki H (2020) Emerging role of IL-6 and NLRP3 inflammasome as potential therapeutic targets to combat COVID-19: Role of lncRNAs in cytokine storm modulation. Life Sci 257:118114. https://doi.org/10.1016/j.lfs.2020.118114
Park SK, Kang JY, Kim JM, Kim HJ, Heo HJ (2021) Ecklonia cava Attenuates PM2.5-Induced Cognitive Decline through Mitochondrial Activation and Anti-Inflammatory Effect. Mar Drugs 19(3):131. https://doi.org/10.3390/md19030131
Parzych K, Zetterqvist AV, Wright WR, Kirkby NS, Mitchell JA, Paul-Clark MJ (2017) Differential role of pannexin-1/ATP/P2X7 axis in IL-1β release by human monocytes. FASEB J 31(6):2439–2445. https://doi.org/10.1096/fj.201600256
Pelegrin P, Surprenant A (2006)Pannexin-1 mediates large pore formation and interleukin-1beta release by the ATP-gated P2X7 receptor. EMBO J 25(21):5071–5082. https://doi.org/10.1038/sj.emboj.7601378
Petrilli V, Papin S, Dostert C, Mayor A, Martinon F, Tschopp J (2007) Activation of the NALP3 inflammasome is triggered by low intracellular potassium concentration. Cell Death Differ 14(9):1583–1589. https://doi.org/10.1038/sj.cdd.4402195
Qu J, Tao XY, Teng P, Zhang Y, Guo CL, Hu L, Qian YN, Jiang CY, Liu WT (2017) Blocking ATP-sensitive potassium channel alleviates morphine tolerance by inhibiting HSP70-TLR4-NLRP3-mediated neuroinflammation. J Neuroinflammation 14(1):228. PMID: 29178967. https://doi.org/10.1186/s12974-017-0997-0
Riteau N, Baron L, Villeret B, Guillou N, Savigny F, Ryffel B, Rassendren F, le Bert M, Gombault A, Couillin I (2012) ATP release and purinergic signaling: a common pathway for particle-mediated inflammasome activation. Cell Death Dis 3:e403. https://doi.org/10.1038/cddis.2012.144
Sadatomi D, Nakashioya K, Mamiya S, Honda S, Kameyama Y, Yamamura Y, Tanimura S, Takeda K (2017) Mitochondrial function is required for extracellular ATP-induced NLRP3 inflammasome activation. J Biochem 161(6):503-512. PMID: 28096454. https://doi.org/10.1093/jb/mvw098
Samek L, Furman L, Mikrut M, Regiel-Futyra A, Macyk W, Stochel G, van Eldik R (2017) Chemical composition of submicron and fine particulate matter collected in Krakow, Poland. Consequences for the APARIC project. Chemosphere 187:430–439. https://doi.org/10.1016/j.chemosphere.2017.08.090
Shah A (2020) Novel Coronavirus-Induced NLRP3 Inflammasome Activation: A Potential Drug Target in the Treatment of COVID-19. Front Immunol 11:1021. https://doi.org/10.3389/fimmu.2020.01021
Sharma J, Parsai K, Raghuwanshi P, Ali SA, Tiwari V, Bhargava A, Mishra PK (2021) Emerging role of mitochondria in airborne particulate matter-induced immunotoxicity. Environ Pollut 270:116242. https://doi.org/10.1016/j.envpol.2020.116242
Shen C, Liu J, Zhu F, Lei R, Cheng H, Zhang C, Sui X, Ding L, Yang M, Chen H, Ding R, Cao J (2019) The effects of cooking oil fumes-derived PM2.5 on blood vessel formation through ROS-mediated NLRP3 inflammasome pathway in human umbilical vein endothelial cells. Ecotoxicol Environ Saf 174:690–698. https://doi.org/10.1016/j.ecoenv.2019.03.028
Shi JQ, Wang BR, Jiang T, Gao L, Zhang YD, Xu J (2020) NLRP3 Inflammasome: A Potential Therapeutic Target in Fine Particulate Matter-Induced Neuroinflammation in Alzheimer's Disease. J Alzheimers Dis 77(3):923-934. PMID: 32804134. https://doi.org/10.3233/JAD-200359
Shim DW, Shin WY, Yu SH, Kim BH, Ye SK, Koppula S, Won HS, Kang TB, Lee KH (2017) BOT-4-one attenuates NLRP3 inflammasome activation: NLRP3 alkylation leading to the regulation of its ATPase activity and ubiquitination. Sci Rep (1):15020. PMID: 29118366, https://doi.org/10.1038/s41598-017-15314-8
Shimada K, Crother TR, Karlin J, Dagvadorj J, Chiba N, Chen S, Ramanujan VK, Wolf AJ, Vergnes L, Ojcius DM, Rentsendorj A, Vargas M, Guerrero C, Wang Y, Fitzgerald KA, Underhill DM, Town T, Arditi M (2012) Oxidized mitochondrial DNA activates the NLRP3 inflammasome during apoptosis. Immunity 36(3):401–414. https://doi.org/10.1016/j.immuni.2012.01.009
Shou Y, Huang Y, Zhu X, Liu C, Hu Y, Wang H (2019) A review of the possible associations between ambient PM2.5 exposures and the development of Alzheimer's disease. Ecotoxicol Environ Saf 174:344–352. https://doi.org/10.1016/j.ecoenv.2019.02.086
Suadicani SO, Brosnan CF, Scemes E (2006) P2X7 receptors mediate ATP release and amplification of astrocytic intercellular Ca2+ signaling. J Neurosci 26(5):1378–1385. https://doi.org/10.1523/JNEUROSCI.3902-05.2006
Sun B, Shi Y, Li Y, Jiang J, Liang S, Duan J, Sun Z (2020)Short-term PM2.5 exposure induces sustained pulmonary fibrosis development during post-exposure period in rats. J Hazard Mater 385:121566. https://doi.org/10.1016/j.jhazmat.2019.121566
Surprenant A, Rassendren F, Kawashima E, North RA, Buell G (1996) The cytolytic P2Z receptor for extracellular ATP identified as a P2X receptor (P2X7). Science 272(5262):735–738. https://doi.org/10.1126/science.272.5262.735
Sutterwala FS, Haasken S, Cassel SL (2014) Mechanism of NLRP3 inflammasome activation. Ann N Y Acad Sci 1319:82–95. https://doi.org/10.1111/nyas.12458
Tang Q, Huang K, Liu J, Wu S, Shen D, Dai P, Li C (2019a) Fine particulate matter from pig house induced immune response by activating TLR4/MAPK/NF-kappaB pathway and NLRP3 inflammasome in alveolar macrophages. Chemosphere 236:124373. https://doi.org/10.1016/j.chemosphere.2019.124373
Tang YS, Zhao YH, Zhong Y, Li XZ, Pu JX, Luo YC, Zhou QL (2019b) Neferine inhibits LPS-ATP-induced endothelial cell pyroptosis via regulation of ROS/NLRP3/Caspase-1 signaling pathway. Inflamm Res 68(9):727–738. https://doi.org/10.1007/s00011-019-01256-6
Tao RJ, Cao WJ, Li MH, Yang L, Dai RX, Luo XL, Liu Y, Ge BX, Su X, Xu JF (2020) PM2.5 compromises antiviral immunity in influenza infection by inhibiting activation of NLRP3 inflammasome and expression of interferon-beta. Mol Immunol 125:178–186. https://doi.org/10.1016/j.molimm.2020.07.001
Tonkin RS, Bowles C, Perera CJ, Keating BA, Makker PGS, Duffy SS, Lees JG, Tran C, Don AS, Fath T, Liu L, O'Carroll SJ, Nicholson LFB, Green CR, Gorrie C, Moalem-Taylor G (2018) Attenuation of mechanical pain hypersensitivity by treatment with Peptide5, a connexin-43 mimetic peptide, involves inhibition of NLRP3 inflammasome in nerve-injured mice. Exp Neurol 300:1–12. https://doi.org/10.1016/j.expneurol.2017.10.016
van den Berg DF, Te VA (2020) Severe COVID-19: NLRP3 Inflammasome Dysregulated. Front Immunol 11:1580. https://doi.org/10.3389/fimmu.2020.01580
Wang Y, Yang C, Mao K, Chen S, Meng G, Sun B (2013) Cellular localization of NLRP3 inflammasome. Protein Cell 4(6):425–431. https://doi.org/10.1007/s13238-013-2113-2
Wang BR, Shi JQ, Ge NN, Ou Z, Tian YY, Jiang T, Zhou JS, Xu J, Zhang YD (2018) PM2.5 exposure aggravates oligomeric amyloid beta-induced neuronal injury and promotes NLRP3 inflammasome activation in an in vitro model of Alzheimer's disease. J Neuroinflammation 15(1):132. PMID: 29720213. https://doi.org/10.1186/s12974-018-1178-5
Wang C, Meng X, Meng M, Shi M, Sun W, Li X, Zhang X, Liu R, Fu Y, Song L (2020a) Oxidative stress activates the TRPM2-Ca(2+)-NLRP3 axis to promote PM2.5-induced lung injury of mice. Biomed Pharmacother 130:110481. https://doi.org/10.1016/j.biopha.2020.110481
Wang W, Hu D, Feng Y, Wu C, Song Y, Liu W, Li A, Wang Y, Chen K, Tian M, Xiao F, Zhang Q, Chen W, Pan P, Wan P, Liu Y, Lan H, Wu K, Wu J (2020b) Paxillin mediates ATP-induced activation of P2X7 receptor and NLRP3 inflammasome. BMC Biol 18(1):182. https://doi.org/10.1186/s12915-020-00918-w
Wei T, Tang M (2018) Biological effects of airborne fine particulate matter (PM2.5) exposure on pulmonary immune system. Environ Toxicol Pharmacol 60:195–201. https://doi.org/10.1016/j.etap.2018.04.004
WHO (2016) Ambient air pollution: a global assessment of exposure and burden of disease. World Health OrganizationAvailable from: https://apps.who.int/iris/handle/10665/250141.
Wu X, Nethery R C, Sabath B M, Braun D, Dominici F (2020) Exposure to air pollution and COVID-19 mortality in the United States: A nationwide cross-sectional study. medRxiv. [Preprint]. Sci Adv. 6(45). https://doi.org/10.1101/2020.04.05.20054502
Xie Y, Liu Z, Wen T, Huang X, Liu J, Tang G, Yang Y, Li X, Shen R, Hu B, Wang Y (2019) Characteristics of chemical composition and seasonal variations of PM2.5 in Shijiazhuang, China: Impact of primary emissions and secondary formation. Sci Total Environ 677:215–229. https://doi.org/10.1016/j.scitotenv.2019.04.300
Xiong R, Jiang W, Li N, Liu B, He R, Wang B, Geng Q (2021) PM2.5-induced lung injury is attenuated in macrophage-specific NLRP3 deficient mice. Ecotoxicol Environ Saf 221:112433. https://doi.org/10.1016/j.ecoenv.2021.112433
Xu G, Ren X, Xiong K, Li L, Bi X, Wu Q (2020) Analysis of the driving factors of PM2.5 concentration in the air: A case study of the Yangtze River Delta, China. Ecol Indic 110:105889. https://doi.org/10.1016/j.ecolind.2019.105889
Yang X, Zhao G, Yan J, Xu R, Che C, Zheng H, Zhu G, Zhang J (2019) Pannexin 1 Channels Contribute to IL-1β Expression via NLRP3/Caspase-1 Inflammasome in Aspergillus Fumigatus Keratitis. Curr Eye Res 44(7):716–725. https://doi.org/10.1080/02713683.2019.1584321
Yu EP, Bennett MR (2016) The role of mitochondrial DNA damage in the development of atherosclerosis. Free Radic Biol Med 100:223–230. https://doi.org/10.1016/j.freeradbiomed.2016.06.011
Zappulla D (2008) Environmental stress, erythrocyte dysfunctions, inflammation, and the metabolic syndrome: adaptations to CO2 increases? J Cardiometab Syndr 3(1):30–34. https://doi.org/10.1111/j.1559-4572.2008.07263.x
Zeng X, Huo X, Xu X, Liu D, Wu W (2020)E-waste lead exposure and children's health in China. Sci Total Environ 734:139286. https://doi.org/10.1016/j.scitotenv.2020.139286
Zhang F, Xu L, Chen J, Chen X, Niu Z, Lei T, Li C, Zhao J (2013) Chemical characteristics of PM2.5 during haze episodes in the urban of Fuzhou, China. Particuology 11(3):264–272. https://doi.org/10.1016/j.partic.2012.07.001
Zhang A, Wang P, Ma X, Yin X, Li J, Wang H, Jiang W, Jia Q, Ni L (2015) Mechanisms that lead to the regulation of NLRP3 inflammasome expression and activation in human dental pulp fibroblasts. Mol Immunol 66(2):253–262. https://doi.org/10.1016/j.molimm.2015.03.009
Zhao L, Wang L, Tan J, Duan J, Ma X, Zhang C, Ji S, Qi M, Lu XH, Wang Y, Wang Q, Xu R (2019) Changes of chemical composition and source apportionment of PM2.5 during 2013–2017 in urban Handan, China. Atmos Environ 206:119–131. https://doi.org/10.1016/j.atmosenv.2019.02.034
Zheng R, Tao L, Jian H, Chang Y, Cheng Y, Feng Y, Zhang H (2018) NLRP3 inflammasome activation and lung fibrosis caused by airborne fine particulate matter. Ecotoxicol Environ Saf 163:612–619. https://doi.org/10.1016/j.ecoenv.2018.07.076
Zhong Z, Liang S, Sanchez-Lopez E, He F, Shalapour S, Lin XJ, Wong J, Ding S, Seki E, Schnabl B, Hevener AL, Greenberg HB, Kisseleva T, Karin M (2018) New mitochondrial DNA synthesis enables NLRP3 inflammasome activation. Nature 560(7717):198–203. https://doi.org/10.1038/s41586-018-0372-z
Zhu Y, Xie J, Huang F, Cao L (2020) Association between short-term exposure to air pollution and COVID-19 infection: Evidence from China. Sci Total Environ 727:138704. https://doi.org/10.1016/j.scitotenv.2020.138704
Zoran MA, Savastru RS, Savastru DM, Tautan MN (2020) Assessing the relationship between surface levels of PM2.5 and PM10 particulate matter impact on COVID-19 in Milan, Italy. Sci Total Environ 738:139825. https://doi.org/10.1016/j.scitotenv.2020.139825
Acknowledgements
Not applicable.
Funding
This work was supported by the Postdoctoral Research Foundation of China (2020M683183), the Natural Science Foundation of Henan Province of China (202300410313), and the National Natural Science Foundation of China (21876065).
Author information
Authors and Affiliations
Contributions
Xiang Zeng: Writing—original draft, Conceptualization, Supervision, Funding acquisition. Dongling Liu: Writing—review & editing, Validation, Funding acquisition. Weidong Wu: Writing—review & editing, Validation. Xia Huo: Writing—review & editing, Validation, Supervision, Funding acquisition.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
The authors declare that they are consent for the publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Responsible Editor: Mohamed M. Abdel-Daim
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: There should only be 2 affiliations for this article.
Rights and permissions
About this article
Cite this article
Zeng, X., Liu, D., Wu, W. et al. PM2.5 exposure inducing ATP alteration links with NLRP3 inflammasome activation. Environ Sci Pollut Res 29, 24445–24456 (2022). https://doi.org/10.1007/s11356-021-16405-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-16405-w