Abstract
Purpose
Noninvasive positive pressure ventilation (NPPV) may permit tracheostomy decannulation (TD) in patients with congenital central hypoventilation syndrome (CCHS) requiring nocturnal positive pressure ventilation via tracheostomy (PPV-T). There is limited evidence on optimal strategies for transitioning patients from PPV-T to NPPV. This study aimed to describe the clinical course and outcome of children with CCHS who underwent TD and transitioned from PPV-T to NPPV.
Methods
Retrospective review was conducted on patients with CCHS using nocturnal PPV-T who underwent TD to NPPV. The results of clinical evaluations, airway endoscopy, polysomnography, and clinical course leading to TD were analyzed.
Results
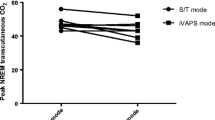
We identified 3 patients with CCHS aged 8–17 years who required PPV-T only during sleep. Patients underwent systematic multidisciplinary evaluations with a pediatric psychologist, pulmonologist, sleep physician, and otolaryngologist utilizing a TD algorithm. These included evaluation in the sleep clinic, NPPV mask fitting and desensitization, endoscopic airway evaluation, daytime tracheostomy capping, acclimatization to low-pressure NPPV, polysomnography with capped tracheostomy and NPPV titration, and if successful, TD. All patients underwent successful TD following optimal titration of NPPV during polysomnography. The duration to TD from decision to pursue NPPV was between 2.4 and 10.6 months, and the duration of hospitalization for TD was between 4 and 5 days. There were no NPPV-related complications; however, all patients required surgical closure of tracheocutaneous fistula.
Conclusion
NPPV may be an effective and feasible option for patients with CCHS requiring PPV-T during sleep and permits TD. In patients with CCHS, a systematic multidisciplinary algorithm may optimize successful transition to NPPV and TD.
Similar content being viewed by others
References
Weese-Mayer DE, Berry-Kravis EM, Ceccherini I, Keens TG, Loghmanee DA, Trang H, ATS Congenital Central Hypoventilation Syndrome Subcommittee (2010) An official ATS clinical policy statement: congenital central hypoventilation syndrome - genetic basis, diagnosis, and management. Am J Respir Crit Care Med 181:626–644. https://doi.org/10.1164/rccm.200807-1069ST
Kasi AS, Perez IA, Kun SS, Keens TG (2016) Congenital central hypoventilation syndrome: diagnostic and management challenges. Pediatric Health Med Ther 7:99–107. https://doi.org/10.2147/PHMT.S95054
Vanderlaan M, Holbrook CR, Wang M, Tuell A, Gozal D (2004) Epidemiologic survey of 196 patients with congenital central hypoventilation syndrome. Pediatr Pulmonol 37:217–229. https://doi.org/10.1002/ppul.10438
Ramesh P, Boit P, Samuels M (2008) Mask ventilation in the early management of congenital central hypoventilation syndrome. Arch Dis Child Fetal Neonatal Ed 93:F400–F403. https://doi.org/10.1136/adc.2008.139931
Kerbl R, Litscher H, Grubbauer HM, Reiterer F, Zobel G, Trop M, Urlesberger B, Eber E, Kurz R (1996) Congenital central hypoventilation syndrome (Ondine’s curse syndrome) in two siblings: delayed diagnosis and successful noninvasive treatment. Eur J Pediatr 155:977–980. https://doi.org/10.1007/bf02282890
Xu Z, Wu Y, Li B, Zheng L, Liu J, Shen K (2019) Noninvasive ventilation in a young infant with congenital central hypoventilation and 7-year follow-up. Pediatr Investig 3:261–264
Migliori C, Cavazza A, Motta M et al (2003) Early use of Nasal-BiPAP in two infants with congenital central hypoventilation syndrome. Acta Paediatr 92:823–826. https://doi.org/10.1080/08035250310002849
Saddi V, Teng A, Thambipillay G et al (2019) Nasal mask average volume-assured pressure support in an infant with congenital central hypoventilation syndrome. Respirol case reports 7:e00448
Tibballs J, Henning RD (2003) Noninvasive ventilatory strategies in the management of a newborn infant and three children with congenital central hypoventilation syndrome. Pediatr Pulmonol 36:544–548. https://doi.org/10.1002/ppul.10392
Trang H, Samuels M, Ceccherini I, Frerick M, Garcia-Teresa MA, Peters J, Schoeber J, Migdal M, Markstrom A, Ottonello G, Piumelli R, Estevao MH, Senecic-Cala I, Gnidovec-Strazisar B, Pfleger A, Porto-Abal R, Katz-Salamon M (2020) Guidelines for diagnosis and management of congenital central hypoventilation syndrome. Orphanet J Rare Dis 15:252. https://doi.org/10.1186/s13023-020-01460-2
Willis D, Scribner A, Jambhekar S (2017) Successful tracheal decannulation in a child with congenital central hypoventilation syndrome. Ann Clin Case Rep 2:1439 http://www.anncaserep.com/full-text/accr-v2-id1439.php
Vagiakis E, Koutsourelakis I, Perraki E, Roussos C, Mastora Z, Zakynthinos S, Kotanidou A (2010) Average volume-assured pressure support in a 16-year-old girl with congenital central hypoventilation syndrome. J Clin Sleep Med 6:609–612
Kam K, Bjornson C, Mitchell I (2014) Congenital central hypoventilation syndrome; safety of early transition to non-invasive ventilation. Pediatr Pulmonol 49:410–413. https://doi.org/10.1002/ppul.22848
Paglietti MG, Porcaro F, Sovtic A, Cherchi C, Verrillo E, Pavone M, Bottero S, Cutrera R (2019) Decannulation in children affected by congenital central hypoventilation syndrome: a proposal of an algorithm from two European centers. Pediatr Pulmonol 54:1663–1669. https://doi.org/10.1002/ppul.24448
Henningfeld JK, Maletta K, Ren B, Richards KL, Wegner C, D'Andrea LA (2016) Liberation from home mechanical ventilation and decannulation in children. Pediatr Pulmonol 51:838–849. https://doi.org/10.1002/ppul.23396
Perez IA, Keens TG, Davidson Ward SL (2010) Noninvasive positive pressure ventilation in the treatment of hypoventilation in children. Sleep Med Clin 5:471–484. https://doi.org/10.1016/j.jsmc.2010.05.013
Mitchell RB, Hussey HM, Setzen G, Jacobs IN, Nussenbaum B, Dawson C, Brown CA III, Brandt C, Deakins K, Hartnick C, Merati A (2013) Clinical consensus statement: tracheostomy care. Otolaryngol Head Neck Surg 148:6–20. https://doi.org/10.1177/0194599812460376
Berry RB, Chediak A, Brown LK, Finder J, Gozal D, Iber C, Kushida CA, Morgenthaler T, Rowley JA, Davidson-Ward SL, NPPV Titration Task Force of the American Academy of Sleep Medicine (2010) Best clinical practices for the sleep center adjustment of noninvasive positive pressure ventilation (NPPV) in stable chronic alveolar hypoventilation syndromes. J Clin Sleep Med 6:491–509
Kushida CA, Chediak A, Berry RB, Brown LK, Gozal D, Iber C, Parthasarathy S, Quan SF, Rowley JA, Positive Airway Pressure Titration Task Force, American Academy of Sleep Medicine (2008) Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J Clin Sleep Med 4:157–171
Valika T, Chin AC, Thompson DM, Kabre R, Lavin JM, Neault SH, Ballard HA, Kenny AS, Weese-Mayer DE (2019) Airway obstruction during sleep due to diaphragm pacing precludes decannulation in young children with CCHS. Respiration. 98:263–267
Slifer KJ, Kruglak D, Benore E, Bellipanni K, Falk L, Halbower AC, Amari A, Beck M (2007) Behavioral training for increasing preschool children’s adherence with positive airway pressure: a preliminary study. Behav Sleep Med 5:147–175. https://doi.org/10.1080/15402000701190671
Parmar A, Baker A, Narang I (2019) Positive airway pressure in pediatric obstructive sleep apnea. Paediatr Respir Rev 31:43–51. https://doi.org/10.1016/j.prrv.2019.04.006
DiFeo N, Meltzer LJ, Beck SE, Karamessinis LR, Cornaglia MA, Traylor J, Samuel J, Gallagher PR, Radcliffe J, Beris H, Menello MK, Marcus CL (2012) Predictors of positive airway pressure therapy adherence in children: a prospective study. J Clin Sleep Med 8:279–286. https://doi.org/10.5664/jcsm.1914
Harford K-L, Jambhekar S, Com G, Pruss K, Kabour M, Jones K, Ward WL (2013) Behaviorally based adherence program for pediatric patients treated with positive airway pressure. Clin Child Psychol Psychiatry 18:151–163. https://doi.org/10.1177/1359104511431662
Huang J, Colrain IM, Panitch HB, Tapia IE, Schwartz MS, Samuel J, Pepe M, Bandla P, Bradford R, Mosse YP, Maris JM, Marcus CL (2008) Effect of sleep stage on breathing in children with central hypoventilation. J Appl Physiol 105:44–53. https://doi.org/10.1152/japplphysiol.01269.2007
Acknowledgement
The authors thank the patients for their participation in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study was approved by the institutional review board at Children’s Healthcare of Atlanta.
Informed consent
This study was approved by the institutional review board at Children’s Healthcare of Atlanta. The data used was retrospective; hence, the requirements for informed consent and parental permission were waived.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(PDF 91 kb)
Rights and permissions
About this article
Cite this article
Kasi, A.S., Anand, N., Harford, KL. et al. Tracheostomy decannulation to noninvasive positive pressure ventilation in congenital central hypoventilation syndrome. Sleep Breath 26, 133–139 (2022). https://doi.org/10.1007/s11325-021-02368-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02368-2