Abstract
Purpose
We sought to determine the prevalence of low arousal threshold (LAT) in veterans with post-traumatic stress disorder (PTSD) and whether or not LAT is associated with decreased use of continuous positive airway pressure (CPAP).
Methods
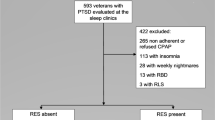
We conducted a retrospective study of all veterans with documented PTSD who had an apnea hypopnea index > 5/h over a 27-month period. Demographic, clinical characteristics, and CPAP usage were extracted from the medical records. A multivariate analysis was conducted to assess predictors of CPAP use at 3 months in patients with LAT after adjusting for severity of PTSD.
Results
LAT was identified in 55% of 119 patients with PTSD and newly diagnosed OSA. LAT was associated with younger age (odds ratio [OR] 0.91; 95% confidence interval [CI] 0.86–0.95), lower BMI (OR 0.82; 95% CI 0.73–0.91), presence of insomnia (OR 1.34; 95% CI 1.19–1.81), and use of antidepressant (OR 1.14; 95% CI 1.09–2.01). PTSD severity, REM rebound, and the presence of baseline comorbid insomnia were each associated with CPAP use at 3 months. Neither daytime sleepiness, body mass index (BMI), nor LAT endotype was correlated with CPAP utilization. Insomnia was the only factor associated with decreased CPAP use in patients with PTSD and LAT (P = 0.04).
Conclusion
The LAT endotype is common among veterans with PTSD. An improved understanding of how insomnia in this population affects CPAP utilization would be instrumental in designing targeted therapy to improve sleep quality.
Similar content being viewed by others
References
Spoormaker VI, Montgomery P (2008) Disturbed sleep in post-traumatic stress disorder: secondary symptom or core feature? Sleep Med Rev 12(3):169–184. https://doi.org/10.1016/j.smrv.2007.08.008
Harvey AG, Jones C, Schmidt DA (2003) Sleep and posttraumatic stress disorder: a review. Clin Psychol Rev 23(3):377–407. https://doi.org/10.1016/s0272-7358(03)00032-1
Jordan BK, Marmar CR, Fairbank JA, Schlenger WE, Kulka RA, Hough RL, Weiss DS (1992) Problems in families of male Vietnam veterans with posttraumatic stress disorder. J Consult Clin Psychol 60(6):916–926
Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL (2004) Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 351(1):13–22. https://doi.org/10.1056/NEJMoa040603
Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL (1993) Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. J Consult Clin Psychol 61(6):984–991
Edmondson D, Richardson S, Falzon L, Davidson KW, Mills MA, Neria Y (2012) Posttraumatic stress disorder prevalence and risk of recurrence in acute coronary syndrome patients: a meta-analytic review. PLoS One 7(6):e38915. https://doi.org/10.1371/journal.pone.0038915
Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG (2019) Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of Sleep Medicine systematic review, meta-analysis, and GRADE assessment. J Clin Sleep Med 15(2):301–334. https://doi.org/10.5664/jcsm.7638
El-Solh AA, Vermont L, Homish GG, Kufel T (2017) The effect of continuous positive airway pressure on post-traumatic stress disorder symptoms in veterans with post-traumatic stress disorder and obstructive sleep apnea: a prospective study. Sleep Med 33:145–150. https://doi.org/10.1016/j.sleep.2016.12.025
Orr JE, Smales C, Alexander TH, Stepnowsky C, Pillar G, Malhotra A, Sarmiento KF (2017) Treatment of OSA with CPAP is associated with improvement in PTSD symptoms among veterans. J Clin Sleep Med 13(1):57–63. https://doi.org/10.5664/jcsm.6388
Marrone O, Salvaggio A, Bue AL, Bonanno A, Riccobono L, Insalaco G, Bonsignore MR (2011) Blood pressure changes after automatic and fixed CPAP in obstructive sleep apnea: relationship with nocturnal sympathetic activity. Clin Exp Hypertens 33(6):373–380. https://doi.org/10.3109/10641963.2010.531853
El-Solh AA, Ayyar L, Akinnusi M, Relia S, Akinnusi O (2010) Positive airway pressure adherence in veterans with posttraumatic stress disorder. Sleep 33(11):1495–1500. https://doi.org/10.1093/sleep/33.11.1495
Collen JF, Lettieri CJ, Hoffman M (2012) The impact of posttraumatic stress disorder on CPAP adherence in patients with obstructive sleep apnea. J Clin Sleep Med 8(6):667–672. https://doi.org/10.5664/jcsm.2260
Ratnavadivel R, Chau N, Stadler D, Yeo A, McEvoy RD, Catcheside PG (2009) Marked reduction in obstructive sleep apnea severity in slow wave sleep. J Clin Sleep Med 5(6):519–524
Eckert DJ, Younes MK (2014) Arousal from sleep: implications for obstructive sleep apnea pathogenesis and treatment. J Appl Physiol 116(3):302–313. https://doi.org/10.1152/japplphysiol.00649.2013
Gray EL, McKenzie DK, Eckert DJ (2017) Obstructive sleep apnea without obesity is common and difficult to treat: evidence for a distinct pathophysiological phenotype. J Clin Sleep Med 13(1):81–88. https://doi.org/10.5664/jcsm.6394
Zinchuk A, Edwards BA, Jeon S, Koo BB, Concato J, Sands S, Wellman A, Yaggi HK (2018) Prevalence, associated clinical features, and impact on continuous positive airway pressure use of a low respiratory arousal threshold among male United States veterans with obstructive sleep apnea. J Clin Sleep Med 14(5):809–817. https://doi.org/10.5664/jcsm.7112
Wallace DM, Wohlgemuth WK (2019) Predictors of insomnia severity index profiles in United States veterans with obstructive sleep apnea. J Clin Sleep Med 15(12):1827–1837. https://doi.org/10.5664/jcsm.8094
El-Solh AA, Adamo D, Kufel T (2018) Comorbid insomnia and sleep apnea in veterans with post-traumatic stress disorder. Sleep Breath 22(1):23–31. https://doi.org/10.1007/s11325-017-1618-y
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6):540–545
Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, Keane TM (2013) The clinician-administered PTSD scale for DSM-5 (CAPS-5). US Department of Veterans Affairs. Accessed 1/2/2020
Association AP (2013) Diagnostic and statistical manual of mental disorders, fifth edition (DSM-5). American Psychiatric Association, Washington, D.C.
Berry RB, Brooks R, Gramaldo C, Harding SM, Lloyd RM, Marcus CL, Vaughn BV (2017) The AASM manual for the scoring of sleep and associated events: rukes, terminology, and technical specifications. American Academy of Sleep Medicine, Darien
Edwards BA, Eckert DJ, McSharry DG, Sands SA, Desai A, Kehlmann G, Bakker JP, Genta PR, Owens RL, White DP, Wellman A, Malhotra A (2014) Clinical predictors of the respiratory arousal threshold in patients with obstructive sleep apnea. Am J Respir Crit Care Med 190(11):1293–1300. https://doi.org/10.1164/rccm.201404-0718OC
Marin JM, Carrizo SJ, Vicente E, Agusti AG (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 365(9464):1046–1053. https://doi.org/10.1016/S0140-6736(05)71141-7
Johns MW (2000) Sensitivity and specificity of the multiple sleep latency test (MSLT), the maintenance of wakefulness test and the Epworth sleepiness scale: failure of the MSLT as a gold standard. J Sleep Res 9(1):5–11
Weathers F, Litz B, Herman D, Huska J, Keane T (1993) The PTSD checklist: reliability, validity, & diagnositic utility. Paper presented at the Annual Meeting of the Internation Society of Traumatic Stress Studies, San Antonio, TX
Pietrzak RH, Tsai J, Armour C, Mota N, Harpaz-Rotem I, Southwick SM (2015) Functional significance of a novel 7-factor model of DSM-5 PTSD symptoms: results from the National Health and Resilience in Veterans study. J Affect Disord 174:522–526. https://doi.org/10.1016/j.jad.2014.12.007
Armour C, Tsai J, Durham TA, Charak R, Biehn TL, Elhai JD, Pietrzak RH (2015) Dimensional structure of DSM-5 posttraumatic stress symptoms: support for a hybrid Anhedonia and Externalizing Behaviors model. J Psychiatr Res 61:106–113. https://doi.org/10.1016/j.jpsychires.2014.10.012
El-Solh AA, Riaz U, Roberts J (2018) Sleep disorders in patients with posttraumatic stress disorder. Chest 154(2):427–439. https://doi.org/10.1016/j.chest.2018.04.007
Eckert DJ, White DP, Jordan AS, Malhotra A, Wellman A (2013) Defining phenotypic causes of obstructive sleep apnea. Identification of novel therapeutic targets. Am J Respir Crit Care Med 188(8):996–1004. https://doi.org/10.1164/rccm.201303-0448OC
Foster BK, Kravitz S, Collen J, Holley A (2019) Insomia among military members with OSA. Sleep 42:A196
Smith PR, Sheikh KL, Costan-Toth C, Forsthoefel D, Bridges E, Andrada TF, Holley AB (2017) Eszopiclone and zolpidem do not affect the prevalence of the low arousal threshold phenotype. J Clin Sleep Med 13(1):115–119. https://doi.org/10.5664/jcsm.6402
Capaldi VF 2nd, Guerrero ML, Killgore WD (2011) Sleep disruptions among returning combat veterans from Iraq and Afghanistan. Mil Med 176(8):879–888. https://doi.org/10.7205/milmed-d-10-00440
Caldwell JA, Knapik JJ, Lieberman HR (2017) Trends and factors associated with insomnia and sleep apnea in all United States military service members from 2005 to 2014. J Sleep Res 26(5):665–670. https://doi.org/10.1111/jsr.12543
Carberry JC, Jordan AS, White DP, Wellman A, Eckert DJ (2016) Upper airway collapsibility (Pcrit) and pharyngeal dilator muscle activity are sleep stage dependent. Sleep 39(3):511–521. https://doi.org/10.5665/sleep.5516
Younes M, Ostrowski M, Atkar R, Laprairie J, Siemens A, Hanly P (2007) Mechanisms of breathing instability in patients with obstructive sleep apnea. J Appl Physiol 103(6):1929–1941. https://doi.org/10.1152/japplphysiol.00561.2007
Smith S, Sullivan K, Hopkins W, Douglas J (2004) Frequency of insomnia report in patients with obstructive sleep apnoea hypopnea syndrome (OSAHS). Sleep Med 5(5):449–456. https://doi.org/10.1016/j.sleep.2004.03.005
Wichniak A, Wierzbicka A, Walecka M, Jernajczyk W (2017) Effects of antidepressants on sleep. Curr Psychiatry Rep 19(9):63. https://doi.org/10.1007/s11920-017-0816-4
Fava M (2004) Daytime sleepiness and insomnia as correlates of depression. J Clin Psychiatry 65(Suppl 16):27–32
Decision Memo for Continuous Positive Airway Pressure (CPAP) Therapy for Obstructive Sleep Apnea (OSA) (CAG-00093N) (October 30, 2001). Centers for Medicare and Medicaid Services
Koo BB, Wiggins R, Molina C (2012) REM rebound and CPAP compliance. Sleep Med 13(7):864–868. https://doi.org/10.1016/j.sleep.2012.03.019
Verma A, Radtke RA, VanLandingham KE, King JH, Husain AM (2001) Slow wave sleep rebound and REM rebound following the first night of treatment with CPAP for sleep apnea: correlation with subjective improvement in sleep quality. Sleep Med 2(3):215–223. https://doi.org/10.1016/s1389-9457(00)00069-1
Smales ET, Edwards BA, Deyoung PN, McSharry DG, Wellman A, Velasquez A, Owens R, Orr JE, Malhotra A (2015) Trazodone effects on obstructive sleep apnea and non-REM arousal threshold. Ann Am Thorac Soc 12(5):758–764. https://doi.org/10.1513/AnnalsATS.201408-399OC
Eckert DJ, Owens RL, Kehlmann GB, Wellman A, Rahangdale S, Yim-Yeh S, White DP, Malhotra A (2011) Eszopiclone increases the respiratory arousal threshold and lowers the apnoea/hypopnoea index in obstructive sleep apnoea patients with a low arousal threshold. Clin Sci (Lond) 120(12):505–514. https://doi.org/10.1042/CS20100588
Carter SG, Berger MS, Carberry JC, Bilston LE, Butler JE, Tong BK, Martins RT, Fisher LP, McKenzie DK, Grunstein RR, Eckert DJ (2016) Zopiclone increases the arousal threshold without impairing genioglossus activity in obstructive sleep apnea. Sleep 39(4):757–766. https://doi.org/10.5665/sleep.5622
Jordan AS, O'Donoghue FJ, Cori JM, Trinder J (2017) Physiology of arousal in obstructive sleep apnea and potential impacts for sedative treatment. Am J Respir Crit Care Med 196(7):814–821. https://doi.org/10.1164/rccm.201612-2511PP
Agnew HW Jr, Webb WB, Williams RL (1966) The first night effect: an EEG study of sleep. Psychophysiology 2(3):263–266. https://doi.org/10.1111/j.1469-8986.1966.tb02650.x
Funding
This study was partially funded by a Merit Review Award from the U.S. Department of Veterans Affairs (CX001656).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
AES has received funding from the US Department of Veterans Affairs. All other authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The VA Western New York Healthcare System Institutional Review Board approved this study.
Disclaimer
The contents of this paper do not represent the views of the Department of Veterans Affairs or the United States Government.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
El-Solh, A.A., Lawson, Y. & Wilding, G.E. Impact of low arousal threshold on treatment of obstructive sleep apnea in patients with post-traumatic stress disorder. Sleep Breath 25, 597–604 (2021). https://doi.org/10.1007/s11325-020-02106-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-020-02106-0