Abstract
Background
Peritoneal dialysis (PD) patients with preserved residual diuresis have a lower risk of death and complications. Here we analyzed associations between residual diuresis and presence of fluid overload and biomarkers of cardiac strain and nutrition in PD patients.
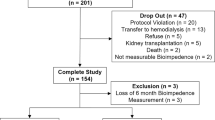
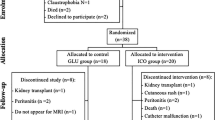
Methods
Among 44 PD patients placed into three subgroups, depending on volume of residual diuresis (group A ≤ 500; group B 600–1900; and group C ≥ 2000 mL/day), we examined: overhydration (OH) assessed by bioimpedance analysis (BIA; yielding OH index OHBIA) and by clinical criteria (edema and hypertension); nutritional status (by subjective global assessment, SGA); metabolic status (electrolytes, serum lipid profile, CRP, and albumin); biomarkers of fluid overload and cardiac strain (N-terminal probrain natriuretic peptide, NT-proBNP, and troponin T, TnT); and, echocardiography and chest X-ray.
Results
With increasing residual diuresis in group A, B and C, fewer patients had signs of overhydration defined as OHBIA > 1.1 L (75.0, 42.9 and 33.3 %) or peripheral edema (25.0, 21.4 and 0 %) and NT-proBNP (15199 ± 16150 vs. 5930 ± 9256 vs. 2600 ± 3907 pg/mL; p < 0.05) and TnT (0.15 ± 0.17 vs. 0.07 ± 0.09 vs. 0.04 ± 0.03 ng/mL; p < 0.05) were significantly lower. Significant differences were found also in ejection fraction, SGA, and total cholesterol, albumin and hemoglobin levels whereas blood pressures and serum CRP did not differ significantly.
Conclusion
Signs of OH and cardiac strain are common in PD patients, even in those with diuresis of 1000–2000 mL/day and with no clinical signs or symptoms, suggesting that even moderate decrease in residual renal function in PD patients associate with OH and other complications.
Similar content being viewed by others
References
Marron B, Remon C, Perez-Fontan M, Quiros P, Ortiz A (2008) Benefits of preserving residual renal function in peritoneal dialysis. Kidney Int Suppl 108:S42–S51
Chandna SM, Farrington K (2004) Residual renal function: considerations on its importance and preservation in dialysis patients. Semin Dial 17(3):196–201
Lysaght MJ, Vonesh EF, Gotch F, Ibels L, Keen M, Lindholm B et al (1991) The influence of dialysis treatment modality on the decline of remaining renal function. ASAIO Trans/Am Soc Artif Intern Organs 37(4):598–604
Moist LM, Port FK, Orzol SM, Young EW, Ostbye T, Wolfe RA et al (2000) Predictors of loss of residual renal function among new dialysis patients. J Am Soc Nephrol: JASN 11(3):556–564
Misra M, Vonesh E, Van Stone JC, Moore HL, Prowant B, Nolph KD (2001) Effect of cause and time of dropout on the residual GFR: a comparative analysis of the decline of GFR on dialysis. Kidney Int 59(2):754–763
Lang SM, Bergner A, Topfer M, Schiffl H (2001) Preservation of residual renal function in dialysis patients: effects of dialysis-technique-related factors. Perit Dial Int 21(1):52–57
Jansen MA, Hart AA, Korevaar JC, Dekker FW, Boeschoten EW, Krediet RT et al (2002) Predictors of the rate of decline of residual renal function in incident dialysis patients. Kidney Int 62(3):1046–1053
Diaz-Buxo JA, White SA, Himmele R (2013) The importance of residual renal function in peritoneal dialysis patients. Adv Perit Dial 29:19–24
Wang AY, Wang M, Woo J, Lam CW, Lui SF, Li PK et al (2004) Inflammation, residual kidney function, and cardiac hypertrophy are interrelated and combine adversely to enhance mortality and cardiovascular death risk of peritoneal dialysis patients. J Am Soc Nephrol 15(8):2186–2194
Han SH, Lee SC, Ahn SV, Lee JE, Kim DK, Lee TH et al (2007) Reduced residual renal function is a risk of peritonitis in continuous ambulatory peritoneal dialysis patients. Nephrol Dial Transplant 22(9):2653–2658
Rivera-Gorrin M, Teruel-Briones JL, Rodriguez-Mendiola N, Diaz-Dominguez M, Ruiz-Roso G, Quereda-Rodriguez-Navarro C (2014) Residual renal function in patients on peritoneal dialysis: effect of peritonitis episodes. Nefrologia 34(6):802–804
Diaz-Buxo JA, Lowrie EG, Lew NL, Zhang SM, Zhu X, Lazarus JM (1999) Associates of mortality among peritoneal dialysis patients with special reference to peritoneal transport rates and solute clearance. Am J Kidney Dis 33(3):523–534
Szeto CC, Lai KN, Wong TY, Law MC, Leung CB, Yu AW et al (1999) Independent effects of residual renal function and dialysis adequacy on nutritional status and patient outcome in continuous ambulatory peritoneal dialysis. Am J Kidney Dis 34(6):1056–1064
Rocco M, Soucie JM, Pastan S, McClellan WM (2000) Peritoneal dialysis adequacy and risk of death. Kidney Int 58(1):446–457
Bargman JM, Thorpe KE, Churchill DN, Group CPDS (2001) Relative contribution of residual renal function and peritoneal clearance to adequacy of dialysis: a reanalysis of the CANUSA study. J Am Soc Nephrol 12(10):2158–2162
Paniagua R, Amato D, Vonesh E, Correa-Rotter R, Ramos A, Moran J et al (2002) Effects of increased peritoneal clearances on mortality rates in peritoneal dialysis: ADEMEX, a prospective, randomized, controlled trial. J Am Soc Nephrol: JASN 13(5):1307–1320
Kalantar-Zadeh K, Kleiner M, Dunne E, Lee GH, Luft FC (1999) A modified quantitative subjective global assessment of nutrition for dialysis patients. Nephrol Dial Transplant 14(7):1732–1738
Maiorca R, Brunori G, Zubani R, Cancarini GC, Manili L, Camerini C et al (1995) Predictive value of dialysis adequacy and nutritional indices for mortality and morbidity in CAPD and HD patients: a longitudinal study. Nephrol Dial Transplant 10(12):2295–2305
Szeto CC, Wong TY, Leung CB, Wang AY, Law MC, Lui SF et al (2000) Importance of dialysis adequacy in mortality and morbidity of chinese CAPD patients. Kidney Int 58(1):400–407
Remon C, Quiros PL, Perez Banasco V, Toran D, Tejuca F, Merino MJ et al (2006) Report of the Andalusian registry of patients with end stage renal disease in treatment with peritoneal dialysis: period 1999–2004. Nefrologia 26(1):45–55
Konings CJ, Kooman JP, Schonck M, Struijk DG, Gladziwa U, Hoorntje SJ et al (2003) Fluid status in CAPD patients is related to peritoneal transport and residual renal function: evidence from a longitudinal study. Nephrol Dial Transplant 18(4):797–803
Matsuda A, Matsumura O, Ogawa T, Tayama Y, Motojima M, Maeda T et al (2010) Contribution of residual renal function on peritoneal solute transport in dialysis patients. Am J Nephrol 32(3):187–193
Van Biesen W, Williams JD, Covic AC, Fan S, Claes K, Lichodziejewska-Niemierko M et al (2011) Fluid status in peritoneal dialysis patients: the European body composition monitoring (EuroBCM) study cohort. PLoS One 6(2):e17148
Cader RA, Ibrahim OA, Paul S, Gafor HA, Mohd R (2014) Left ventricular hypertrophy and chronic fluid overload in peritoneal dialysis patients. Int Urol Nephrol 46(6):1209–1215
Avila-Diaz M, Ventura MD, Valle D, Vicente-Martinez M, Garcia-Gonzalez Z, Cisneros A et al (2006) Inflammation and extracellular volume expansion are related to sodium and water removal in patients on peritoneal dialysis. Perit Dial Int 26(5):574–580
Ates K, Nergizoglu G, Keven K, Sen A, Kutlay S, Erturk S et al (2001) Effect of fluid and sodium removal on mortality in peritoneal dialysis patients. Kidney Int 60(2):767–776
Wang AY, Sea MM, Ip R, Law MC, Chow KM, Lui SF et al (2001) Independent effects of residual renal function and dialysis adequacy on actual dietary protein, calorie, and other nutrient intake in patients on continuous ambulatory peritoneal dialysis. J Am Soc Nephrol 12(11):2450–2457
Aguilera A, Codoceo R, Selgas R, Garcia P, Picornell M, Diaz C et al (1998) Anorexigen (TNF-alpha, cholecystokinin) and orexigen (neuropeptide Y) plasma levels in peritoneal dialysis (PD) patients: their relationship with nutritional parameters. Nephrol Dial Transplant 13(6):1476–1483
Liu Y, Coresh J, Eustace JA, Longenecker JC, Jaar B, Fink NE et al (2004) Association between cholesterol level and mortality in dialysis patients: role of inflammation and malnutrition. JAMA, J Am Med Assoc 291(4):451–459
Kagan A, Elimalech E, Lemer Z, Fink A, Bar-Khayim Y (1997) Residual renal function affects lipid profile in patients undergoing continuous ambulatory peritoneal dialysis. Perit Dial Int 17(3):243–249
Palomo-Pinon S, Mora-Villalpando CJ, Del Carmen Prado-Uribe M, Ceballos-Reyes GM, De Jesus Ventura-Garcia M, Avila-Diaz M et al (2014) Inflammation and myocardial damage markers influence loss of residual renal function in peritoneal dialysis patients. Arch Med Res 45(6):484–488
Wang AY, Woo J, Wang M, Sea MM, Sanderson JE, Lui SF et al (2005) Important differentiation of factors that predict outcome in peritoneal dialysis patients with different degrees of residual renal function. Nephrol Dial Transplant 20(2):396–403
Pecoits-Filho R, Heimburger O, Barany P, Suliman M, Fehrman-Ekholm I, Lindholm B et al (2003) Associations between circulating inflammatory markers and residual renal function in CRF patients. Am J Kidney Dis 41(6):1212–1218
Zhang F, Liu H, Gong X, Liu F, Peng Y, Cheng M et al (2015) Risk factors for mortality in Chinese patients on continuous ambulatory peritoneal dialysis. Perit Dial Int 35(2):199–205
Unsal A, Koc Y, Basturk T, Sakaci T, Ahbap E, Sinangil A et al (2013) Clinical outcomes and mortality in peritoneal dialysis patients: a 10-year retrospective analysis in a single center. Clin Nephrol 80(4):270–279
Wang AY, Wang M, Woo J, Law MC, Chow KM, Li PK et al (2002) A novel association between residual renal function and left ventricular hypertrophy in peritoneal dialysis patients. Kidney Int 62(2):639–647
Wang AY, Lam CW, Wang M, Chan IH, Lui SF, Zhang Y et al (2009) Diagnostic potential of serum biomarkers for left ventricular abnormalities in chronic peritoneal dialysis patients. Nephrol Dial Transplant 24(6):1962–1969
Lee JA, Kim DH, Yoo SJ, Oh DJ, Yu SH, Kang ET (2006) Association between serum n-terminal pro-brain natriuretic peptide concentration and left ventricular dysfunction and extracellular water in continuous ambulatory peritoneal dialysis patients. Perit Dial Int 26(3):360–365
Saunders JT, Nambi V, de Lemos JA, Chambless LE, Virani SS, Boerwinkle E et al (2011) Cardiac troponin T measured by a highly sensitive assay predicts coronary heart disease, heart failure, and mortality in the atherosclerosis risk in communities study. Circulation 123(13):1367–1376
Bansal N, Hyre Anderson A, Yang W, Christenson RH, deFilippi CR, Deo R et al (2015) High-sensitivity troponin T and N-terminal Pro-B-type natriuretic peptide (NT-proBNP) and risk of incident heart failure in patients with CKD: the chronic renal insufficiency cohort (CRIC) study. J Am Soc Nephrol 26(4):946–956
Bansal N, Hyre Anderson A, Yang W, Christenson RH, deFilippi CR, Deo R et al (2015) High-sensitivity troponin T and N-terminal pro-B-type natriuretic peptide (NT-proBNP) and risk of incident heart failure in patients with CKD: the chronic renal insufficiency cohort (CRIC) study. J Am Soc Nephrol: JASN 26(4):946–956
Caliskan Y, Ozkok A, Akagun T, Alpay N, Guz G, Polat N et al (2012) Cardiac biomarkers and noninvasive predictors of atherosclerosis in chronic peritoneal dialysis patients. Kidney Blood Press Res 35(5):340–348
Lowbeer C, Gutierrez A, Gustafsson SA, Norrman R, Hulting J, Seeberger A (2002) Elevated cardiac troponin T in peritoneal dialysis patients is associated with CRP and predicts all-cause mortality and cardiac death. Nephrol Dial Transplant 17(12):2178–2183
Oh HJ, Lee MJ, Kwon YE, Park KS, Park JT, Han SH et al (2015) Which biomarker is the best for predicting mortality in incident peritoneal dialysis patients: NT-ProBNP, Cardiac TnT, or hsCRP?—a prospective observational study. Medicine 94(44):e1636
Buckalew VM Jr, Berg RL, Wang SR, Porush JG, Rauch S, Schulman G (1996) Prevalence of hypertension in 1,795 subjects with chronic renal disease: the modification of diet in renal disease study baseline cohort—modification of diet in renal disease study group. Am J Kidney Dis 28(6):811–821
Menon MK, Naimark DM, Bargman JM, Vas SI, Oreopoulos DG (2001) Long-term blood pressure control in a cohort of peritoneal dialysis patients and its association with residual renal function. Nephrol Dial Transplant 16(11):2207–2213
Acknowledgments
We thank patients who participated in the study and staff that collected the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Bengt Lindholm is employed by Baxter Healthcare. Baxter Novum is the result of a grant from Baxter Healthcare to Karolinska Institutet.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the Bioethical Committee of the Poznan University of Medical Sciences and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Sikorska, D., Pawlaczyk, K., Olewicz-Gawlik, A. et al. The importance of residual renal function in peritoneal dialysis. Int Urol Nephrol 48, 2101–2108 (2016). https://doi.org/10.1007/s11255-016-1428-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-016-1428-3