Abstract
Purpose
Functional vitamin K deficiency (both K1 and K2) is postulated to be one of the most relevant links between chronic kidney disease and vascular calcification in hemodialysis (HD) patients. Recommended dietary restrictions in HD patients superimposed on diversity of eating habits across the countries may affect the prevalence of functional vitamin K deficiency. The aim of this study was to determine the level of functional vitamin K deficiency and its relation to vitamin K1 intake in HD patients in Upper Silesia in Poland.
Methods
Protein-induced vitamin K absence or antagonist-II (PIVKA-II) and undercarboxylated matrix Gla protein (ucMGP) were assessed by ELISA in 153 stable, prevalent HD patients and 20 apparently healthy adults (to establish normal ranges for PIVKA-II and ucMGP). Daily phylloquinone intake was assessed using a food frequency questionnaire.
Results
PIVKA-II and ucMGP levels were increased in 27.5 and 77.1 % of HD patients in comparison with the reference ranges in apparently healthy controls, respectively. In 45 % of cases, the increased PIVKA-II level was explained by insufficient phylloquinone intake for Polish population (recommended intake: >55 μg for women and >65 µg for men). Applying ROC analysis, we showed that vitamin K1 intake below 40.2 µg/day was associated with increased PIVKA-II levels. There was no correlation between vitamin K1 intake and plasma concentration of ucMGP, or between PIVKA-II and ucMGP.
Conclusions
(1) Functional vitamin K1 deficiency is explained by low vitamin K1 intake in less than half of HD patients. (2) Undercarboxylated matrix Gla protein level is a poor surrogate for functional vitamin K1 deficiency.
Similar content being viewed by others
Introduction
Cardiovascular diseases (coronary artery disease, congestive heart failure, arrhythmias or sudden cardiac death) are the main causes of morbidity and mortality in patients with chronic kidney disease (CKD). Increased mortality in hemodialysis (HD) patients often is associated with accelerated atherosclerosis and excessive vascular calcification [1]. Increased risk of the development of cardiovascular calcification in patients with CKD can only partly be explained by the presence of established risk factors such dyslipidemia, hypertension, smoking habit or diabetes [2, 3]. Functional deficiency of proteins involved in the regulation of calcium metabolism is probably a crucial mechanism for this process [2]. A direct link between the decreased availability of vitamin K and vascular calcification has been suggested by numerous studies [4–7]. The term ‘vitamin K’ refers to a group of compounds consisting of the plant form, phylloquinone (vitamin K1), the bacterial form, the menaquinones (MK, vitamin K2) and a synthetic form, menadione (vitamin K3), which is also an intermediate in vitamin K metabolism [8].
Recent studies indicate both low vitamin K intake and functional vitamin K deficiency among patients receiving renal replacement therapy [9–11]. Vitamin K intake is affected by low-potassium and low-phosphorus recommended diet in HD patients. According to Cranenburg et al. [12], mean daily vitamin K1 intake in HD patients was 118 μg and mean vitamin K2 intake was 21 μg. Most of the studies using HPLC methods showed undetectable or very low concentrations of menaquinones (especially MK-4) in HD patients [12, 13].
Deficiency of vitamin K, either due to diminished intake or the use of coumarin derivatives, results in undercarboxylation of vitamin K-dependent proteins (VKDPs) [14]. This includes several proteins involved in the regulation of the process of calcification—matrix Gla protein (MGP) and osteocalcin (OC) [14, 15]. The optimal daily vitamin K intake required to activate VKDPs has not been determined; however, data from interventional studies on vitamin K supplementation suggest benefits of this approach [7].
MGP is a calcification inhibitor expressed by vascular smooth muscle cells in the vasculature. To obtain MGP function—inhibition of bone morphogenetic protein 2 (BMP-2), γ-carboxylation of its five residues with the presence of vitamin K as a co-factor is required [16]. The degree of carboxylation required for MGP function is not known. The uncarboxylated form of MGP (ucMGP) does not inhibit the process of vascular calcification; thus, plasma levels of ucMGP reflect the availability of vitamin K in the vessel wall [6]. The accumulation of ucMGP in atherosclerotic lesions and areas of calcification has been reported in several studies [16, 17]. According to Cranenburg et al. [2], the circulating fraction of ucMGP may be decreased in the presence of arterial calcification due to the increased ucMGP accumulation observed in calcified tissues in HD patients; however, the exact mechanism of this process has not been described as yet.
A marker commonly used for the assessment of functional vitamin K (mostly vitamin K1) deficiency is the plasma level of protein induced by vitamin K absence or antagonist-II (PIVKA-II). PIVKA-II is a liver-derived VKDP that reflects vitamin K status [2]. According to several recent studies, half of HD patients have subclinical vitamin K deficiency, demonstrated by increased circulating levels of PIVKA-II. Lee et al. [18] showed that 73 % of patients with chronic renal failure had hepatic vitamin K deficiency with elevated PIVKA-II concentrations (>2 ng/mL, mean value 4.48 ng/mL). Recommended dietary restrictions in HD patients superimposed on diversity of eating habits across the countries may affect the prevalence of functional vitamin K deficiency.
The aim of this study was to determine the level of functional vitamin K deficiency and its relation to vitamin K1 intake in HD patients in Upper Silesia in Poland.
Subjects and methods
A total of 153 stable, prevalent HD patients (93 men and 60 women) were included in the study. Patients on HD therapy for less than 6 months, hospitalized patients, patients taking vitamin K antagonists and those with a previous history of gastrointestinal disturbances were excluded from the study. The study protocol was accepted by the local bioethical committee (KNW-2-015/N/3/K). Informed consent was obtained from all individual participants included in the study. The study did not include training with a nutritionist and did not interfere with previous nutritional recommendations.
All HD patients were receiving dialysis three times per week for 3.5 to 5 h (11.7 ± 0.9 h weekly). HD patient characteristics including causes of CKD, duration of HD therapy and Kt/V are given in Table 1. The control group consisted of 20 apparently healthy adults (10 men and 10 women) of similar age to the HD patients, with normal kidney function.
The study protocol involved obtaining additional blood samples while performing routine tests (blood count, urea, calcium, phosphate, sodium, potassium) before a midweek HD session and after an overnight fast. Only patients on morning HD sessions were recruited.
Measurements
Protein-induced vitamin K absence or antagonist-II (PIVKA-II) and ucMGP were assessed by ELISA using commercially available kits (Cusabio, Wuhan, China) with intra-assay and inter-assay coefficients of variability below 8 and 10 %, respectively (for both kits). Detection ranges for PIVKA-II and ucMGP were 0.312–20 and 0.156–10 ng/mL, while the lower limit of detection was 0.078–0.039 ng/mL (according to manufacturer), respectively. For ucMGP determination, 5000-fold dilution was used.
We established the normal ranges for PIVKA-II and ucMGP as the values of the 95 % confidence interval around the mean in 20 apparently healthy adult subjects: 0.37–0.66 ng/mL and 5.1–9.2 mg/mL, respectively.
Daily phylloquinone intake assessment
Daily phylloquinone, calciferol, calcium, phosphate, sodium, magnesium, iron and potassium, as well as energy and macronutrients intakes (fat, carbohydrates, protein, cholesterol, dietary fiber), were assessed on the basis of a Diet History Questionnaire II (DHQ)—a freely available food frequency questionnaire (FFQ) developed by staff at the Risk Factor Monitoring and Methods Branch (RFMMB). For a purpose of this study, a past year with portion size version of the questionnaire was used. Patients were asked 134 food item and eight dietary supplement past-year intake questions with questions included about portion size. Before receiving the FFQ, each participant was instructed orally about completing the form and printed instructions were also provided. FFQ records were reviewed for completeness.
Statistical analysis
Statistical analysis was performed with Statistica 10.0 PL Stat Soft Corporation software (www.statsoft.com). The normality of quantitative variables distribution was checked by the Shapiro–Wilk test. Variables with skewed distributions (e.g., vitamin K1 intake) were logarithmically transformed for correlation analyses. Results are given as mean values with standard deviations or 95 % confidence intervals (95 % CI), or medians with interquartile ranges. For comparison of groups, we used the χ 2 test (qualitative variables) and ANOVA, followed by Tukey’s test (quantitative variables). The adequacy of statistical power of these analyses was controlled (>0.8). Correlation coefficients were calculated according to Pearson. The receiver operating characteristic (ROC) was used for the establishment of daily K1 intake resulting in increased plasma PIVKA-II levels (greater than established reference range for healthy individuals—95 percentile).
Values of p < 0.05 were considered to be statistically significant.
Results
Plasma concentration of PIVKA-II and ucMGP
The mean plasma concentration of PIVKA-II in HD patients was 0.59 (0.51–0.68) ng/mL (Table 2) and was not significantly different than in healthy subjects—0.51 (0.37–0.66) ng/mL. Increased plasma PIVKA-II concentrations (>0.66 ng/mL) were found in 42 of the HD patients (27.5 %). Additionally, plasma concentration of ucMGP in HD patients was significantly (p < 0.001) greater than in healthy subjects [17.9 (16.3–19.5) vs. 7.1 (5.1–9.2) mg/mL]; increased levels (>9.2 mg/mL) were found in 118 of the HD patients (77.1 %).
Daily K1 intake
Median (interquartile range) K1 intake in HD patients was 103 (43,221) µg (Table 3). No difference was found in vitamin K1 intake between men and women. However, the intake was lower than recommended for the Polish population (at least 65 µg/day for men and 55 µg/day for women [15]) in 32 % of HD patients. The intake of vitamin K1 was most strongly related to the consumption of protein (R = 0.560, p < 0.001), fiber (R = 0.664, p < 0.001) and magnesium (R = 0.601, p < 0.001). In addition, daily K1 intake was proportional to the serum level of HDL cholesterol (R = 0.196, p < 0.05).
Functional vitamin K deficiency and vitamin K1 intake
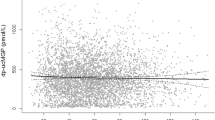
The subgroup of HD patients with increased PIVKA-II levels was characterized by lower daily K1 intake (Table 3). The receiver operator curve (ROC) analysis revealed that increased plasma concentration of PIVKA-II was characteristic of participants with a daily K1 intake of less than 40.2 µg per day (with 38.7 % sensitivity and 84 % specificity)—Fig. 1.
The second ROC analysis showed that HD patients with daily vitamin K1 intake over 98.1 µg/day are characterized by lower risk of increased PIVKA-II levels (with 65.0 % sensitivity and 51.2 % specificity). Approximately 25 % of patients with such an intake had increased PIVKA-II levels.
Functional vitamin K deficiency and ucMGP levels
The levels of ucMGP were similar in patients with and without functional vitamin K deficiency—17.2 (14.2–20.2) versus 18.4 (16.5–20.3) mg/mL; NS. Additionally, there was no correlation between plasma concentration of ucMGP and PIVKA-II (R = −0.016, p = 0.85) and between ucMGP and daily K1 intake (R = 0.028, p = 0.77).
Discussion
The results of our study increase the knowledge concerning the regional variability of the prevalence of functional vitamin K deficiency in HD patients and indicate the need for the standardization of methods used for its assessment.
There are only a few studies assessing vitamin K intake and status in HD patients in the literature [2, 5, 9, 18, 19]. A recent study by Holden and co-workers in 172 subjects with stage 3–5 CKD showed that the criteria for subclinical vitamin K deficiency were met by 6 % of the patients based on circulating K1 measurements, by 60 % based on OC carboxylation and by 97 % based on PIVKA-II levels [9]. In a population of 24 HD patients, Lee et al. showed elevated PIVKA-II concentrations in 73 %, while Schlieper et al. described abnormal PIVKA-II concentrations in 64 % of HD patients [5, 18]. In our study, functional vitamin K deficiency was demonstrated by increased plasma PIVKA-II concentrations in 27.5 % of HD patients. Our data are more similar to those obtained by Nerlander et al. [19] who found vitamin K deficiency based upon PIVKA-II measurements in 14.6 % of patients (with 60 % of patients treated with warfarin). The observed variation of the obtained results is mostly related to the shortcomings in the methodology (probably limited specificity of antibodies to recognition uncarboxylated and carboxylated proteins) for functional vitamin K assessment, including measurements of PIVKA-II concentration with commercially available ELISA kits. We cannot exclude that some variation is related to diverse vitamin K intake related to traditional choices of food by specific populations.
In the present study, we utilized an ELISA kit from Cusabio. HD patients with increased plasma concentration of PIVKA-II (>0.66 ng/mL) had markedly lower daily vitamin K1 intake (less than 40.2 µg/day) than recommended for the Polish population (>55 μg for women and >65 µg for men). However, among HD patients with increased PIVKA levels, 55 % had adequate dietary vitamin K1 intake. Higher daily vitamin K1 intake (over 98.1 µg/day) was needed to prevent vitamin K deficiency defined by increased PIVKA-II concentration. In a subgroup with greater intake, increased PIVKA-II levels were observed in a quarter of patients. These data suggest that other factors may also contribute to disturbed vitamin K1 metabolism in HD patients, leading to subclinical functional vitamin K1 deficiency: e.g., gut microbiota composition, impaired vitamin K absorption or disturbed metabolism. It should be stressed that numerous studies have found adequate vitamin K intake in the majority of HD patients.
According to Cranenburg et al. [12], mean dietary vitamin K1 intake among HD patients in the Netherlands was 118 μg/day (18–494) and for vitamin K2 was 21 μg/day (2–68). Those data are similar to values obtained in the present study (phylloquinone intake 103 [43–221] µg/day) with 32 % of patients not meeting recommended phylloquinone intake for the Polish population. It should be stressed that the food frequency questionnaire that was used in this study does not allow us to determine vitamin K2 intake. We have recently performed a study in 85 HD patients using a three-day food diary that showed mean vitamin K1 and MK-4 intake of 98.8 (90–108) and 28.5 (26.2–30.8) μg/day, respectively [13].
Specific diet suggestions for HD patients (low-phosphorus and low-potassium diet) may lead to decreased intake of green vegetables (the main source of phylloquinone) and dairy products (the primary source for menaquinones) that can cause nutritional vitamin K deficiency. However, the compliance with dietary recommendations is usually low.
The process of γ-carboxylation with the participation of vitamin K allows MGP bioactivity to be used as a calcification inhibitor. Our data failed to prove that functional deficiency of vitamin K influences ucMGP levels in HD patients. Unexpectedly, plasma ucMGP concentrations were significantly greater than in healthy subjects (17.9 [16.3–19.5] vs. 7.1 [5.1–9.2] mg/mL; p < 0.001). The sparse available published data on ucMGP concentrations in HD patients, published by a single group, are somewhat contradictory results. According to the data from the Heart and Soul Study, decreased serum ucMGP level is associated with reduced glomerular filtration rate [20]. Study by Cranenburg et al. showed markedly lower ucMGP concentrations in HD patients with the lowest values observed in a group with calciphylaxis compared with reference population [2]. In two subsets of HD patients (N = 40 and N = 120), the same group showed levels of ucMGP in HD patients (193 ± 65 and 173 ± 70 nM/L, respectively) were lower by about 50 % than in apparently healthy subjects of the same age (441 ± 97 and 424 ± 126 nM/L, respectively) [21, 22]. We cannot exclude that the differences found are the consequence of the methodology for ucMGP measurements used by us and by Schurgers’ group.
However, in line with our data, more studies have described elevated concentrations of dephosphorylated-uncarboxylated MGP (dp-ucMGP) in HD patients [5–7, 12, 23, 24]. It should be stressed that only ucMGP and dp-ucMGP could be measured in plasma, and the function of phosphorylation of MGP is, as yet, unknown, though some data indicate that it may play a role in regulating the secretion of proteins into the extracellular environment [25]. We did not determine dp-ucMGP concentrations, and this may be considered to be a limitation of our study.
MGP is produced by vascular smooth muscle cells and is subsequently γ-carboxylated in the presence of vitamin K. It is suggested that this process is more dependent on menaquinone than phylloquinone [16]. In line with this hypothesis, we have shown that ucMGP is not a surrogate marker of functional vitamin K deficiency, as we have observed similar values in a subgroup with normal and increased PIVKA-II levels.
The main limitation of the study was the lack of measurement of phylloquinone levels in serum samples. We did not determine vitamin K2 intake due to limitations of the food frequency questionnaire. Additionally, due to a small number of subjects, vitamin K intake in the control group was not assessed, as it may not accurately reflect vitamin K1 intake in healthy Polish adult population.
In conclusion, we have shown that functional vitamin K1 deficiency is explained by low vitamin K1 intake itself in less than half of HD patients and that ucMGP level is a poor surrogate of functional vitamin K1 deficiency.
References
Di Lullo L, House A, Gorini A et al (2015) Chronic kidney disease and cardiovascular complications. Heart Fail Rev 20:259–272
Cranenburg EC, Vermeer C, Koos R et al (2008) The circulating inactive form of matrix Gla Protein (ucMGP) as a biomarker for cardiovascular calcification. J Vasc Res 45:427–436
Santoro A, Mandreoli M (2014) Chronic renal disease and risk of cardiovascular morbidity-mortality. Kidney Blood Press Res 39:142–146
Schlieper G, Brandenburg V, Djuric Z et al (2009) Risk factors for cardiovascular calcifications in non-diabetic Caucasian haemodialysis patients. Kidney Blood Press Res 32:161–168
Schlieper G, Westenfeld R, Krüger T et al (2011) Circulating nonphosphorylated carboxylated matrix gla protein predicts survival in ESRD. J Am Soc Nephrol 22:387–395
Delanaye P, Krzesinski JM, Warling X et al (2014) Dephosphorylated-uncarboxylated matrix Gla protein concentration is predictive of vitamin K status and is correlated with vascular calcification in a cohort of hemodialysis patients. BMC Nephrol 15:145
Caluwé R, Vandecasteele S, Van Vlem B, Vermeer C, De Vriese AS (2014) Vitamin K2 supplementation in haemodialysis patients: a randomized dose-finding study. Nephrol Dial Transplant 29:1385–1390
Booth SL, Al Rajabi A (2008) Determinants of vitamin K status in humans. Vitam Horm 78:1–22
Pilkey RM, Morton AR, Boffa MB et al (2007) Subclinical vitamin K deficiency in hemodialysis patients. Am J Kidney Dis 49:432–439
Holden RM, Iliescu E, Morton AR, Booth SL (2008) Vitamin K status of Canadian peritoneal dialysis patients. Perit Dial Int 28:415–418
Holden RM, Morton AR, Garland JS, Pavlov A, Day AG, Booth SL (2010) Vitamins K and D status in stages 3–5 chronic kidney disease. Clin J Am Soc Nephrol 5:590–597
Cranenburg EC, Schurgers LJ, Uiterwijk HH et al (2012) Vitamin K intake and status are low in hemodialysis patients. Kidney Int 82:605–610
Wyskida K, Żak-Gołąb A, Łabuzek K et al (2015) Daily intake and serum concentration of menaquinone-4 (MK-4) in hemodialysis patients with chronic kidney disease. Clin Biochem 48:1246–1251
Schurgers LJ, Uitto J, Reutelingsperger CP (2013) Vitamin K-dependent carboxylation of matrix Gla-protein: a crucial switch to control ectopic mineralization. Trends Mol Med 19:217–226
Sadler JE (2004) Medicine: K is for koagulation. Nature 427:493–494
Schurgers LJ, Teunissen KJ, Knapen MH et al (2005) Novel conformation-specific antibodies against matrix gamma-carboxyglutamic acid (Gla) protein: undercarboxylated matrix Gla protein as marker for vascular calcification. Arterioscler Thromb Vasc Biol 25:1629–1633
Shroff RC, McNair R, Figg N et al (2008) Dialysis accelerates medial vascular calcification in part by triggering smooth muscle cell apoptosis. Circulation 118:1748–1757
Lee IJ, Hilliard B, Swami A et al (2012) Growth arrest-specific gene 6 (Gas6) levels are elevated in patients with chronic renal failure. Nephrol Dial Transplant 27:4166–4172
Nerlander M, Voong K, Manghat P et al (2009) Subclinical deficiency of vitamin K status in chronic kidney disease. World Congress of Nephrology (Poster session), Milan, May 22–26
Parker BD, Ix JH, Cranenburg EC et al (2009) Association of kidney function and uncarboxylated matrix Gla protein: data from the Heart and Soul Study. Nephrol Dial Transplant 24:2095–2101
Cranenburg EC, Brandenburg VM, Vermeer C et al (2009) Uncarboxylated matrix Gla protein (ucMGP) is associated with coronary artery calcification in haemodialysis patients. Thromb Haemost 101:359–366
Hermans MM, Vermeer C, Kooman JP et al (2007) Undercarboxylated matrix GLA protein levels are decreased in dialysis patients and related to parameters of calcium-phosphate metabolism and aortic augmentation index. Blood Purif 25:395–401
Westenfeld R, Krueger T, Schlieper G et al (2012) Effect of vitamin K2 supplementation on functional vitamin K deficiency in hemodialysis patients: a randomized trial. Am J Kidney Dis 59:186–195
Shea MK, O’Donnell CJ, Vermeer C et al (2011) Circulating uncarboxylated matrix gla protein is associated with vitamin K nutritional status, but not coronary artery calcium, in older adults. J Nutr 141:1529–1534
Wajih N, Borras T, Xue W, Hutson SM, Wallin R (2004) Processing and transport of matrix gamma-carboxyglutamic acid protein and bone morphogenetic protein-2 in cultured human vascular smooth muscle cells: evidence for an uptake mechanism for serum fetuin. J Biol Chem 279:43052–43060
Acknowledgments
We thank Prof. Jonattan Fox, MD, Ph.D., for his invaluable editorial help during the preparation of this manuscript.
Funding
This study was funded by Medical University of Silesia in Katowice (Grant Number KNW-1-015/N/3/K).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Wyskida, K., Żak-Gołąb, A., Wajda, J. et al. Functional deficiency of vitamin K in hemodialysis patients in Upper Silesia in Poland. Int Urol Nephrol 48, 765–771 (2016). https://doi.org/10.1007/s11255-016-1255-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-016-1255-6