Abstract
This study was conducted in order to determine the effect of the presence of urinary incontinence on sexual quality of life in women diagnosed with chronic physical diseases. The sample of the cross sectional and comparative study consisted of 67.5 % (n = 191) female inpatients with and 32.5 % (n = 92) female inpatients without urinary incontinence complaints being treated for chronic physical diseases in the internal diseases clinic of a public hospital. Data was collected using the patient identification form, the International Incontinence Consultation Questionnaire-Short Form and the Sexual Quality of Life Scale for Women. The average score that women with urinary incontinence took from the sexual quality of life scale (61.50 ± 19.10) was lower than the average score of women without urinary incontinence (77.19 ± 18.75) (p < 0.01). There was a negative meaningful relationship between the frequency, amount, and effect of urinary incontinence and sexual quality of life (p < 0.05). The sexual quality of life of women who were 50 years of age and above, who had respiratory system diseases, had a duration of illness between 6 and 10 years, perceived their general health as bad, parity and gave normal birth, were in their menopausal period, and had hysterectomies was significantly lower (p < 0.05). As a result, in women with chronic physical diseases and urinary incontinence, the sexual quality of life is affected in a worse level compared to those who do not have urinary incontinence.
Similar content being viewed by others
Introduction
Chronic diseases are long term diseases that can’t be resolved on their own and cause degradation in quality of life because of the symptoms and complications brought about by the disease [1]. Chronic diseases may cause the loss of certain function in patients over time. One of these function losses is urinary incontinence. Urinary incontinence (UI) is involuntary release of urine that can cause social and hygienic problems. UI has several types defined as stress urinary incontinence, that is involuntary loss of urine during sneezing, coughing and exerting effort; urge urinary incontinence, meaning an involuntary loss of urine with a sudden desire to void; mixed urinary incontinence defined as the combination of these two types [2]. UI is a health problem that shows increasing prevalence with increasing age which affects people of all ages. Even though UI is seen 2–3 times more frequently in women compared to men [3, 4], a large number of women are not able to express this problem to healthcare professionals or individuals around them due to stigmatisation or their feelings of shame. For this reason, UI is accepted to be a silent epidemic today [5, 6]. In studies performed in Turkey, the UI prevalence in women in Turkey has been reported to vary between 20.5 and 68.8 % [3].
Even though urinary incontinence is not a situation that threatens the life of a woman, it can cause serious morbidity with concerns such as continuous wetness, irritation, and smell. UI is a medical, social, and economical problem that causes many psychological problems in women including shame and depression, and thus causes a decrease in self confidence, social isolation, and degradations in quality of life [4, 5, 7–12]. Additionally, UI affects the daily home and work activities of women negatively [10, 13]. UI has negative effects on sexual health, which is an important element of quality of life and an inseparable part of human life, aswell [13–20]. In literature, more than half of women with UI are stated to have disorders in their sexual functions [21, 22].
Urinary incontinence disrupts women’s sexual health in various degrees. Psychological pressure, fear of releasing urine during intercourse, and fear of smell have roles in the etiology [19]. In studies, women with UI were found to have sexual dysfunction complaints such as fear of releasing urine during intercourse, decrease in sexual appetite, stimulation disorders, decrease or loss in vaginal sensitivity, decrease in vaginal lubrication, orgasm disorders, and the presence of pain compared to healthy women [12, 23–26]. These problems cause a decrease in proximity and sharing between spouses, negatively affecting marriage relationships [6, 11, 27].
Because of the increasing prevalence of urinary incontinence and its effect on sexual health, the quality of life of women with chronic physical diseases may get even worse [22]. Studies on the prevalence of UI alongside chronic physical diseases [28, 29] and its effects on sexual health are present in literature [10, 11, 14, 16, 18, 19, 26]. However, studies examining the effect of the presence of UI, which can disrupt quality of life by itself, alongside chronic physical diseases on sexual life are insufficient. For this reason, this study was performed in order to determine the effect of UI accompanying chronic physical diseases in women on sexual quality of life and to exhibit the relationships between certain variables and sexual quality of life in women.
Materials and Method
Sample
The universe of this descriptive and cross sectional study consisted of 342 female inpatients being treated for any chronic diseases in the internal diseases, endocrinology, cardiology, neurology, and chest diseases clinics of a public hospital between January 2nd and July 1st 2015. Women over 18 years of age who had been diagnosed with a chronic physical disease for at least 6 months who had no communication problems, had no problems with reading, understanding and answering questions, had the sufficient cognitive level, had no genetic predilection to UI, had no history of urinary system anomalies, diseases or medicine use that may cause UI development who agreed to participate in the study were included in the sample. In this context, 191 women (67.5 %) with UI and 92 women (32.5 %) without UI were included in the study for a total of 283 women.
The average age of the women with chronic diseases was 52.26 ± 12.15 (min: 26, max: 74) years, 70.4 % were married, 33.3 % were primary school graduates, and 73.4 % were housewives. The average duration of illness of the women was 7.55 ± 5.22 (min: 2, max: 24) years, 40.1 % were obese, 37.3 % had cardiovascular system diseases, 25.4 % had diabetes, and 60.4 % were in their menopausal period.
Data Collection Tools
Data was collected using the patient identification form, the International Consultation on Incontinence Questionnaire-Short Form, and the Sexual Quality of Life Scale for Women.
Patient Identification Form
This form consists of 21 questions regarding socio demographic characteristics (age, gender, marital status, education etc.), disease related (name of the disease, illness duration, general health perception) and cases that may cause urinary incontinence (usage of diuretics treatments, number of births, menopause status, presence of hysterectomy etc.).
International Consultation on Incontinence Questionnaire Short Form (ICIQ-SF)
This is a scale used to establish the severity, frequency, and type of urinary incontinence and show to what extent urinary incontinence affects the quality of life of the individual. The ICIQ-SF is a short, easily understood, and easily applied questionnaire regarding urinary incontinence and its effects on quality of life, and its Turkish validity and reliability was performed by Cetinel et al. [30]. The ICIQ-SF contains 6 questions and three of those questions are added together to obtain a score (questions 3, 4, and 5) (minimum 3 and maximum 21). While the 1st and 2nd questions in the ICIQ-SF question age and gender and the 3rd question asks about the frequency of urinary incontinence, the 4th question “How much urine do you think you inadvertently release? (Usage of protective diapers or not)” gives a measure summarized as little, medium, or a lot. The 5th question of the ICIQ-SF questions how much urinary incontinence affects daily life. The 6th question asks when the incontinence events occur. The reliability cronbach alpha coefficient of the scale in this study was found as 0.94.
Sexual Quality of Life Questionnaire-Women (SQLQ)
The scale, which was developed by Symonds et al. [31] and tested for validity and reliability in Turkish by Tugut and Golbasi [32], is applied to women above the age of 18. The scale is a 6 way likert type scale with 18 questions. Each item is expected to be answered by taking into account the sexual life in the last 4 weeks. Each item on the scale is scored between 1 and 6 (1 = I totally agree, 2 = I mostly agree, 3 = I partially agree, 4 = I partially do not agree, 5 = I mostly disagree, 6 = I totally disagree). The range of scores that can be taken from the scale is between 18 and 108. A higher score in the scale shows better sexual quality of life. In our study, the Cronbach alpha reliability coefficient of the scale was found to be 0.93.
Application
In order to protect patient confidentiality, data was collected by the researchers via face to face interviews in a separate room where nobody else was present or in another setting where the researcher could interview the patient alone. Researchers informed the patients on the aim and importance of the study, and women who agreed to participate filled out the patient identification form and the International Consultation on Incontinence Questionnaire via face to face interviews, while the sexual quality of life scale was handed to the women to be filled out alone in order to ensure they were comfortable giving answers. The completion of the study forms by the individuals took approximately 20–25 min on average.
Ethic Approval
Written permission from the ethical board of a university (Decision No: 2014-12/08) was taken before collecting data. Additionally, each woman in the study was verbally informed on the context of the study and voluntary participation, and written permissions from the women were taken. The study was conducted in accordance with the ethical standards of the Helsinki declaration.
Analysis of the Data
Data was interpreted using the SPSS 21.0 package program. The UI and sexual quality of life levels of the women were evaluated using the average test. In the comparison of the descriptive characteristics of women with and without UI, the Chi-squared test was used. The relationship between the presence of UI and the quality of life of the women was evaluated through Pearson correlation analysis. In order to determine the relationship between the descriptive characteristics of the women with UI and sexual quality of life the student t test, one way ANOVA, and the Kruskall Wallis test were used. In statistical evaluation, meaningfulness was evaluated at a level of p < 0.05.
Results
The demographic and disease related characteristics of the women with and without UI were given in Table 1. Accordingly, there were advanced statistically meaningful differences between women with and without UI with regard to age, body mass index (BMI), duration of chronic illness, general health perception, parity, menopause status, presence of hysterectomy, status regarding having urinary tract infection within the past year, and daily amount of liquids consumed (p < 0.01). In this context, the average age of women with incontinence was higher, and most of them were obese, gave more than five births, and menopausal. Additionally, the duration of chronic diseases for these patients were higher and their general health perception was worse. The amount of liquids consumed by women with UI was lower compared to women without.
Among women with chronic diseases and urinary incontinence, 39.5 % stated that they had UI episodes at least once a day, 23.6 % stated they had them once a week or less, and 13.8 % stated they had them continuously. 41.5 % of the women stated they released a small amount while 23.1 % stated they released a lot.
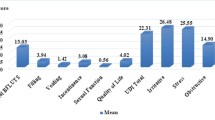
The distribution of the average scores the women with UI took from the ICIQ-SF was given in Table 2. When the average score taken from the test (11.59 ± 5.41) was evaluated, it was seen that UI affects the daily lives of women with chronic diseases on a moderate level with regard to frequency, amount, and effect.
The comparison of the score averages taken by the women with and without UI from the sexual quality of life scale was given in Table 3. Accordingly, the sexual quality of life score average of women with chronic physical diseases was 66.60 ± 20.33, and the score average of women with UI (61.50 ± 19.10) was lower than the score average of women without UI (77.19 ± 18.75) (p < 0.01).
In Table 4, the relationship between the UI status of women and their sexual quality of life was given. According to the correlation analysis performed, there was a negative meaningful relationship between sexual quality of life and the frequency, amount, and effect of UI (p < 0.05; p < 0.01). Thus, as the UI frequency, amount and effect increase, the sexual quality of life of the women is affected negatively.
In Table 5, the relationship between the demographic and disease related characteristics of the women and their sexual quality of life was given. Age, the type and duration of the chronic disease, general health perception, parity, menopause status, and the presence of hysterectomy are the factors that affect sexual life in women (p < 0.05; p < 0.01). Accordingly, women of age 50 and above who have respiratory system diseases, with a duration of illness between 6 and 10 years, who perceive their general health as poor, gave more than five births, gave births through normal means, are menopausal, and underwent hysterectomy all have lower sexual quality of life.
Discussion
The detection of the presence of UI and sexual dysfunction in women may be hard because of social values, norms, shyness, or lack of information [2, 33]. These cases, which affect the daily lives of individuals, may make life even harder when encountered alongside other diseases. For these reasons health professionals should determine the presence of UI and sexual dysfunction in the early period through efficient diagnosis and evaluation, especially in individuals with chronic diseases.
Urinary incontinence is a complex health problem that may arise because of many related factors such as age, gender, weight, the number of pregnancies and births, type of birth given, menopause, hysterectomy, or smoking [10]. Especially in women with chronic diseases, these risk factors may increase the prevalence of UI even more. In this study, 67.5 % of the women with chronic physical diseases were found to have a complaint of UI. Additionally, it was found that women with UI were older, mostly obese or menopausal, and gave more than five births when compared to women without UI, with longer duration of chronic illness. In studies in literature performed for specific diseases, the prevalence of UI and related factors vary. In a study by Hrisanfow and Hagglund [30], the prevalence of UI in women with chronic obstructive lung disease was found to be 49.6 %. In the same study, the BMI values of the women with UI were found to be higher, although there was no difference between average ages [30]. In a study conducted with women with diabetes, the prevalence of UI was found to change between 38 and 44 %,and the presence of UI was found not to be related to age, BMI, status regarding urinary tract infection history, and parity [28]. The fact that the prevalence of UI was found to be higher than the studies in literature may be caused by women with different chronic diseases being included in the study. Additionally, the findings of our study are important with regard to health professionals determining women under risk of UI in the early period.
Turkey has a highly heterogeneous social and cultural structure. Attitudes of women living in rural areas are more conservative and religious. This influences the women’s health behaviours [34] and perspectives about UI. UI is not perceived as a health problem by Turkish women and still remains largely hidden [35]. Whereas, UI affects a woman’s physical and psychological health, family life, and social life from every aspect [4, 5, 9–12]. In our study, UI was found to affect the lives of women with chronic diseases on a medium level with regard to frequency, amount, and effect. Findings in literature also support this finding, showing that the presence of UI in women with various chronic diseases decreases quality of life [3, 4, 11, 36].
Sexual health, which is considered an important and positive dimension of the personal health of individuals from every age group and a supportive factor for healthy aging [2, 17], can be affected by many factors throughout one’s lifetime. One of these factors is categorized as diseases that last for a long time [32]. In literature, sexual dysfunction is stated to be seen more frequently in women with chronic diseases compared to the general population and the healthy group [37, 38]. In our study, the sexual quality of life of women with chronic physical diseases was found to be on an average level that considering the values may be obtained from the total score of the scale. In a study conducted with women with diabetes using the same scale, similar findings were achieved [33]. In a study by Sentosa et al. [39] having chronic diseases was found to affect sexual life negatively. The findings of our study show that the sexual health status of patients should be evaluated alongside their physical health problems.
Urinary incontinence is a strong obstacle for the continuation of a healthy sexual life [15–17]. In our study, the women with UI were found to have worse sexual quality of life compared to women without UI complaints, and it was additionally found that the sexual quality of life is affected negatively as the frequency, amount, and effect of UI increases. In a qualitative study performed with women with spinal cord injuries, the sexual experiences of women were found to be negatively affected by UI and the women were found to experience excessive anxiety regarding urinary release during intercourse [40]. In another qualitative study, most of the women with UI stated that they feel shame during intercourse and thus experience loss of sexual appetite [6]. In another study, the sexual satisfaction of women with UI was found to be 4.7 times less when compared to healthy women, and women were found to try different methods to hide this problem from their spouses and delay intercourse [41]. In a study by Coyne et al. [37] women with UI were found to have intercourse less frequently compared to those without UI (50–91 %), and in a study by Yang et al. [17] a third of women with UI were found to not have intercourse for the past six months. In a study by Nilsson et al. [42] most of the women with UI stated that sexuality was important in their lives, one-third stated they released urine during intercourse half stated they received less satisfaction because of urinary incontinence and worried they would release urine during intercourse, and two-thirds stated that they found themselves anxious and repulsive regarding the subject. In other studies, similar findings were reached [11, 12, 23, 25–27]. The findings of our study suggest that women, beside coping with their chronic diseases, face problems such as UI and sexual life.
In women with chronic diseases developmental life events such as age, pregnancy, birth, lactation, and menopause and disease specific events such as duration of illness, pain, depression, anxiety, fatigue, and the side effects of medicine may cause sexual dysfunction just as well as UI [24, 32, 38]. In our study, the sexual quality of life of women above age 50 who gave more than five births, who gave normal birth, who were menopausal and had UI was found to be lower. In a study by Yang et al. [17] when women with active and inactive sexual lives with UI were compared, those with inactive sexual lives were found to be older, mostly postmenopausal, and have given more births. In the same study, BMI and manner of parity were found to not affect the sexual functions of women with UI [17]. In another study, it was found that the sexual dysfunction complaints of women increase with age, and that having chronic diseases, giving many births, and being menopausal affected sexual health negatively [24]. In a study conducted with middle aged adults using a similar scale, the sexual quality of life of those who were 56 and above and those who had any disease was found to be lower [43]. The findings of our study are important with regard to exhibiting the factors disrupting sexual quality of life in women with UI. In this context, it is an inevitable conclusion that efficient counseling services should be provided to women in risk groups in order to protect and improve the health of women.
Limitations of the Study
Since the study was conducted in a single hospital with inpatients who fulfilled the inclusion criteria, it has a sample and time limitation. Additionally, the self reports of the patients regarding UI and sexual quality of life are limited to the ICIQ-SF and SQLQ. In future studies, sexual quality of life should be evaluated with a wider sample and prevention interventions for the loss of sexual quality of life should be applied and tested.
Conclusion
The results of our study show that the sexual quality of life of women with chronic physical diseases and urinary incontinence is affected negatively. Additionally, sexual quality of life gets even worse as the frequency, amount, and effect of UI increases. Alongside factors that can’t be controlled such as age and menopause status, controllable factors such as the type of the chronic disease, duration of illness, parity affect quality of life in women with UI on an important level.
In this context, health professionals should certainly consider UI a health problem, and evaluate women with chronic physical diseases for UI risk factors (parity, menopause status etc.) regardless of their life stage. Additionally, health professionals should question the presence of UI and effect of UI on sexual health when taking patient history, provide services to women in the context of a holistic care approach, take an active role in providing counseling services on the topics of UI protection and treatment, disease management, and continuation of a healthy sexual life, and contribute to the betterment of sexual quality of life by helping resolve the determined issues. Awareness being raised on UI and healthy sexual life in women through health education programs given both through media and the institution can be effective in determining women who have problems on the issue in the early period, protecting women’s health.
References
Kumsar, A.K., Yilmaz, F.T.: Overview of quality of life in chronic disease patients. Erciyes Univ. Fac. Health Sci. J. 2(2), 62–70 (2014)
Ozkan, S., Ogce, F., Cakır, D.: Quality of life and sexual function of women with urinary incontinence. Jpn. J. Nurs. Sci. 8, 11–19 (2011)
Sensoy, N., Dogan, N., Ozek, B., Karaaslan, L.: Urinary incontinence in women: prevalence rates, risk factors and impact on quality of life. Pak. J. Med. Sci. 29(3), 818–822 (2013)
Szymona-Pałkowska, K., Kraczkowski, J.J., Janowski, K., Steuden, S., Adamczuk, J., Robak, J.M., Bakalczuk, S., Bakalczuk, G.: Selected determinants of quality of life in women with urinary incontinence. Prz Menopauzalny 13(2), 84–88 (2014)
Yip, S.K., Cardozo, L.: Psychological morbidity and female urinary incontinence. Best Pract. Res. Clin. Obstet. Gynaecol. 21, 321–329 (2007)
Akyuz, A., Kok, G., Kilic, A., Guvenc, G.: In her own words: living with urinary incontinence in sexual life. Sex. Disabil. 32, 23–33 (2014)
Sen, I., Onaran, M., Aksakal, N., Acar, C., Tan, M.O., Acar, A., et al.: The impact of urinary incontinence on female sexual function. Adv. Ther. 23, 999–1008 (2006)
Alan, C., Koçoğlu, H., Ersay, A.R., Alan, H., Ertung, Y., Kurt, H.A.: Effects of stress type urinary incontinence on sexual function, social status and quality of life. N. J. Urol. 5(3), 123–131 (2009)
Hägglund, D., Ahlström, G.: The meaning of women’s experience of living with long-term urinary incontinence is powerlessness. J. Clin. Nurs. 16(10), 1946–1954 (2007)
Topuz, Ş.: Urinary continence and sexuality. Balikesir Health Sci. J. 4(1), 60–64 (2015)
Oh, S.J., Ku, J.H., Choo, M.S., Yun, J.M., Kim, D.Y., Park, W.H.: Health-related quality of life and sexual function in women with stress urinary incontinence and over active bladder. Int. J. Urol. 15, 62–67 (2008)
Liebergall-Wischnitzer, M., Paltiel, O., Hochner-Celnikier, D., Lavy, Y., Manor, O., Wruble, A.C.W.: Sexual function and quality of life for women with mild-to-moderate stress urinary incontinence. J. Midwifery Women’s Health 56(5), 461–467 (2011)
Sinclair, A.J., Ramsay, I.N.: The psychosocial impact of urinary incontinence in women. Obstet. Gynaecol. 13, 143–148 (2011)
LeCroy, C.: Urinary incontinence occurring during intercourse: effect on sexual function in women. Urol. Nurs. 26(1), 53–56 (2006)
Jha, S., Strelley, K., Radley, S.: Incontinence during intercourse: myths unravelled. Int. Urogynecol. J. 23(5), 633–637 (2012)
Serati, M., Salvatore, S., Uccella, S., Nappi, R.E., Bolis, P.: Female urinary incontinence during intercourse: a review on an under studied problem for women’s sexuality. J. Sex. Med. 6, 40–48 (2009)
Yang, S.H., Yang, J.M., Wang, K.H., Huang, W.C.: Biologic correlates of sexual function in women with stress urinary incontinence. J. Sex. Med. 5(12), 2871–2879 (2008)
Faira, K., Pedrosa, L.A.K.: Quality of life and sexual function in women with and without urinary incontinence: an evaluation. Rev. Eletr. Enf. 14(2), 366–373 (2012)
Aslan, G., Köseoğlu, H., Sadik, O., Gimen, S., Cihan, A., Esen, A.: Sexual function in women with urinary incontinence. Int. J. Impot. Res. 17(3), 248–251 (2005)
Farage, M.A., Miller, K.W., Berardesca, E., Maibach, H.I.: Psychosocial and societal burden of incontinence in the aged population: a review. Arch. Gynecol. Obstet. 277(4), 285–290 (2008)
Dalpiaz, O., Kerschbaumer, A., Mitterberger, M., Pinggera, G.M., Colleselli, D., Bartsch, G., Strasser, H.: Female sexual dysfunction: a new urogynaecological research field. BJU Int. 101(6), 717–721 (2008)
Salman, M.Y., Fazlıoğlu, A.: The affects of urinary incontinence, over active bladder and bladder pain syndrome on female sexual dysfunctions. Turk. Klinikleri J. Urol. Spec. Top. 8(3), 45–51 (2015)
Salonia, A., Zanni, G., Nappi, R.E., Briganti, A., Dehò, F., Fabbri, F., Colombo, R., Guazzoni, G., DiGirolamo, V., Rigatti, P., Montorsi, F.: Sexual dysfunction is common in women with lower urinary tract symptoms and urinary incontinence: results of a cross-sectional study. Eur. Urol. 45(5), 642–648 (2004)
Cayan, S., Akbay, E., Bozlu, M., et al.: The prevalence of female sexual dysfunction and potential risk factors that may impair sexual functionin Turkish women. Urol. Int. 72, 52–57 (2004)
Handa, V.L., Harvey, L., Cundiff, G.W., Siddique, S.A., Kjerulff, K.H.: Sexual function among women with urinary incontinence and pelvic organ prolapse. Am. J. Obstet. Gynaecol. 191, 751–756 (2004)
Dean, N., Wilson, D., Herbison, P., Glazener, C., Aung, T., Macarthur, C.: Sexual function, delivery mode history, pelvic floor muscle exercises and incontinence: a cross-sectional study six years post-partum. Aust. N. Z. J. Obstet. Gynaecol. 48, 302–311 (2008)
Bekker, M.D., Beck, J.J.H., Putter, H., Van Driel, M.F., Pelger, R.C.M., Weijmar Schultz, W.C., Lycklama à Nijeholt, G.A.B., Elzevier, H.W.: Sexual experiences of men with incontinent partners. J. Sex. Med. 7, 1877–1882 (2010)
Bani-Issa, W., Almomani, F., Eldeirawi, K.: Urinary incontinence among adult women with diabetes in Jordan: epidemiology, correlates and perceived impact on emotional and social well-being. J. Clin. Nurs. 23(17–18), 2451–2460 (2014)
Hrisanfow, E., Hagglund, D.: The prevalence of urinary incontinence among women and men with chronic obstructive pulmonary disease in Sweden. J. Clin. Nurs. 20, 1895–1905 (2011)
Çetinel, B., Özkan, B., Can, G.: The validation study of ICIQ-SF Turkish version. Turk. J. Urol. 30(3), 332–338 (2004)
Symonds, T., Boolell, M., Quırk, F.: Development of questionnaire on sexual quality of life in women. J. Sex Marital Ther. 31, 385–397 (2005)
Tuğut, N., Gölbaşı, Z.: A validity and reliability study of Turkish version of the Sexual Quality of Life Questionnaire-Female. Cumhur. Med. J. 32, 172–180 (2010)
Celik, S., Golbası, Z., Kelleci, M., Satman, I.: Sexual dysfunction and sexual quality of life in women with diabetes: the study based on a diabetic center. Sex. Disabil. 33, 233–241 (2015)
Bahar, Z., Beser, A., Ozbicakci, S., Haney, M.O.: Health promotion behaviours of Turkish women. Dokuz Eylul Univ. Sch. Nurs. Electron. J. 6, 9–16 (2013)
Beji, N.K., Ozbas, A., Aslan, E., Bilgic, D., Erkan, H.A.: Overview of the social impact of urinary incontinence with a focus on Turkish women. Urol. Nurs. 30, 327–334 (2010)
Riss, P., Kargl, J.: Quality of life and urinary incontinence in women. Maturitas 68, 137–142 (2011)
Coyne, K.S., Sexton, C.C., Irwin, D.E., Kopp, Z.S., Kelleher, C.J., Milsom, I.: The impact of over active bladder, incontinence and other lower urinary tract symptoms on quality of life, work productivity, sexuality and emotional well-being in men and women: results from the EPIC study. BJU Int. 101, 1388–1395 (2008)
Cardeau, D., Courtois, F.: Sexual disorders in women with MS: assessment and management. Ann. Phys. Rehabil. Med. 57, 337–347 (2014)
Santosa, A., Őhman, A., Högberg, U., Stenlund, H., Hakimi, M., Ng, N.: Cross-sectional survey of sexual dysfunction and quality of life among older people in Indonesia. J. Sex. Med. 8, 1594–1602 (2011)
Cramp, J., Courtois, F., Connolly, M., Cosby, J., Ditor, D.: The impact of urinary incontinence on sexual function and sexual satisfaction in women with spinal cord injury. Sex. Disabil. 32, 397–412 (2014)
Kizilkaya Beji, N., Yalçın, O., Ayyıldız, E.H., Kayir, A.: Effect of urinary leakage on sexual function during sexual intercourse. Urol. Int. 74(3), 250–255 (2005)
Nilsson, M., Lalos, O., Lindkvist, H., Lalos, A.: How do urinary incontinence and urgency affect women’s sexual life? Acta Obstet. Gynecol. Scand. 90(6), 621–628 (2011)
Kim, J.S., Kang, S.A.: Study on body image, sexual quality of life, depression, and qualityof life in middle-aged adults. Asian Nurs. Res. (Korean Soc. Nurs. Sci.). 9(2), 96–103 (2015)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Taskin Yilmaz, F., Karakoc Kumsar, A., Demirel, G. et al. The Effect of Urinary Incontinence on Sexual Quality of Life in Women with Chronic Physical Diseases. Sex Disabil 34, 403–415 (2016). https://doi.org/10.1007/s11195-016-9457-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11195-016-9457-5