Abstract
Background
Sleep apnea (SA) is a prevalent chronic disease with significant morbidity that negatively impacts a patient’s perception of health and quality of life (QoL).
Objective
This review synthesized qualitative evidence on the experiences of patients living with SA to understand the disease’s impacts on QoL.
Methods
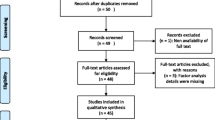
We performed a systematic review of qualitative studies and searched eight electronic databases from inception dates to 22 September 2020. We analyzed the data using Sandelowski’s proposed method of meta-synthesis, and applied Critical Appraisal Skills Program (CASP) and GRADE-Confidence in the Evidence from Reviews of Qualitative research (GRADE-CERQual) criteria to appraise the studies’ qualities, and synthesized findings, respectively.
Results
Fourteen qualitative studies met the selection criteria. Four themes and 16 subthemes emerged: (1) sleep-related manifestations (n = 14) with four subthemes (sleep disruptors; sleepiness & napping; fatigue & low energy level; decreased cognition), (2) reduced psychological well-being and functioning (n = 14) with seven subthemes (anxiety & feeling vulnerable; hostility; sadness, sense of hopelessness & depression; embarrassment, shame & diminished self-concept; guilt & self-blame; maladaptive coping; self-stigma, (3) impaired physical and role functioning (n = 13) with three subthemes (reduced activities & routine disruption; reduced sexual activities & desire; reduced job performance & participation), (4) impaired social and relational functioning (n = 13) with two subthemes (strained interpersonal relationships; social isolation & loneliness).
Conclusions
SA patients experienced sleep-disrupting symptoms and daytime sleepiness/fatigue which adversely impacted physical, psycho-cognitive, and social aspects of their lives in complex interactive ways. This understanding can help facilitate patient-centric care and develop comprehensive patient-reported measures to effect good health outcomes.


Similar content being viewed by others
Data availability statement
Supporting data can be found in the electronic supplementary materials (ESM) available at https://doi.org/10.1007/s1136-022-03332-7.
References
Institute of Medicine (US) Committee on Quality of Health Care in America. (2001). Crossing the quality chasm: a new health system for the 21st century. National Academies Press.
Rathert, C., Wyrwich, M. D., & Boren, S. A. (2013). Patient-centered care and outcomes: A systematic review of the literature. Medical Care Research and Review, 70(4), 351–379.
National Quality Forum. (2013). Patient-reported outcomes (PROs) in performance measurement [cited 2021 July 21]. Retrieved from: www.qualityforum.org/Projects/n-r/Patient-Reported_Outcomes/Patient-Reported_Outcomes.aspx
Patrick, D. L., Burke, L. B., Gwaltney, C. J., Leidy, N. K., Martin, M. L., Molsen, E., & Ring, L. (2011). Content validity–establishing and reporting the evidence in newly developed patient-reported outcomes (PRO) instruments for medical product evaluation: ISPOR PRO good research practices task force report: Part 1–eliciting concepts for a new PRO instrument. Value Health, 14(8), 967–977.
Peasgood, T., Mukuria, C., Carlton, J., Connell, J., & Brazier, J. (2021). Criteria for item selection for a preference-based measure for use in economic evaluation. Quality of Life Research, 30(5), 1425–1432.
Boehnke, J. R., & Rutherford, C. (2021). Using feedback tools to enhance the quality and experience of care. Quality of Life Research, 30(11), 3007–3013.
U.S. Food and Drug Administration. (2009). Guidance for industry—patient-reported outcome measures: Use in medical product development to support labeling claims. U.S. Food and Drug Administration [cited 2022 May 1]. Retrieved from: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/patient-reported-outcome-measures-use-medical-product-development-support-labeling-claims.
Reeve, B. B., Wyrwich, K. W., Wu, A. W., Velikova, G., Terwee, C. B., Snyder, C. F., et al. (2013). ISOQOL recommends minimum standards for patient-reported outcome measures used in patient-centered outcomes and comparative effectiveness research. Quality of Life Research, 22(8), 1889–1905.
Garvey, J. F., Pengo, M. F., Drakatos, P., & Kent, B. D. (2015). Epidemiological aspects of obstructive sleep apnea. Journal of Thoracic Disease, 7(5), 920–929.
Bradley, T. D., & Floras, J. S. (2009). Obstructive sleep apnoea and its cardiovascular consequences. Lancet, 373(9657), 82–93.
Benjafield, A. V., Ayas, N. T., Eastwood, P. R., Heinzer, R., Ip, M. S., Morrell, M. J., Nunez, C. M., Patel, S. R., Penzel, T., Pépin, J. L., & Peppard, P. E. (2019). Estimation of the global prevalence and burden of obstructive sleep apnoea: A literature-based analysis. Lancet Respiratory Medicine, 7(8), 687–98.
Pauletto, P., Réus, J. C., Bolan, M., Massignan, C., Flores-Mir, C., Maia, I., Gozal, D., Hallal, A. L., Porporatti, A. L., & Canto, G. D. (2021). Association between obstructive sleep apnea and health-related quality of life in untreated adults: A systematic review. Sleep Breath. https://doi.org/10.1007/s11325-021-02323-1
Silva, F. S. L., Bezerra, J., Mota, B. C., de Oliveira, A. C. S., Sobreira-Neto, M. A., de Castro, S. S., & Leite, C. F. (2020). Are the International Classification of Functioning, Disability and Health (ICF) domains considered in the obstructive sleep apnea instruments? An integrative review. Sleep Breath. https://doi.org/10.1007/s11325-020-02173-3
Chafe, R. (2017). The Value of qualitative description in health services and policy research. Healthcare Policy, 12(3), 12–18.
Cheng, K. K. F., & Clark, A. M. (2017). Qualitative methods and patient-reported outcomes: Measures development and adaptation. International Journal of Qualitative Methods, 16(1), 1609406917702983.
Tetzlaff, J., Page, M., & Moher, D. (2020). PNS154 The Prisma 2020 Statement: Development of and key changes in an updated guideline for reporting systematic reviews and meta-analyses. Value in Health, 23, S312–S313.
Sandelowski, M., Barroso, J., & Voils, C. I. (2007). Using qualitative metasummary to synthesize qualitative and quantitative descriptive findings. Research in Nursing & Health, 30(1), 99–111.
World Health Organization. (2021). What is the WHO definition of health? [cited 2021 May 16]. Retrieved from https://www.who.int/about/who-we-are/frequently-asked-questions
Atkins, S., Lewin, S., Smith, H., Engel, M., Fretheim, A., & Volmink, J. (2008). Conducting a meta-ethnography of qualitative literature: Lessons learnt. BMC Medical Research Methodology, 8, 21.
Newton, B. J., Rothlingova, Z., Gutteridge, R., LeMarchand, K., & Raphael, J. H. (2012). No room for reflexivity? Critical reflections following a systematic review of qualitative research. Journal of Health Psychology, 17(6), 866–885.
CASP.(2018). CASP Qualitative Studies Checklist: Critical Appraisal Skills Programme [cited 2020 October 28]. Retrieved from https://casp-uk.net/wp-content/uploads/2018/01/CASP-Qualitative-Checklist-2018.pdf
Lewin, S., Booth, A., Glenton, C., Munthe-Kaas, H., Rashidian, A., Wainwright, M., Bohren, M. A., Tunçalp, Ö., Colvin, C. J., Garside, R., & Carlsen, B. (2018). Applying GRADE-CERQual to qualitative evidence synthesis findings: Introduction to the series. Implement Science, 13(Suppl 1), 2.
Schünemann, H., Brozek, J., Guyatt, G., Oxman, A. (Eds.). (updated October 2013). Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach: GRADE Working Group. Retrieved from gdt.guidelinedevelopment.org/app/handbook/handbook.html
Higgins, JP., Altman, D., Sterne, JA. (Eds). (updated June 2017). Chapter 8: Assessing risk of bias in included studies. 2017. Cochrane Handbook for Systematic Reviews of Interventions version 520 [Internet]. Cochrane, 2017. Retrieved from www.training.cochrane.org/handbook
Lewin, S., Bohren, M., Rashidian, A., Munthe-Kaas, H., Glenton, C., Colvin, C. J., Garside, R., Noyes, J., Booth, A., Tunçalp, Ö., & Wainwright, M. (2018). Applying GRADE-CERQual to qualitative evidence synthesis findings-paper 2: How to make an overall CERQual assessment of confidence and create a Summary of Qualitative Findings table. Implement Sci., 13(Suppl 1), 10.
Broström, A., Johansson, P., Ass, A. S., Albers, J., Mårtensson, J., & Svanborgb, E. (2006). 1324: Signs and consequences of obstructive sleep apnea before treatment initiation. European Journal of Cardiovascular Nursing, 5, 15.
Chu, G., Price, E., Paech, G. M., Choi, P., & McDonald, V. M. (2020). Sleep apnea in maintenance hemodialysis: A mixed-methods study. Kidney Medicine, 2(4), 388–97.
Gullvåg, M., Gjeilo, K. H., Fålun, N., Norekvål, T. M., Mo, R., & Broström, A. (2019). Sleepless nights and sleepy days: a qualitative study exploring the experiences of patients with chronic heart failure and newly verified sleep-disordered breathing. Scandinavian Journal of Caring Sciences, 33(3), 750–9.
Lee, C. H., Lin, M. H., Chen, N. H., Ho, L. H., Lee, H. F., & Tsao, L. I. (2015). The experiences of obstructive sleep apnea in women. Hu li za zhi The journal of nursing, 62(6), 48–56.
Menard KJ. (2015). Experience of Women with a Diagnosis of Obstructive Sleep Apnea (OSA): A Dissertation. (Graduate School of Nursing Dissertations). https://doi.org/10.13028/721d-2s16 [cited 2021 January 16]. Retrieved from https://escholarship.umassmed.edu/gsn_diss/36.
O’Donoghue, N.-M., & Elizabeth, A. (2012). Exploring the impact of sleep apnoea on daily life and occupational engagement. British Journal of Occupational Therapy, 75(11), 509–516.
Reishtein, J. L., Pack, A. I., Maislin, G., Dinges, D. F., Bloxham, T. J., George, C. F., Greenberg, H., Kader, G. A., Mahowald, M. W., Younger, J. B., & Weaver, T. E. (2006). Sleepiness and relationships in obstructive sleep apnea. Issues in Mental Health Nursing, 27(3), 319–30.
Rodgers, B. (2014). Breaking through limbo: Experiences of adults living with obstructive sleep apnea. Behavioral Sleep Medicine, 12(3), 183–197.
Rudolph, M. A., Rotsides, J. M., & Zapanta, P. E. (2018). The patient’s perioperative perspective during the treatment of obstructive sleep apnea: A pilot study. Sleep and Breathing, 22(4), 997–1003.
Sawyer, AM. (2007). Adult perceptions of the diagnosis and treatment of obstructive sleep apnea: Sociocultural and ethnic influences on adherence outcomes. University of Pennsylvania.
Tandeter, H., Hershkovitz, Y., & Kacen, L. (2016). A single qualitative study can show same findings as years of quantitative research: Obstructive sleep apnoea as an example. Australasian Medical Journal, 9(6), 176–84.
Veale, D., Poussin, G., Benes, F., Pepin, J. L., & Levy, P. (2002). Identification of quality of life concerns of patients with obstructive sleep apnoea at the time of initiation of continuous positive airway pressure: A discourse analysis. Quality of Life Research, 11(4), 389–99.
Waldman, L. T., Parthasarathy, S., Villa, K. F., Bron, M., Bujanover, S., & Brod, M. (2020). Understanding the burden of illness of excessive daytime sleepiness associated with obstructive sleep apnea: A qualitative study. Health and Quality of Life Outcomes, 18(1), 1.
Zarhin, D. (2014). Obstructive sleep apnea as a patient contested disease: Pathways to and away from medicalization. Dissertation Abstracts International Section A: Humanities and Social Sciences. 75(1-A(E)), No-Specified.
Wilson, I. B., & Cleary, P. D. (1995). Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. Jama, 273(1), 59–65.
Swinburn, P., Lloyd, A., Boye, K. S., Edson-Heredia, E., Bowman, L., & Janssen, B. (2013). Development of a disease-specific version of the EQ-5D-5L for use in patients suffering from psoriasis: Lessons learned from a feasibility study in the UK. Value Health, 16(8), 1156–1162.
Flemons, W. W., & Tsai, W. (1997). Quality of life consequences of sleep-disordered breathing. The Journal of Allergy and Clinical Immunology, 99(2), S750–S756.
Moyer, C. A., Sonnad, S. S., Garetz, S. L., Helman, J. I., & Chervin, R. D. (2001). Quality of life in obstructive sleep apnea: A systematic review of the literature. Sleep Medicine, 2(6), 477–491.
Engleman, H. M., & Douglas, N. J. (2004). Sleep 4: Sleepiness, cognitive function, and quality of life in obstructive sleep apnoea/hypopnoea syndrome. Thorax, 59(7), 618–622.
Ware, J. E., Jr., & Sherbourne, C. D. (1992). The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care, 30(6), 473–483.
Brooks, R. (1996). EuroQol: The current state of play. Health Policy, 37(1), 53–72.
World Health Organization. (2021). WHOQOL: Measuring Quality of Life [cited 2021 December 21]. Available in https://www.who.int/tools/whoqol
Mezzich, J. E., Cohen, N. L., Ruiperez, M. A., Banzato, C. E., & Zapata-Vega, M. I. (2011). The multicultural quality of life index: Presentation and validation. Journal of Evaluation in Clinical Practice, 17(2), 357–364.
Abma, I. L., van der Wees, P. J., Veer, V., Westert, G. P., & Rovers, M. (2016). Measurement properties of patient-reported outcome measures (PROMs) in adults with obstructive sleep apnea (OSA): A systematic review. Sleep Medicine Reviews, 28, 18–31.
Johns, M. W. (1991). A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep, 14(6), 540–545.
Van Knippenberg, F. C., Passchier, J., Heysteck, D., Shackleton, D., Schmitz, P., Poublon, R. M., & Van der Meche, F. (1995). The Rotterdam Daytime Sleepiness Scale: A new daytime sleepiness scale. Psychological Reports, 76(1), 83–7.
Gliklich, R. E., & Wang, P. C. (2002). Validation of the snore outcomes survey for patients with sleep-disordered breathing. Archives of Otolaryngology—Head and Neck Surgery, 128(7), 819–824.
Dolan, D. C., Taylor, D. J., Okonkwo, R., Becker, P. M., Jamieson, A. O., Schmidt-Nowara, W., & Rosenthal, L. D. (2009). The time of day sleepiness scale to assess differential levels of sleepiness across the day. Journal of Psychosomatic Research, 67(2), 127–133.
Sangal, R. B. (2012). Evaluating sleepiness-related daytime function by querying wakefulness inability and fatigue: Sleepiness-Wakefulness Inability and Fatigue Test (SWIFT). Journal of Clinical Sleep Medicine, 8(6), 701–711.
Weaver, T. E., Laizner, A. M., Evans, L. K., Maislin, G., Chugh, D. K., Lyon, K., Smith, P. L., Schwartz, A. R., Redline, S., Pack, A. I., & Dinges, D. E. (1997). An instrument to measure functional status outcomes for disorders of excessive sleepiness. Sleep, 20(10), 835–43.
Flemons, W. W., & Reimer, M. A. (1998). Development of a disease-specific health-related quality of life questionnaire for sleep apnea. American Journal of Respiratory and Critical Care Medicine, 158(2), 494–503.
Piccirillo, J. F., Gates, G. A., White, D. L., & Schectman, K. B. (1998). Obstructive sleep apnea treatment outcomes pilot study. Otolaryngology-Head and Neck Surgery, 118(6), 833–844.
Lacasse, Y., Bureau, M. P., & Sériès, F. (2004). A new standardised and self-administered quality of life questionnaire specific to obstructive sleep apnoea. Thorax, 59(6), 494.
Moroni, L., Neri, M., Lucioni, A. M., Filipponi, L., & Bertolotti, G. (2011). A new means of assessing the quality of life of patients with obstructive sleep apnea: The MOSAS questionnaire. Sleep Medicine, 12(10), 959–965.
Abma, I. L., Rovers, M., Ijff, M., Hol, B., Westert, G. P., & van der Wees, P. J. (2017). The development of a patient-reported outcome measure for patients with obstructive sleep apnea: The Patient-Reported Apnea Questionnaire (PRAQ). Journal of Patient-Reported Outcomes, 1(1), 14.
Castellanos Caro, G. L., Matiz Ibarra, T. L., Bastidas Goyes, A. R., Bazurto, M. A., & García Manrique, J. G. (2018). Calidad de vida con el síndrome de apnea-hipoapnea del sueño. Universitas Medica, 59, 11–16.
Engel, G. L. (1977). The need for a new medical model: A challenge for biomedicine. Science, 196(4286), 129–136.
Ojelabi, A. O., Graham, Y., Haighton, C., & Ling, J. (2017). A systematic review of the application of Wilson and Cleary health-related quality of life model in chronic diseases. Health and Quality of Life Outcomes, 15(1), 241.
American Academy of Sleep Medicine. (2014). International Classification of Sleep Disorders (3rd ed.). Darien, IL: American Academy of Sleep Medicine.
Chotinaiwattarakul, W., O’Brien, L. M., Fan, L., & Chervin, R. D. (2009). Fatigue, tiredness, and lack of energy improve with treatment for OSA. Journal of Clinical Sleep Medicine, 5(3), 222–227.
Hossain, J. L., Ahmad, P., Reinish, L. W., Kayumov, L., Hossain, N. K., & Shapiro, C. M. (2005). Subjective fatigue and subjective sleepiness: Two independent consequences of sleep disorders? Journal of Sleep Research, 14(3), 245–253.
Acknowledgements
The team would like to acknowledge Ms. Annelissa Chin Mien Chew, a senior librarian from National University Singapore for her advice and guidance in coming up with the search strategy.
Funding
No funding was required for this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study. A-PC & NL conceptualized the study. A-PC, SS & NL designed the study. All authors contributed to data collection and analysis at various stages of the investigation. The first draft of the manuscript was written by, and all tables and figures were prepared by A-PC. Reviewing and editing were performed by A-PC, SS and NL. ZYS proofread the final manuscript. The work was supervised by NL. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest.
Ethical approval
No ethics approval was required for this study.
Consent for publication
All authors consent to publication if the manuscript is accepted.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chua, AP., Soh, Z.Y., Rahman, S.A. et al. Lived experience of patients with sleep apnea: a systematic synthesis of qualitative evidence. Qual Life Res 32, 1447–1467 (2023). https://doi.org/10.1007/s11136-022-03332-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-022-03332-7