Abstract
Purpose
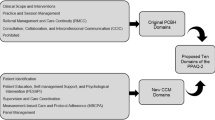
Healthcare engagement is a core measurement target for efforts to improve healthcare systems. This construct is broadly defined as the extent to which healthcare services represent collaborative partnerships with patients. Previous qualitative work operationalized healthcare engagement as generalized self-efficacy in four related subdomains: self-management, collaborative communication, health information use, and healthcare navigation. Building on this work, our objective was to establish a healthcare engagement instrument that is sufficiently unidimensional to yield a single score.
Method
We conducted cognitive interviews followed by a nation-wide mail survey of US Veteran Administration (VA) healthcare users. Data were collected on 49 candidate healthcare engagement items, as well as measures of self-efficacy for managing symptoms, provider communication, and perceived access. Items were subjected to exploratory bifactor, statistical learning, and IRT analyses.
Results
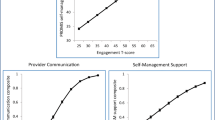
Cognitive interviews were completed by 56 patients and 9552 VA healthcare users with chronic conditions completed the mail survey. Participants were mostly white and male but with sizable minority participation. Psychometric analyses and content considerations reduced the item pool to 23 items, which demonstrated a strong general factor (OmegaH of .89). IRT analyses revealed a high level of reliability across the trait range and little DIF across groups. Most health information use items were removed during analyses, suggesting a more independent role for this domain.
Conclusion
We provide quantitative evidence for a relatively unidimensional measure of healthcare engagement. Despite developed with VA healthcare users, the measure is intended for general use. Future work includes short-form development and validation with other patient groups.



Similar content being viewed by others
Data availability
Data will be made available in accordance with the data management plan submitted to the VA Office of Research and Development. Within one year of publication of manuscripts addressing the aims of the grant, investigators will make a deidentified, anonymized dataset available to the public.
Code availability
Code for the analyses presented in this paper will be made available upon request.
References
Blumenthal, D., & McGinnis, J. M. (2015). Measuring vital signs: An IOM report on core metrics for health and health care progress. JAMA, 313(19), 1901–1902. https://doi.org/10.1001/jama.2015.4862.
Carman, K. L., Dardess, P., Maurer, M., Sofaer, S., Adams, K., Bechtel, C., & Sweeney, J. (2013). Patient and family engagement: A framework for understanding the elements and developing interventions and policies. Health Affairs (Millwood), 32(2), 223–231. https://doi.org/10.1377/hlthaff.2012.1133.
Frampton, S. B., Guastello, S., Hoy, L., Naylor, M., Sheridan, S., & Johnston-Fleece, M. (2017). Harnessing evidence and experience to change culture: A guiding framework for patient and family engaged care. NAM Perspectives, 7(1), 1–37. https://doi.org/10.31478/201701f.
Berwick, D. M., Nolan, T. W., & Whittington, J. (2008). The triple aim: Care, health, and cost. Health Affairs (Millwood), 27(3), 759–769. https://doi.org/10.1377/hlthaff.27.3.759.
Castellon-Lopez, Y., Skrine Jeffers, K., Duru, O. K., Moreno, G., Moin, T., Grotts, J., et al. (2020). Psychometric properties of the altarum consumer engagement (ACE) measure of activation in patients with prediabetes. Journal of General Internal Medicine, 35(11), 3159–3165. https://doi.org/10.1007/s11606-020-05727-z.
Graffigna, G., Barello, S., Bonanomi, A., & Lozza, E. (2015). Measuring patient engagement: Development and psychometric properties of the Patient Health Engagement (PHE) Scale. Frontiers in Psychology. https://doi.org/10.3389/fpsyg.2015.00274.
Wasson, J. H., & Coleman, E. A. (2014). Health confidence: An essential measure for patient engagement and better practice. Family Practice Management, 21(5), 8–12.
Gruman, J., Rovner, M. H., French, M. E., Jeffress, D., Sofaer, S., Shaller, D., & Prager, D. J. (2010). From patient education to patient engagement: Implications for the field of patient education. Patient Education and Counseling, 78(3), 350–356. https://doi.org/10.1016/j.pec.2010.02.002.
Tzeng, H. M., & Marcus Pierson, J. (2017). Measuring patient engagement: Which healthcare engagement behaviours are important to patients? Journal of Advanced Nursing, 73(7), 1604–1609. https://doi.org/10.1111/jan.13257.
Powell, R. E., Doty, A., Casten, R. J., Rovner, B. W., & Rising, K. L. (2016). A qualitative analysis of interprofessional healthcare team members’ perceptions of patient barriers to healthcare engagement. BMC Health Services Research. https://doi.org/10.1186/s12913-016-1751-5.
Tai-Seale, M., Sullivan, G., Cheney, A., Thomas, K., & Frosch, D. L. (2016). The language of engagement: “Aha!” moments from engaging patients and community partners in two pilot projects of the patient-centered outcomes research institute. The Permanente Journal, 20(2), 89–92. https://doi.org/10.7812/TPP/15-123.
Grant, R. W., Altschuler, A., Uratsu, C. S., Sanchez, G., Schmittdiel, J. A., Adams, A. S., & Heisler, M. (2017). Primary care visit preparation and communication for patients with poorly controlled diabetes: A qualitative study of patients and physicians. Primary Care Diabetes, 11(2), 148–153. https://doi.org/10.1016/j.pcd.2016.11.003.
Austin, E. J., Lee, J. R., Bergstedt, B., Mitchell, A. I., Javid, S. H., Ko, C. W., & Gore, J. L. (2020). “Help me figure this out”: Qualitative explorations of patient experiences with cancer pathology reports. Patient Education and Counseling. https://doi.org/10.1016/j.pec.2020.07.020.
Smith, S. K., Dixon, A., Trevena, L., Nutbeam, D., & McCaffery, K. J. (2009). Exploring patient involvement in healthcare decision making across different education and functional health literacy groups. Social Science and Medicine, 69(12), 1805–1812. https://doi.org/10.1016/j.socscimed.2009.09.056.
Bokhour, B. G., Cohn, E. S., Cortes, D. E., Solomon, J. L., Fix, G. M., Elwy, A. R., et al. (2012). The role of patients’ explanatory models and daily-lived experience in hypertension self-management. Journal of General Internal Medicine, 27(12), 1626–1634. https://doi.org/10.1007/s11606-012-2141-2.
Kimerling, R., Lewis, E. T., Javier, S. J., & Zulman, D. M. (2019). Opportunity or burden? A behavioral framework for patient engagement. Medical Care. https://doi.org/10.1097/MLR.0000000000001240.
Bombard, Y., Baker, G. R., Orlando, E., Fancott, C., Bhatia, P., Casalino, S., et al. (2018). Engaging patients to improve quality of care: A systematic review. Implementation Science, 13(1), 1–22. https://doi.org/10.1186/s13012-018-0784-z.
Bandura, A. (2006). Guide for constructing self-efficacy scales. In F. Pajares & T. Urdan (Eds.), Self-efficacy beleifs of adolescents. (pp. 307–337). Information Age Publishing.
Bandura, A. (2004). Health promotion by social cognitive means. Health Education and Behavior, 31(2), 143–164. https://doi.org/10.1177/1090198104263660.
Reeve, B. B., Hays, R. D., Bjorner, J. B., Cook, K. F., Crane, P. K., Teresi, J. A., et al. (2007). Psychometric evaluation and calibration of health-related quality of life item banks: Plans for the Patient-Reported Outcomes Measurement Information System (PROMIS). Medical Care, 45(5 Suppl 1), S22-31. https://doi.org/10.1097/01.mlr.0000250483.85507.04.
Cella, D., Riley, W., Stone, A., Rothrock, N., Reeve, B., Yount, S., et al. (2010). The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. Journal of Clinical Epidemiology, 63(11), 1179–1194. https://doi.org/10.1016/j.jclinepi.2010.04.011.
DeWalt, D. A., Rothrock, N., Yount, S., Stone, A. A., & PROMIS Cooperative Group. (2007). Evaluation of item candidates: The PROMIS qualitative item review. Medical care, 45(5 Suppl 1), S12–S21. https://doi.org/10.1097/01.mlr.0000254567.79743.e2.
Clark, L. A., & Watson, D. (1995). Constructing validity: Basic issues in objective scale development. Psychological Assessment, 7(3), 309–319.
Fihn, S. D., Francis, J., Clancy, C., Nielson, C., Nelson, K., Rumsfeld, J., et al. (2014). Insights from advanced analytics at the veterans health administration. Health Affairs, 33(7), 1203–1211. https://doi.org/10.1377/hlthaff.2014.0054.
Wong, E. S., Wang, V., Liu, C. F., Hebert, P. L., & Maciejewski, M. L. (2015). Do Veterans health administration enrollees generalize to other populations? Medical Care Research and Review. https://doi.org/10.1177/1077558715617382.
Hernandez, S. E., Sylling, P. W., Mor, M. K., Fine, M. J., Nelson, K. M., Wong, E. S., et al. (2019). Developing an algorithm for combining race and ethnicity data sources in the Veterans health administration. Military Medicine, 185(3–4), 3495-e500. https://doi.org/10.1093/milmed/usz322.
Nelson, K. M., Chang, E. T., Zulman, D. M., Rubenstein, L. V., Kirkland, F. D., & Fihn, S. D. (2019). Using predictive analytics to guide patient care and research in a national health system. Journal of General Internal Medicine, 34(8), 1379–1380. https://doi.org/10.1007/s11606-019-04961-4.
Wagner, T. H., Almenoff, P., Francis, J., Jacobs, J., & Pal Chee, C. (2018). Assessment of the Medicare advantage risk adjustment model for measuring veterans affairs hospital performance. JAMA Network Open, 1(8), e185993. https://doi.org/10.1001/jamanetworkopen.2018.5993.
Gruber-Baldini, A. L., Velozo, C., Romero, S., & Shulman, L. M. (2017). Validation of the PROMIS® measures of self-efficacy for managing chronic conditions. Quality of Life Research, 26(7), 1915–1924. https://doi.org/10.1007/s11136-017-1527-3.
Dyer, N., Sorra, J. S., Smith, S. A., Cleary, P. D., & Hays, R. D. (2012). Psychometric properties of the consumer assessment of healthcare providers and systems (CAHPSs) clinician and group adult visit survey. Medical Care, 50(11), 7.
Kimerling, R., Pavao, J., Greene, L., Karpenko, J., Rodriguez, A., Saweikis, M., & Washington, D. L. (2015). Access to mental health care among women Veterans: Is VA meeting women’s needs? Medical Care, 53(4 Suppl 1), S97–S104. https://doi.org/10.1097/MLR.0000000000000272.
Bollen, K., & Lennox, R. (1991). Conventional wisdom on measurement: A structural equation perspective. Psychological Bulletin, 110(2), 305–314. https://doi.org/10.1037/0033-2909.110.2.305.
Streiner, D. L., Norman, G. R., & Cairney, J. (2015). Health measurement scales: A practical guide to their development and use. . Oxford University Press.
Revelle, W. (1979). Hierarchical cluster analysis and the internal structure of tests. Multivariate Behavioral Research, 14(1), 57–74. https://doi.org/10.1207/s15327906mbr1401_4.
Reise, S. P., Morizot, J., & Hays, R. D. (2007). The role of the bifactor model in resolving dimensionality issues in health outcomes measures. Quality of Life Research, 16(1), 19–31. https://doi.org/10.1007/s11136-007-9183-7.
Reise, S. P., Bonifay, W. E., & Haviland, M. G. (2013). Scoring and modeling psychological measures in the presence of multidimensionality. Journal of Personality Assessment, 95(2), 129–140. https://doi.org/10.1080/00223891.2012.725437.
Chapman, B. P., Weiss, A., & Duberstein, P. (2016). Statistical learning theory for high dimensional prediction: Application to criterion-keyed scale development. Psychological Methods, 21(4), 603–620. https://doi.org/10.1037/met0000088.
Reise, S. P., Moore, T. M., & Haviland, M. G. (2010). Bifactor models and rotations: Exploring the extent to which multidimensional data yield univocal scale scores. Journal of Personality Assessment, 92(6), 544–59. https://doi.org/10.1080/00223891.2010.496477.
Smits, N., van der Ark, L. A., & Conijn, J. M. (2018). Measurement versus prediction in the construction of patient-reported outcome questionnaires: Can we have our cake and eat it? Quality of Life Research, 27(7), 1673–1682. https://doi.org/10.1007/s11136-017-1720-4.
Elleman, L. G., McDougald, S. K., Condon, D. M., & Revelle, W. (2020). That takes the BISCUIT: A comparative study of predictive accuracy and parsimony of four statistical learning techniques in personality data, with data missingness conditions. European Journal of Personality Assessment. https://doi.org/10.31234/osf.io/tuqap.
Samejima, F. (1968). Estimation of latent ability using a response pattern of graded scores. ETS Research Bulletin Series, 1968(1), i–169. https://doi.org/10.1002/j.2333-8504.1968.tb00153.x.
Gibbons, R. D., Bock, R. D., Hedeker, D., Weiss, D. J., Segawa, E., Bhaumik, D. K., et al. (2007). Full-information item bifactor analysis of graded response data. Applied Psychological Measurement, 31(1), 4–19. https://doi.org/10.1177/0146621606289485.
Toland, M. D., Sulis, I., Giambona, F., Porcu, M., & Campbell, J. M. (2017). Introduction to bifactor polytomous item response theory analysis. Journal of School Psychology, 60, 41–63. https://doi.org/10.1016/j.jsp.2016.11.001.
Stucky, B. D., Thissen, D., & Edelen, M. O. (2013). Using logistic approximations of marginal trace lines to develop short assessments. Applied Psychological Measurement, 37(1), 41–57. https://doi.org/10.1177/0146621612462759.
Choi, S. W., Gibbons, L. E., & Crane, P. K. (2011). lordif : An R package for detecting differential item functioning using iterative hybrid ordinal logistic regression/item response theory and Monte Carlo simulations. Journal of Statistical Software. https://doi.org/10.18637/jss.v039.i08.
Hays, R. D., Calderón, J. L., Spritzer, K. L., Reise, S. P., & Paz, S. H. (2018). Differential item functioning by language on the PROMIS® physical functioning items for children and adolescents. Quality of Life Research, 27(1), 235–247. https://doi.org/10.1007/s11136-017-1691-5.
Revelle, W. (2020) psych: Procedures for Personality and Psychological Research. 2.0.12 Evanston. Illinois: Northwestern University. https://CRAN.R-project.org/package=psych.
Rosseel, Y. (2012). lavaan: An R package for structural equation modeling. Journal of Statistical Software. https://doi.org/10.18637/jss.v048.i02.
Chalmers, R. P. (2012). mirt: A multidimensional item response theory package for the R environment. Journal of Statistical Software. https://doi.org/10.18637/jss.v048.i06.
Bock, R. D., & Mislevy, R. J. (1982). Adaptive EAP estimation of ability in a microcomputer environment. Applied Psychological Measurement, 6(4), 431–444. https://doi.org/10.1177/014662168200600405.
Koh, H. K., Brach, C., Harris, L. M., & Parchman, M. L. (2013). A proposed “health literate care model” would constitute a systems approach to improving patients’ engagement in care. Health Affairs (Millwood), 32(2), 357–67. https://doi.org/10.1377/hlthaff.2012.1205.
Roberts, E. T., Zaslavsky, A. M., Barnett, M. L., Landon, B. E., Ding, L., & McWilliams, J. M. (2018). Assessment of the effect of adjustment for patient characteristics on hospital readmission rates: Implications for pay for performance. JAMA Internal Medicine, 178(11), 1498–1507. https://doi.org/10.1001/jamainternmed.2018.4481.
Shakir, M., Armstrong, K., & Wasfy, J. H. (2018). Could pay-for-performance worsen health disparities? Journal of General Internal Medicine, 33(4), 567–569. https://doi.org/10.1007/s11606-017-4243-3.
Hausmann, L. R. M., Canamucio, A., Gao, S., Jones, A. L., Keddem, S., Long, J. A., & Werner, R. (2017). Racial and ethnic minority concentration in veterans affairs facilities and delivery of patient-centered primary care. Population Health Management, 20(3), 189–198. https://doi.org/10.1089/pop.2016.0053.
Ginsburg, P. B. (2013). Achieving health care cost containment through provider payment reform that engages patients and providers. Health Affairs (Project Hope), 32(5), 929–934. https://doi.org/10.1377/hlthaff.2012.1007.
Acknowledgements
This manuscript is supported by grants #I21HX001855 and 1I01HX002317 from the United States (US) Department of Veterans Affairs Health Services Research and Development Service. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Funding
This manuscript is supported by Grants #I21HX001855 and 1I01HX002317 from the United States (US) Department of Veterans Affairs Health Services Research and Development Service.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schalet, B.D., Reise, S.P., Zulman, D.M. et al. Psychometric evaluation of a patient-reported item bank for healthcare engagement. Qual Life Res 30, 2363–2374 (2021). https://doi.org/10.1007/s11136-021-02824-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-021-02824-2