Abstract
This study was to investigate the association between sex hormone levels and metabolic syndrome (MetS) risk in female schizophrenia inpatients. In total, 93 female schizophrenia patients were enrolled based on their electronic medical records of hospitalization at the Zigong Psychiatric Research Center, China, between August 2022 to September 2022. Baseline information was collected retrospectively from medical records 6 months before. Logistic regression analysis was applied to assess the potential relationship between sex hormone levels and the risk of developing MetS. 31.2% (29/93) of the total patients, 25.5% (12/47) of the 18–49 age group, and 37.0% (17/46) of the ≥ 50 age group had a history of MetS; the newly-developed MetS prevalence among all female schizophrenia patients was 15.05% (14/93), which was slightly higher but not statistically significant in older patients (age ≥ 50) than in younger patients (age 18–49) (≥ 50 vs. 18–49, 21.74% vs. 8.5%, p = 0.074). Univariate analysis of sex hormone levels and developed MetS discovered that only high prolactin levels correlated with developed MetS in total participants (p = 0.006), especially in older patients (p = 0.004), while estradiol and testosterone levels were not associated. Furthermore, univariate logistic regression analysis of the total participants and with an adjusted model of the ≥ 50 age group confirmed the association of prolactin with MetS in all (OR = 1.016, 95%CI:1.002–1.029, p = 0.023), and older female schizophrenia patients (OR = 1.04, 95%CI: 1.01–1.07, p = 0.008). High serum levels of prolactin in older patients (age ≥ 50) were strongly correlated with the risk of developing MetS among female schizophrenia patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Schizophrenia, which affects over 21 million people worldwide, is a debilitating and chronic mental disorder characterized by clinical behavioral symptoms and underlying abnormalities in brain function [1]. The life expectancy of schizophrenia patients is approximately 10–20 years less than that of the general population [2, 3]. Antipsychotic drugs are the main form of treatment for schizophrenia, and long-term maintenance antipsychotic treatment can protect against all-cause mortality (RR = 0.71, 95% CI: 0.59–0.84, n = 11) compared with no use of anti-psychotics [4]. However, almost all antipsychotic drugs lead to the development of metabolic syndrome (MetS) [5].
MetS includes changes in pathological, clinical, and metabolic parameters and at least three of five medical conditions, namely, abdominal obesity, high blood sugar, high serum triglycerides, high blood pressure, and low serum high-density lipoprotein. Studies have estimated a 37 ~ 67% prevalence of MetS in schizophrenia patients, which is significantly higher than that in the general population [6, 7]. It is reported that MetS is a major cause of reduced life expectancy in schizophrenia patients [8], especially as MetS is a high-risk factor for cardiovascular diseases [9], significantly increasing the mortality risk (RR = 2 to 3) in schizophrenic patients compared with their non-schizophrenic counterparts [10]. The comorbidity of schizophrenia and the MetS is common, and is associated with disturbances of glucose and lipid metabolism related to antipsychotic drugs [11], inadequate individual nutrition education [12], and self-neglect [13]. Thus, it is critical to closely examine the development of MetS in schizophrenia for the early detection, management of these issues and the improvement of outcomes in these patients.
Studies have reported a strong association between the levels of sex hormones and MetS risk in patients with schizophrenia. These include an increased cortisol-to-testosterone (C/T) ratio [14] or cortisol-to-dehydroepiandrosterone sulfate (C/D) ratio [15], and estrogen(16). Nevertheless, to our knowledge, most studies on the associations between sex hormones and MetS risk have focused mainly on male schizophrenic patients. Thus, the present study investigated the issue in female patients with schizophrenia to test the hypothesis that sex hormone levels are also associated with MetS risk in female schizophrenia patients.
Materials and Methods
Study Design and Patient Profile
This study design was observational and retrospective. The data were collected from 155 hospitalized female patients with stable schizophrenia from August 2022 to September 2022 at the Zigong Psychiatric Research Center, China. The schizophrenia diagnosis was performed by two highly trained psychiatrists following the “International Classification of Disease, 10th revision guidelines”. The patients were excluded if they had: 1) severely impaired hepatic or renal function, 2) autoimmune disease, 3) were undergoing antitumor therapies, and/or 4) had missing clinical data or recent hospitalization. Ultimately, 93 female patients with schizophrenia were enrolled in this study, of which 47 were 18–49 years old and 46 were aged over 50. This investigation strictly followed the Declaration of Helsinki, and received ethical approval from the Zigong Psychiatric Research Center in western China (IRB number: 20210101).
Covariates
Information on covariates was obtained from patients who had been hospitalized for over 6 months. The patients were defined as having developed MetS if they had one or more MetS symptoms, including hypertension, diabetes or hyperlipidemia, between August 2022 and September 2022, and which had been absent during the previous six months before. The names and necessary information on patients were obtained from the hospital’s electronic record. The baseline information included age, weight, height, disease duration, marital status, smoking and drinking history, COVID-19 history, menarche age, menstrual status, antipsychotic drug usage (typical or atypical), and reported MetS history including diabetes, hypertension, and hyperlipidemia. Diabetes, hypertension, and hyperlipidemia comorbidities were assessed based on their corresponding diagnostic criteria. Univariate analysis data with p-values < 0.05 associated with MetS were subjected to model correction. We generated an adjusted model with statistically significant variables such as Body Mass Index (BMI) and prolactin levels for enrolled patients ≥ 50 years old.
Statistical Analyses
All data analyses were performed by SPSS 25.0 software. A two-sided p-value < 0.05 was set as the significance threshold. Data are presented as means ± standard deviations, numbers (percentages), or median (p25, p75). Comparisons between the MetS and non-MetS groups were performed using rank-sum tests, Student's t-test, or Pearson's chi-square tests as appropriate. Logistic regression analysis was used to investigate the potential association between serum sex hormone levels with MetS risk among female schizophrenic patients. Covariates were included in model correction only if they were statistically significant according to the single-factor analysis (p < 0.05).
Results
This study had certain limitations. Firstly, the inpatients were from only one center. Secondly, the sample size was relatively small, and the data of some older inpatients were missing. Thirdly, this is a case–control study with some missing and irreparable information. For example, there were no comprehensive data on all sex hormones, and only the information on estradiol, prolactin and testosterone was relatively complete. Despite these limitations, however, we obtained some useful results. In the future, more comprehensive prospective investigations, from multiple centers with larger patient populations, broader age ranges, and follow-up durations are needed to confirm our results.
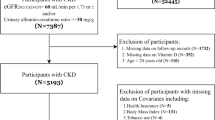
Figure 1 depicts the patient selection process for this retrospective investigation. Overall, 155 female patients with schizophrenia who were hospitalized between August 2022 and September 2022 were enrolled. Of these, 26 patients had short hospitalizations and 15 patients had been recently hospitalized and, therefore, did not have clinical data from the previous six months. Furthermore, 10 patients with severely impaired hepatic and renal function, 6 patients with autoimmune disease, and 5 patients who were undergoing anti-tumor treatment were excluded. Ultimately, 93 patients were included in the analysis.
Table 1 summarizes the data from developed MetS patients versus non-developed MetS patients. Overall, 31.2% (29/93) of the total patient cohort, including 25.5% (12/47) of the 18–49 aged group and 37.0% (17/46) of the ≥ 50 age group had a history of MetS. The prevalence of recently developed MetS in all the female patients with schizophrenia was 15.05% (14/93); this was slightly higher in older patients (aged ≥ 50) than in younger patients (aged 18–49) (≥ 50 vs. 18–49, 21.74% vs. 8.5%, p = 0.074) although the difference was not statistically significant. Meanwhile, age, marital status, disease duration, menarche age, MetS history, antipsychotic drug usage (typical or atypical), and amenorrhea status did not differ significantly between the MetS and non-MetS patients. None of the patients had a history of drinking, smoking, or COVID-19 (data not shown). However, compared with the non-MetS group, MetS was associated with significantly higher levels of serum cholesterol in the 18–49 age group (p = 0.009) and BMI in the ≥ 50 age group (p = 0.036).
Univariate analysis of sex hormone levels and MetS showed that only high levels of serum prolactin were correlated with MetS risk in the overall patients (p = 0.006) and the ≥ 50 age group (p = 0.004) (Table 2). Univariate logistic regression analysis of high prolactin levels (p = 0.023, OR = 1.016, 95%CI:1.002–1.029) in all participants indicated an increased risk of developing MetS. We further adjusted the potential confounders, including an increase in BMI and high prolactin levels in the ≥ 50 age group, and the data verified the association of elevated prolactin levels with an increased risk of developing MetS (p = 0.008, OR = 1.04, 95%CI:1.01–1.07; Table 3).
Discussion
This study investigated the association of sex hormone levels with the risk of developing MetS in female inpatients with schizophrenia. Specifically, serum estradiol and testosterone levels showed no significant association with the development of MetS within six months in the entire cohort while high serum prolactin levels were found to be associated with an increased risk of developing MetS in patients over the age of 50. Besides, the BMI values of patients aged 50 and over and the cholesterol levels of patients aged 18–49 differed significantly between the MetS and non-MetS groups. Based on our results and in terms of the association of sex hormones with MetS risk, we strongly recommend that clinicians pay close attention to prolactin levels and BMI in female patients with schizophrenia over the age of 50 years, as well as cholesterol levels, rather than estradiol or testosterone, in patients aged between 18 and 49.
Schizophrenia is a chronic psychiatric disorder that requires the lifelong use of medication. Antipsychotic drugs are both the first-line and main treatment for schizophrenia(4, 17). Previous studies have shown associations between a higher risk of MetS and the duration of the illness and continuous use of antipsychotic drugs in schizophrenic patients [18, 19]. Interestingly, the disease duration showed no significant difference between the developed and non-developed MetS groups in this study. In other words, the results of our study contrasted with previous thinking that there was no link between MetS prevalence and long-term antipsychotic drug use in female schizophrenic patients. These differences may be due to two main reasons: 1) the sample size was small; 2) this was a case–control study with some missing and irreparable information, such as the use of antihypertensive or hypolipidemic drugs. Larger patient populations and longer follow-ups involving prospective data collection and analysis are warranted to confirm these differences.
A previous study found that antipsychotic treatment of schizophrenia increased the levels of prolactin [20]. Another study proposed that abnormalities in the prolactin pathway may contribute to schizophrenia, type 2 diabetes, and/or MetS [21]. Consistently, we also observed a strong association between high prolactin levels and MetS risk in the present study. Notably, testosterone and estradiol levels showed no such association. Gallagher et al. found that cortisol and dehydroepiandrosterone sulfate (DHEA-S) levels were significantly increased in chronic schizophrenia patients [22]. DHEAS can be converted to either androgens or estrogens depending on the gender. Testosterone and cortisol levels in men could be a better predictor of MetS risk than the cortisol-to-testosterone ratio [23]. However, in the present study, testosterone levels did not differ significantly between female schizophrenia patients and the normal control [24], implying that testosterone levels in female schizophrenia patients did not do any harm. These results also suggest that excessive measurement of serum testosterone levels is unnecessary as a simple assessment of MetS risk. A recent meta-analysis suggested that estradiol can be an effective and safe adjunct treatment for female schizophrenia patients [25]. Riordan et al. found similar results in adult female Sprague–Dawley rats [26]. Although we found no statistically significant association of estradiol levels with MetS, we did observe a lower level of estradiol in the MetS group. The most likely reason for the difference could be that the number of enrolled patients was relatively small, leading to a possible discrepancy. Studies with lager sample sizes and broader age groups should be undertaken to confirm the potential relationship between low estradiol levels and MetS in female patients with schizophrenia.
In addition, the association between prolactin levels and MetS risk was inconsistent in the different age groups. Only those over 50 years of age showed a strong relationship between high prolactin levels and MetS risk. The prolactin levels in patients aged 18–49 showed no association with MetS risk, however, the cholesterol levels showed a significant difference between the MetS and non-MetS groups. Moreover, the adjusted model verified that the BMI of female patients aged 50 and over was also significantly associated with MetS risk. These results imply that precise clinical intervention should be undertaken according to the patient’s age to reduce the risk of MetS development, specifically, by paying close attention on cholesterol levels in younger patients (18–49) and BMI and prolactin levels in patients older than 50 years.
Conclusions
The findings showed that high serum levels of prolactin in the ≥ 50 age group were strongly associated with MetS risk in female patients with schizophrenia.
References
Jauhar S, Johnstone M, McKenna PJ. Schizophrenia Lancet. 2022;399(10323):473–86. https://doi.org/10.1016/s0140-6736(21)01730-x.
Correll CU, Solmi M, Croatto G, Schneider LK, Rohani-Montez SC, Fairley L, et al. Mortality in people with schizophrenia: a systematic review and meta-analysis of relative risk and aggravating or attenuating factors. World Psychiatry. 2022;21(2):248–71. https://doi.org/10.1002/wps.20994.
Hjorthøj C, Stürup AE, McGrath JJ, Nordentoft M. Years of potential life lost and life expectancy in schizophrenia: a systematic review and meta-analysis. Lancet Psychiatry. 2017;4(4):295–301. https://doi.org/10.1016/s2215-0366(17)30078-0.
Lally J, MacCabe JH. Antipsychotic medication in schizophrenia: a review. Br Med Bull. 2015;114(1):169–79. https://doi.org/10.1093/bmb/ldv017.
Khasanova AK, Dobrodeeva VS, Shnayder NA, Petrova MM, Pronina EA, Bochanova EN, et al. Blood and urinary biomarkers of antipsychotic-induced metabolic syndrome. Metabolites. 2022;12(8). https://doi.org/10.3390/metabo12080726.
Vancampfort D, Wampers M, Mitchell AJ, Correll CU, De Herdt A, Probst M, et al. A meta-analysis of cardio-metabolic abnormalities in drug naïve, first-episode and multi-episode patients with schizophrenia versus general population controls. World Psychiatry. 2013;12(3):240–50. https://doi.org/10.1002/wps.20069.
Deh M, Schreurs V, Vancampfort D, van Wınkel R. Metabolic syndrome in people with schizophrenia: a review. World Psychiatry. 2009;8(1):15–22. https://doi.org/10.1002/j.2051-5545.2009.tb00199.x.
Laursen TM. Life expectancy among persons with schizophrenia or bipolar affective disorder. Schizophr Res. 2011;131(1–3):101–4. https://doi.org/10.1016/j.schres.2011.06.008.
Lind L, Sundström J, Ärnlöv J, Risérus U, Lampa E. A longitudinal study over 40 years to study the metabolic syndrome as a risk factor for cardiovascular diseases. Sci Rep. 2021;11(1):2978. https://doi.org/10.1038/s41598-021-82398-8.
Olfson M, Gerhard T, Huang C, Crystal S, Stroup TS. Premature Mortality Among Adults With Schizophrenia in the United States. JAMA Psychiat. 2015;72(12):1172–81. https://doi.org/10.1001/jamapsychiatry.2015.1737.
Enez Darcin A, Yalcin Cavus S, Dilbaz N, Kaya H, Dogan E. Metabolic syndrome in drug-naïve and drug-free patients with schizophrenia and in their siblings. Schizophr Res. 2015;166(1–3):201–6. https://doi.org/10.1016/j.schres.2015.05.004.
Sugawara N, Sagae T, Yasui-Furukori N, Yamazaki M, Shimoda K, Mori T, et al. Effects of nutritional education on weight change and metabolic abnormalities among patients with schizophrenia in Japan: A randomized controlled trial. J Psychiatr Res. 2018;97:77–83. https://doi.org/10.1016/j.jpsychires.2017.12.002.
Jayatilleke N, Hayes RD, Chang CK, Stewart R. Acute general hospital admissions in people with serious mental illness. Psychol Med. 2018;48(16):2676–83. https://doi.org/10.1017/s0033291718000284.
Smith GD, Ben-Shlomo Y, Beswick A, Yarnell J, Lightman S, Elwood P. Cortisol, testosterone, and coronary heart disease: prospective evidence from the Caerphilly study. Circulation. 2005;112(3):332–40. https://doi.org/10.1161/circulationaha.104.489088.
Vuksan-Ćusa B, Sagud M, Mihaljević-Peleš A, Jakšić N, Jakovljević M. Metabolic syndrome and cortisol/DHEAS ratio in patients with bipolar disorder and schizophrenia. Psychiatr Danub. 2014;26(2):187–9.
Regitz-Zagrosek V, Lehmkuhl E, Mahmoodzadeh S. Gender aspects of the role of the metabolic syndrome as a risk factor for cardiovascular disease. Gend Med. 2007;4(Suppl B):S162-77. https://doi.org/10.1016/s1550-8579(07)80056-8.
Barnes TR, Drake R, Paton C, Cooper SJ, Deakin B, Ferrier IN, et al. Evidence-based guidelines for the pharmacological treatment of schizophrenia: Updated recommendations from the British Association for Psychopharmacology. J Psychopharmacol. 2020;34(1):3–78. https://doi.org/10.1177/0269881119889296.
Jeong SH, Lee NY, Kim SH, Chung IW, Youn T, Kang UG, et al. Long-term evolution of metabolic status in patients with schizophrenia stably maintained on second-generation antipsychotics. Psychiatry Investig. 2018;15(6):628–37. https://doi.org/10.30773/pi.2018.01.18.1.
Mitchell AJ, Vancampfort D, Sweers K, van Winkel R, Yu W, De Hert M. Prevalence of metabolic syndrome and metabolic abnormalities in schizophrenia and related disorders–a systematic review and meta-analysis. Schizophr Bull. 2013;39(2):306–18. https://doi.org/10.1093/schbul/sbr148.
Zhu Y, Zhang C, Siafis S, Zhuo K, Zhu D, Wu H, et al. Prolactin levels influenced by antipsychotic drugs in schizophrenia: A systematic review and network meta-analysis. Schizophr Res. 2021;237:20–5. https://doi.org/10.1016/j.schres.2021.08.013.
Postolache TT, Del Bosque-Plata L, Jabbour S, Vergare M, Wu R, Gragnoli C. Co-shared genetics and possible risk gene pathway partially explain the comorbidity of schizophrenia, major depressive disorder, type 2 diabetes, and metabolic syndrome. Am J Med Genet B Neuropsychiatr Genet. 2019;180(3):186–203. https://doi.org/10.1002/ajmg.b.32712.
Gallagher P, Watson S, Smith MS, Young AH, Ferrier IN. Plasma cortisol-dehydroepiandrosterone (DHEA) ratios in schizophrenia and bipolar disorder. Schizophr Res. 2007;90(1–3):258–65. https://doi.org/10.1016/j.schres.2006.11.020.
Han Y, Ji H, Liu L, Zhu Y, Jiang X. The relationship of functional status of cortisol, testosterone, and parameters of metabolic syndrome in male schizophrenics. Biomed Res Int. 2020;2020:9124520. https://doi.org/10.1155/2020/9124520.
Bulut SD, Bulut S, Gundogmus AG, Aydemir C. Serum DHEA-S, testosterone and cortisol levels in female patients with schizophrenia. Endocr Metab Immune Disord Drug Targets. 2018;18(4):348–54. https://doi.org/10.2174/1871530318666180212102128.
Li Z, Wang Y, Wang Z, Kong L, Liu L, Li L, et al. Estradiol and raloxifene as adjunctive treatment for women with schizophrenia: A meta-analysis of randomized, double-blind, placebo-controlled trials. Acta Psychiatr Scand. 2022. https://doi.org/10.1111/acps.13530.
Riordan AJ, Schaler AW, Fried J, Paine TA, Thornton JE. Estradiol and luteinizing hormone regulate recognition memory following subchronic phencyclidine: Evidence for hippocampal GABA action. Psychoneuroendocrinology. 2018;91:86–94. https://doi.org/10.1016/j.psyneuen.2018.02.024.
Acknowledgements
This work was funded by the Collaborative innovation project of Zigong Institute of Brain Science(No:2022ZCNKY18).
Author information
Authors and Affiliations
Contributions
Hongli Zhang contributed to the data collection and writing of this article. Jin Peng contributed to the writing and proofreading of this article. Yilin Wang contributed to the guidance and analysis of this article.
Corresponding author
Ethics declarations
Ethical Approval
This study strictly followed the Declaration of Helsinki and received ethical approval from the Zigong Psychiatric Research Center (IRB number: 2022062003).
Conflict of Interest
There is no conflict of interest in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, H., Peng, J. & Wang, Y. Association Between Prolactin, Estradiol, and Testosterone Levels and the Development of Metabolic Syndrome in Female Inpatients with Schizophrenia: A Case–Control Study. Psychiatr Q 94, 211–220 (2023). https://doi.org/10.1007/s11126-023-10025-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11126-023-10025-y