Abstract
Objective
To examine the clinic no-show rate across different modalities of care delivery (Face to Face, Telephone visits and Audio–Video visits).
Methods
Clinic no show data for adult patients was extracted from the electronic health records used by the psychiatry clinic for 10 months before pandemic and 10 months during pandemic. No show rate was analyzed by visits type (new vs return) and across different modalities (face-to-face vs Telephone vs Audio–Video) before and during COVID pandemic.
Results
There were 13,916 scheduled visits during the 10-month period before the pandemic of which 2,522 were no show. There were 13,251 scheduled visits during the 10-month period during the COVID pandemic of which 2,029 were no show. The overall clinic no show rate decreased from pre pandemic to pandemic period (18.1% vs 15.3%) after transitioning to telehealth. Across different modalities during the pandemic, the no-show rate for Telephone visits was significantly lower than for face- to-face visits. No difference was identified for no-show rates between face-to-face visits and audio–video visits during the pandemic. The no-show rate for face-to-face visits before the pandemic compared to during the pandemic also showed no difference.
Conclusion
Using technology in health care delivery can decrease the clinic no show rate. Digital literacy for patients and providers is critical for successful utilization of telehealth.
Similar content being viewed by others
Introduction
Psychiatry clinics, especially those associated with academic medical institutions, have long struggled with higher no-show rates [1, 2]. No-show attendance rates for outpatient psychiatry clinic are reported by various studies to differ anywhere from 2–30% [3]. Furthermore, the no-show rate for initial psychiatric evaluations is twice that of most other specialties [2].Gajwani reported a no-show rate of 31% at University of Texas Health Sciences Center at Houston, an academic institution [1]. Patients who no-show to initial psychiatric appointments have been found to have more frequent hospitalization and emergency department visits. [2, 4] In addition to the patients not being treated due to missed appointments, there is concern for the large financial burden placed on the clinics with monetary loss associated with no-show rates. At the Michael E DeBakey VA Medical Center in Houston, Texas, the average cost of a no-show patient across multiple departments (Audiology, Cardiology, Dermatology, Eye Care, Gastroenterology, Mental Health, Orthopedics, Podiatry, Primary Care, and Urology) was $196 in 2008 [5]. At the University of Missouri outpatient psychiatry clinic, the no-shows represented between $11–19 million in lost revenue [6]. Furthermore, high no-show rates create increased burden on clinicians and administrative staff in the form of contacting and rescheduling patients [7]. No show appointments not only waste clinic resources, but they also prolong the waiting time for patients wanting to see a provider. Clinical capacity and workflow are not optimally utilized during no show appointments as time and clinic resources are wasted whereby providers could be seeing other patients [8]. This prolongs the waiting time for patients waiting to see a provider to establish care and delays treatment for patients who are already established/seeking care [9].
Due to the financial burden of missed appointments and the wasted time of providers and resources, several studies have investigated reasons for missed appointments. Common attributes of patients who no-show to their appointments include lower socioeconomic status, younger age, ethnic minorities, prior history of no-show, living farther from outpatient clinics, poorly insured, and the less educated [7, 10]. The University of Missouri’s data revealed that the scheduler who made the appointments affected one-third of the probability of whether the patient would show. This was based off whether the scheduler followed protocol assigning appointments vs asking the patients’ time preference [6]. Common reasons reported for missed appointments by patients include patient illness, oversleeping, inability to get off work/scheduling conflict, transportation issues, lost appointment card, believing the appointment was on a different day or time, lack of understanding of the scheduling system, and motivational issues/avoidance of treatment [7, 10]. Forgetfulness as a factor of missed appointments is a response heard twice as often in psychiatry outpatient clinics than that other specialties [1]. Multiple studies have reported that factors affecting missed initial appointments include male sex, younger age, lower socioeconomic status, comorbid substance abuse disorders, poor family support, poor adherence to psychotropic drugs, lack of or limited health care insurance, poor social functioning, unemployment, longer periods from contact to appointment, higher numbers of previous hospital admissions, and shorter hospital stays. [2, 4], Common practices that have been shown to reduce no-show rates include collaborating with referral sources for new patient evaluations, reducing clinic wait times, making reminder calls, using behavioral engagement strategies, and creating a welcoming clinic environment [8]. Parikh et al. studied patient no-show rates among patients receiving a clinic staff reminder, automated appointment reminder or no reminder, with results indicating no show rates lower in that respective order. Staff reminder calls are most commonly employed and in general health settings reduced no-show rates from 23.1% to 13.6% [8]. Ultimately, reducing no-show rates leads to improvement for patients, physicians, and clinic workflow.
The current COVID-19 pandemic has presented challenges to delivering quality health care to both new and established patients. There was special concern for delivering continuity of care to those with mental illness, as they may be more susceptible to decompensation from fear of acquiring the virus and the isolation of quarantine and social distancing. [11, 12].
The field of psychiatry has pioneered the way for telemedicine, allowing easy implementation of telepsychiatry into current practice [13–15]. This transition was made more feasible with the lifting of some prior telehealth restrictions. The Coronavirus Preparedness and Response Supplemental Appropriations Act was signed into law on March 6, 2020 [16]. This act waived telehealth reimbursement restrictions for geographic and originating site restrictions. The Health and Human Services Office of Civil Rights has additionally announced that it would waive HIPPA penalties for using non-HIPAA compliant video conferencing software during video conferencing appointments. These include popular platforms such as Skype, FaceTime, etc. [17].
It is largely unknown how implementation of telepsychiatry visits during the COVID-19 era impacted clinic workflow. This study examined the no show rate in a large academic outpatient psychiatry clinic in eastern North Carolina before and during COVID-19. The clinic serves a multi-county catchment area. Given the widespread availability of virtual platforms to the public, it was anticipated that the no-show rate would drop, and clinic workflow would improve in the outpatient psychiatry clinic.
Methods
This study was conducted at the ambulatory psychiatry clinic at the East Carolina University which is a large academic outpatient psychiatry practice in eastern North Carolina. Like other institutions across the country, this clinic transitioned from face-to-face vits to telehealth including both telephone visits and audio–video visits during COVID pandemic. The clinic used Zoom for Healthcare (HIPPA compliant) as the virtual encounter platform. The patients were also given the option of continuing to come in person for visits. Data about clinic appointments for adult patients (age 18 and above) was collected from Electronic Medical Record system for 20 months, from May 2019 to December 2020. We compared the clinic no show rate for the 10-month pre-Covid period (from May 2019 to Feb 2020) to 10 months during Covid pandemic (March 2020 to Dec 2020). During pre-Covid period all the appointments were face to face. During the Covid period telephone visits, audio–video visits and face to face visits were included.
We defined clinic no show rate as the total number of patients who did not attend the appointment divided by the total number of patients scheduled. We did not include cancelled appointments or rescheduled appointments in calculating the no show rate. Data was analyzed by using SAS software (SAS 9.4, Cary, NC). We compared no show rates by appointment type (New vs Return visit) as well as by modality (Telephone vs Audio–Video vs Face to Face visit). This study was considered exempt from institutional review board approval.
Results
During the 10-month pre-COVID-19 period there were 13,916 scheduled appointments, of which 2,522 were no-show. During the 10-month COVID-19 period, there were 13,251 scheduled appointments, of which 2,029 were no-show (Table 1 and Fig. 1). The overall no-show rate was 18.1% for the pre-COVID-19 period and it dropped to 15.3% for the COVID-19 period, which was a significant difference (p < 0.0001). For new patients, the no-show rate dropped from 29.8% to 28% (p = 0.2696), and for returning patients it dropped from 16.4% to 13.9% (p < 0.0001).
Prior to the pandemic, all appointments were face-to-face. During the COVID-19 period, some appointments were face-to-face, but phone and virtual appointments were also introduced. We compared the no-show rates for face-to-face appointments before and during the pandemic to determine if there were pandemic-related differences across similar appointment types. We also compared the no-show rate during the pandemic for new and return appointments delivered by different modes (phone, virtual) to look for mode-specific differences.
Table 2 and Fig. 2 show the no-show rates for face-to-face appointments for new and return adult visits both before and during COVID-19. No show rate for face-to-face new visits before Covid was 29.8% and during Covid 28.2% (p = 0.3539). No show rate for face-to-face return visits before Covid was 16.4% and during Covid 16% (p = 0.4427). There were no significant differences in no-show rates for similar visits delivered by face-to-face across the two periods (pre-COVID-19 and during COVID-19).
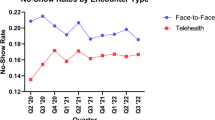
Comparing across modes during COVID-19 period, the no-show rate for phone mode were significantly lower than face-to -face mode for both new visits (p = 0.0208) and return visits (p < 0.0001) (Table 3a, Fig. 3). No-show rates for virtual mode were no better than for face-to-face mode for new visits (p = 0.6812) and return visits (p = 0.186) (Table 3b, Fig. 3).
Discussion
This study demonstrates that in the ambulatory psychiatry clinic at ECU, a large academic outpatient psychiatry practice in eastern North Carolina, the overall no show rate decreased after transitioning to telehealth during COVID pandemic. Even though COVID pandemic created numerous challenges for the society at large, it also created a necessity to adapt quickly to the innovative ways of delivering health care. Telephone and virtual delivery of care made it possible to bridge the physical distancing while maintaining the social distancing and provided opportunity to compare no show rates across different modes.
Psychiatry is well-suited for telehealth and empowers the providers to reach the patients in rural and underserved areas. Before the pandemic, many practices in the country were not using telepsychiatry to reach patients at their homes due to multitude of factors and one of the primary concerns was insurance reimbursement and requirement for being at an originating site [13, 21, 22]. On March 17, 2020, CMS released guidance allowing patients to be seen at home via live video conference without having to be at an originating site for virtual encounters [14, 15, 23]. Then on March 31, 2020, CMS temporarily waived requirements for out of state practitioners to be licensed in the state where they were providing services [14]. The DEA has also suspended the requirement of the Ryan Haight Act that requires providers conduct in person initial evaluations prior to prescribing a controlled substance [24]. DEA licensure in the state where the patient is located to electronically prescribe a controlled substance has also been waived [14, 16]. These provisions have allowed the field of psychiatry to evolve with the COVID-19 pandemic more rapidly and transition from in person to virtual encounters. Initial reports revealed that implementation of telepsychiatry improved outpatient attendance for healthcare delivery [12, 18]. Massachusetts General Hospital-based outpatient psychiatric practice reported a 22% increase in productivity and 20% decrease in no-show rates from pre-COVID period to COVID period [19]. Patient no-show rates for Boston Medical Center psychiatry department dropped to 15% from around 45% [20].
In this study the no show rate for New visits did not differ before and during COVID. No show rate for Return visits was significantly lower during the COVID than before COVID primarily because of using telephone visits. No show rate by telephone mode was significantly lower than other modes (Face to face and Virtual) for new visits (7.7%) and return visits (7.8%). Patients and providers comfort level with using telephone probably contributed to this finding. There were few New visits by Telephone mode than Return visits during COVID. No show rate for virtual mode is no better than Face to Face mode during the COVID (17.1% vs 16%). Low Socioeconomic status and lack of clear policy on what virtual platform to use during the swift transition to telehealth could be possible contributors to the differences in no show rates for telephone and virtual modes. Ease of use with telephone appears to be a driver for the very low no show rate for telephone visits when compared to audio video visits. Another potential contributor is the complexities associated with accessing virtual platforms. Even though virtual platforms have been around for a while, ability to use these platforms may be a limiting factor as it requires technical knowledge and needs some time to learn. This learning curve for the patients and the providers may be one of the factors contributing to increased no show rate for virtual visits when compared to telephone visits. Very low no show rate for telephone visits speaks to the fact that if the patients and providers are comfortable with using the technology, no show rate for virtual visits will decrease. But it can also be impacted by other external factors such as availability of technology to the patients in remote areas including computers and reliable internet, availability of IT support to the clinic as well as patient navigators to educate and guide patients about using the virtual platform that the clinic is using. In addition to these, appropriate policy modifications to support using telehealth can play a significant role in decreasing clinic no show rate.
Limitations
Specific reasons for clinic no shows were not obtained in this study. Data was collected as aggregate no show rate for each modality of care delivery and individual level data was not available to identify the change in clinical symptoms and longitudinal outcomes. The periods compared were not identical times of the year which could have caused a skew in results due to seasonality potentially playing a role in no-show rates. There was no way to determine if decrease in no show rate after transitioning to telehealth during COVID pandemic translated into improved outcomes for the patients. This study took place in an academic psychiatry clinic which may limit generalizability to other specialties and community settings.
Conclusion
Telehealth can decrease the clinic no show rate and has the potential to make a positive impact on the provider and staff time, clinic revenue, patient outcomes and the overall health care system. It is important to understand the learning curve involved for both patients and providers. Successful implementation requires educating patients and providers in using technology, staff and technical support and polices conducive to easy access and widespread utilization of telehealth.
Next Steps
Future studies looking into the reasons for clinic no shows by different modalities of care delivery can help to understand the drivers for no show rate for virtual care. Prospective studies focusing on weather decreased no show rate can translate into improved patient outcomes for telehealth are imperative. It would be helpful to have future studies to evaluate the impact of demographic and socioeconomic factors on telehealth utilization as well as no shows in variety of clinical settings and age groups.
References
Gajwani P. Can what we learned about reducing no-shows in our clinic work for you? Curr Psychiat. 2014;13(9):13–24.
Long J, Sakauye K, Chisty K, Upton J. The Empty Chair Appointment SAGE Open. 2016;6(1):215824401562509. https://doi.org/10.1177/2158244015625094.
Parikh A, Gupta K, Wilson AC, Fields K, Cosgrove NM, Kostis JB. The Effectiveness of Outpatient Appointment Reminder Systems in Reducing No-Show Rates. Am J Med. 2010;123(6):542–8. https://doi.org/10.1016/j.amjmed.2009.11.022.
Cheng K, Huang C, Tsang H, Lin C. Factors related to missed first appointments after discharge among patients with schizophrenia in Taiwan. J Formos Med Assoc. 2014;113(7):436–41. https://doi.org/10.1016/j.jfma.2012.09.016.
Kheirkhah P, Feng Q, Travis LM, Tavakoli-Tabasi S, Sharafkhaneh A. Prevalence, predictors and economic consequences of no-shows. BMC Health Serv Res. 2015;16(1). https://doi.org/10.1186/s12913-015-1243-z.
Butterfield S. Research reveals reasons underlying patient no-shows. 2009. Retrieved November 22, 2020, from https://acpinternist.org/archives/2009/02/no-shows.htm.
Defife JA, Conklin CZ, Smith JM, Poole J. Psychotherapy appointment no-shows: Rates and reasons. Psychotherapy: Theory Res Prac Train. 2010;47(3):413–417. https://doi.org/10.1037/a0021168.
Molfenter T. Reducing Appointment No-Shows: Going from Theory to Practice. Subst Use Misuse. 2013;48(9):743–9. https://doi.org/10.3109/10826084.2013.787098.
Cullen BA. Altering the attendance rate successfully for new patients at an outpatient mental health clinic. Psychiatr Serv. 2018;69(12):1212–4. https://doi.org/10.1176/appi.ps.201800161.
Mehra A, Hoogendoorn CJ, Haggerty G, Engelthaler J, Gooden S, Joseph M, Guiney PA. Reducing Patient No-Shows: An Initiative at an Integrated Care Teaching Health Center. J Am Osteopath Asso. 2018;118(2):77. https://doi.org/10.7556/jaoa.2018.022.
Stoll J, Sadler JZ, Trachsel M. The Ethical Use of Telepsychiatry in the Covid-19 Pandemic. Front Psych. 2020. https://doi.org/10.3389/fpsyt.2020.00665.
Kannarkat JT, Smith NN, Mcleod-Bryant SA. Mobilization of Telepsychiatry in Response to COVID-19–Moving Toward 21st Century Access to Care. Admin Policy Mental Health and Mental Health Serv Res. 2020;47(4):489–91. https://doi.org/10.1007/s10488-020-01044-z.
Chakrabarti S. Usefulness of telepsychiatry: A critical evaluation of videoconferencing-based approaches. World J Psyc. 2015;5(3):286. https://doi.org/10.5498/wjp.v5.i3.286.
Weinstein RS, Krupinski EA, Doarn CR. Clinical examination component of telemedicine, Telehealth, mHealth, and connected Health Medical Practices. Med Clin North Am. 2018;102(3):533–44. https://doi.org/10.1016/j.mcna.2018.01.002.
Deslich S, Stec B, Tomblin S, Coustasse A. Telepsychiatry in the 21st Century: Transforming Healthcare with Technology. Perspec Health Inform Manag. 2013;10.
American Psychiatric Association. (Updated 5/1) Telepsychiatry and COVID-19. Retrieved August 20, 2020, from https://www.psychiatry.org/psychiatrists/practice/telepsychiatry/blog/apa-resources-on-telepsychiatry-and-covid-19.
HHS. OCR Issues Guidance on Telehealth Remote Communications Following Its Notification of Enforcement Discretion. U.S. Dep Health Human Serv. 2020. Retrieved November 10, 2021, from https://public3.pagefreezer.com/content/HHS.gov/31-12-2020T08:51/https://www.hhs.gov/about/news/2020/03/20/ocr-issues-guidance-on-telehealth-remote-communications-following-its-notification-of-enforcement-discretion.html.
Velazquez PP, Gupta G, Gupte G, Carson NJ, Venter J. Rapid Implementation of Telepsychiatry in a Safety-Net Health System During Covid-19 Using Lean. New Eng J Med Catalyst. 2020.
Chen JA, Chung W, Young SK, Tuttle MC, Collins MB, Darghouth SL, Huffman JC. COVID-19 and telepsychiatry: Early outpatient experiences and implications for the future. Gen Hosp Psychiatry. 2020;66:89–95. https://doi.org/10.1016/j.genhosppsych.2020.07.002.
Wedge D. Telepsychiatry Shows Promise As a Key Tool for ACOs: Health City 2020. Retrieved November 25, 2020, from https://www.bmc.org/healthcity/policy-and-industry/telepsychiatry-ACO-costs-engagement.
Cowan KE, McKean AJ, Gentry MT, Hilty DM. Barriers to use of telepsychiatry: Clinicians as gatekeepers. Mayo Clin Proc. 2019;94(12):2510–23. https://doi.org/10.1016/j.mayocp.2019.04.018.
Adaji A, Fortney J. Telepsychiatry in integrated care settings FOCUS. 2017;15(3):257–63. https://doi.org/10.1176/appi.focus.20170007.
U.S. Centers for Medicare & Medicaid Services. Medicare & Coronavirus. 2020. Retrieved December 01, 2020, from https://www.medicare.gov/medicare-coronavirus.
United States Drug Enforcement Administration. (2020, March 20). DEA’s response to COVID-19 [Press release]. Retrieved November 30, 2020, from https://www.dea.gov/press-releases/2020/03/20/deas-response-covid-19.
Funding
No funding was received for conducting this study. The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
This research study was conducted retrospectively from data obtained for administrative purposes. We consulted extensively with the IRB of East Carolina University who determined that our study did not need ethical approval. An IRB official waiver of approval was granted from the IRB of East Carolina University
Informed Consent
Informed consent is not required
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Muppavarapu, K., Saeed, S.A., Jones, K. et al. Study of Impact of Telehealth Use on Clinic “No Show” Rates at an Academic Practice. Psychiatr Q 93, 689–699 (2022). https://doi.org/10.1007/s11126-022-09983-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11126-022-09983-6