Abstract
This study experimentally tested risk behavior outcomes of Connecting, a low-cost, self-directed, family-based prevention program for families with youth placed in their care by state child welfare agencies. Families caring for youth aged 11 to 15 years from across Washington State were recruited and randomly assigned to either the self-directed program with supplemental support (n = 110) or a treatment as usual control condition (n = 110). Program materials included a workbook with family activities and DVDs with video clips. Over the 10-week program, participants received motivational support contacts to prompt program completion. Survey data were collected from youth and their caregivers at baseline, directly following intervention, then again at 12 and 24 months post-intervention. Intervention effects at 24-month follow-up were found to be moderated by age. Among 16- to 17-year-old youth at follow-up, there was an intervention benefit yielding reduced use of any substance (OR = 0.71, 95% CI [0.54, 0.93], p = 0.01) and nonviolent delinquency (OR = 0.73, 95% CI [0.57, 0.94], p = 0.02). There was no intervention effect among adolescents aged 13 to 15 years for any risk behaviors. This evidence suggests that the developmental timing of a self-directed, family-focused preventive intervention for youth and their caregivers in the foster care system may influence risk behaviors that typically emerge in late adolescence. ClinicalTrials.gov Identifier: NCT03157895.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There are more than 84,000 early adolescents (youth from 11 to 15 years of age) in foster care in the USA on a typical day (iFoster, 2020; U.S. Department of Health and Human Services, 2018). Evidence indicates that youth who grow up in foster care have higher incidences of substance misuse and conduct problems (Gypen et al., 2017) and early sexual activity (Latzman et al., 2019), and are at a higher risk for involvement in the juvenile criminal legal system (Orsi et al., 2018) than youth in general.
Foster Placements as Prevention Opportunities
The positive youth development framework (Catalano et al., 2004) suggests that stable and positive foster family placements provide an important opportunity for prevention of behavioral health problems such as substance use, sexual initiation, and delinquency by providing strong, protective environments for development (Gypen et al., 2017). Consistent with this overall approach, the social development model (SDM; Hawkins & Weis, 1985) integrates perspectives from social control (Hirschi, 1969), social learning (Bandura, 1977), and differential association theories (Sutherland, 1973). According to the SDM, prosocial opportunities for involvement, skills, rewards/recognitions, bonds, and healthy beliefs are hypothesized to promote prosocial behavior, while a similar process operates for antisocial opportunities and behavior. Interventions based on this model have been shown to reduce substance use, sexual risk, and delinquent behaviors (Catalano et al., 2021; Haggerty et al., 2007). Foster and relative caregivers need effective family-focused interventions (Barnett et al., 2018; Storer et al., 2014) to help them provide opportunities for positive social development to the teens in their care. Licensed caregivers typically receive preservice training; however, it is questionable that this training adequately prepares them to be emotionally responsive, open to communication, and able to provide for the needs of adolescent youth in their care (Barnett et al., 2018; Feltner et al., 2021). Relatives taking in youth receive little to no training, further limiting their ability to provide social-emotional support for kin in their care. These deficits—in addition to exposure to adverse experiences leading to foster placement—may contribute to elevated health risk behaviors of adolescents in foster care (Casey Family Programs, 2018).
Potential Moderators of Intervention Efficacy
There are individual and environmental factors that may moderate the impact of family-focused interventions, and understanding those factors can lead to improvements in intervention materials, timing, and population targets. One such moderator is developmental timing. Family-focused interventions designed for adolescents often target a range of ages which span early to middle adolescence. Targeted outcomes such as substance use or sexual initiation grow in prevalence over this range, so it is typical to see “sleeper effects” of early prevention interventions—for example, those delivered in the 11- to 13-year age range—not demonstrating a measurable impact until late adolescence (Haggerty et al., 2007; Spoth et al., 2004).
Recently, tests of intervention efficacy have included baseline risk as a potential moderator of program impact (Brincks et al., 2021). In the case of universal interventions for families of teens in foster care, intervention alone may not be enough to overcome the risk already incurred before the youth and caregiver engage in the intervention. This could be especially true of youth already exposed to multiple transitions with many different caregivers, which is a known risk factor for substance use and other risk behaviors (Gypen et al., 2017).
The dose of an intervention has also been shown to be an important factor in intervention outcomes (Brody et al., 2006). Dosage effects are commonly explored in intention-to-treat prevention programs to help identify the benchmark for adherence that will yield an intervention benefit. Families with lower adherence to the intervention—generally less than 60%—likely experience fewer benefits (Baggett et al., 2017). This is concerning, as many families with the highest risk for substandard caregiving behaviors are also the likeliest to engage inconsistently in the program or drop out altogether (Haggerty et al., 2002).
Prevention programs in general may or may not work in the context of specific historical conditions in the larger society. The recent extraordinary events related to the COVID-19 pandemic affected every family in the USA, including those with foster children. Interventions designed to improve communication and bonding between teens and their caregivers may have stronger or weaker effects in the context of school closings and statewide shelter-in-place requirements.
Adapting and Testing a Tailored Approach
Effective caregiver training can improve outcomes for children in care (Cooley & Petren, 2011; Feltner et al., 2021; Price et al., 2015). However, there is a dearth of evidence-based parenting programs tailored to teens in foster care and their caregivers. The programs that do exist typically focus on reducing existing problem behaviors rather than prevention, and target youth with the highest level of need (Barth et al., 2005). Although effective models of parenting programs for the general population of parents and their teens exist (Van Ryzin et al., 2016), they do not consider the unique situation of foster families.
To address the need for parenting programs tailored to support the needs of adolescents in foster care that are easy to use, affordable, and evidence based, we developed Connecting. Connecting was adapted for youth in foster care and their caregivers (Barkan et al., 2014; Haggerty et al., 2016; Storer et al., 2012), using the ADAPT-ITT framework (Wingood & DiClemente, 2008), from an existing universal parenting program with evidence for preventing risky behaviors in adolescence, Staying Connected with Your Teen (STC; Haggerty et al., 2007).
The current study is a randomized controlled trial of the Connecting program in which we examine program effects on health risk behaviors related to substance use, delinquency, and sexual activity at 12-month follow-up (12-FU) and 24-month follow-up (24-FU). Studies of the Connecting program—including a small, randomized, waitlist control pilot study (Haggerty et al., 2016)—and posttest results from this current randomized trial (Haggerty et al. (2021) have demonstrated a positive impact on preventing substance use and other risky behaviors. Building on these promising results, we hypothesized that at 24-FU, adolescents in the Connecting intervention would report lower substance use initiation; prevalence of alcohol, tobacco, marijuana, and other drug use; and less delinquency and sexual activity. Additionally, consistent with other interventions, we expected to see a dose–response relationship, with those completing more of the intervention demonstrating greater preventive effects at 24-FU.
Methods
Program Description
The self-directed, self-paced Connecting program is theoretically guided by the Social Development Strategy (Haggerty & McCowan, 2018) and is intended to be a prevention program for youth ages 11 to 15 years in foster care and their caregivers. The program features a workbook with easy-to-follow activities for caregivers and youth, designed to provide youth with opportunities to contribute to their foster families, acquire the skills needed to take advantage of these opportunities, increase caregiver supervision, reduce conflict, and promote bonding through reward and recognition strategies. The Connecting adaptation included the original STC workbook and DVD, additional activities to promote caregiver-youth bonding, specific resources for foster parents, and special attention to the development of foster youths’ independent living skills (Barkan et al., 2014; Storer et al., 2012). Training materials were mailed to each family assigned to the treatment condition, with the suggestion that families complete one chapter per week over 10 weeks. A family consultant trained in motivational interviewing checked in weekly with families to record completed activities, motivate families to use the materials, and help them problem solve any implementation challenges (Haggerty et al., 2021). No financial incentive was provided to caregivers or youth for program participation; however, licensed caregivers who completed the program could request a certificate with the total number of hours spent on the program (on average about 8 h) which counted towards the training requirements of caregivers in Washington State (36 h of training over 3 years).
Recruitment, Procedures, and Data Collection
Youth/caregiver dyads were recruited from November 2016 through April 2018. The study has been registered in ClinicalTrials.gov; all study procedures were approved by the Washington State Institutional Review Board. The research team collaborated with the Washington State Department of Children, Youth, and Families (DCYF) to select families for recruitment. Eligibility criteria included youth between the ages of 11 and 15 years whose placement in foster care was 30 days or longer, placement with a licensed or unlicensed relative caregiver or a licensed foster caregiver where the placement was expected to last for at least 6 months, and the ability of both youth and caregivers to speak and be literate in English to use the Connecting manual and respond to survey questions. Youth included in the study were not known to be regularly using drugs or alcohol in the last 30 days, and did not have any past involvement in the criminal justice system. Youth in group-home and behavioral rehabilitation services placements were excluded, due to the study’s focus on primary prevention.
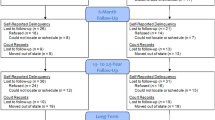
Case data were provided by DCYF in several waves and were initially screened by research staff for eligibility. To manage the flow of screening, opt-out, and recruitment, 549 cases were randomly selected from the first wave. Thereafter, all new cases were screened for eligibility. If a case passed this screen, both foster caregivers and biological parents (if youth was not legally free) were mailed opt-out letters. Families who did not request to opt out were sent a recruitment letter, fact sheet, and consent/assent forms, followed by a phone call within 2 weeks. When a family expressed interest in participating, their social worker was contacted and asked to provide written consent. One hundred and six (98 caregivers and 8 biological parents) opted out and 36 families were not consented by social workers—usually because the placement had become less stable—leaving 751 families who were entered into active recruitment. Three eligible families self-referred and were recruited (see Fig. 1).
Data were collected at four time points: baseline, posttest, 12-FU, and 24-FU. During enrollment, 220 caregivers/youth completed separate online or phone baseline surveys. After the baseline survey was completed, caregivers and youth received a $40 and $20 incentive, respectively, and then caregiver/teen dyads were randomly assigned to either the treatment (n = 110) or treatment as usual control (n = 110) group. Families were randomized in blocks to achieve geographic representation across the three DCYF administrative regions in Washington State. At the end of 3 months, both caregivers and youth in the treatment and control conditions completed a posttest survey, receiving an incentive of $30. Nearly 85% of dyads completed the posttest survey (88.6% of caregivers and 89.5% of youth). During the 3-month study period, 20 enrolled youth changed placements (13 treatment and 7 control). When possible, follow-up was conducted with youth and caregivers in their new placements. Follow-up surveys were administered to caregiver-youth dyads at 12-FU and again at 24-FU.
Sample and Program Completion
The average age of the foster youth was 13 years at baseline; gender was balanced (54% female); youth represented diverse race/ethnicity (30% Hispanic, 15% Black, 12% Native, 9% Asian). The number of placements each youth had been in prior to the study varied from 1 to 17 (M = 3.28, SD = 2.58). Placement type at baseline varied, with 46% placed with nonrelative licensed caregivers, 40% living with relatives, and the remainder with nonrelated close adults who were not licensed (14%). Ten percent of caregivers had been parenting foster, adoptive, or biological children for 5 or fewer years and some had over 40 years of experience (median = 23 years). Of the 110 families assigned to the treatment condition, 86 (78%) completed some of the programs, while 58 (52%) completed 60% or more of the 94 program tasks. See Haggerty et al. (2021) for further details on implementation and high program satisfaction. There were no significant differences in baseline measures of outcomes (see Table 1).
Measures
Youth-Report Risk Behavior Outcomes
Substance Use Reporting
Substance use classes included tobacco, alcohol, marijuana, and other drugs. For all substance classes, the baseline survey measured lifetime use (i.e., “Have you ever used marijuana?”) as a yes/no item. The posttest survey measured the number of occasions of past-30-day use, while the 12-FU and 24-FU surveys measured the number of occasions of past-year use. For tobacco, all time points included cigarettes and smokeless tobacco items, while the 24-FU also included an item for e-cigarettes. For alcohol, baseline queried lifetime use of any alcoholic beverages; for posttest through 24-FU, a single item asked about occasions of use. For marijuana for all time points, a single item queried occasions of marijuana use. For other drugs, one item queried the number of occasions of prescription drug use without a prescription (or more than was prescribed), and a second item asked about any use of other drugs or medications to get high (yes/no item). Response options for substance use items were ordinal (i.e., for alcohol: 0 occasions; 1 to 2 occasions; 3 or more occasions, etc.). Minimal reported use occasions across substances yielded long tails in the ordinal distributions. Thus, binarized scores were calculated for each tobacco, alcohol, marijuana, and other drugs: no use = 0 and any use at all = 1. For substance classes with multiple items (i.e., for tobacco: cigarettes, smokeless tobacco, and e-cigarettes), endorsement of any use on any item yielded a code of 1. An additional “any use” variable was created at each time point to examine overall substance use. The “any use” variable was scored by assigning a 0 to youth who reported no use of any substances at that time point and a 1 to youth who reported any use across all substances.
Substance Use Initiation
Variables for substance use initiation were calculated for 12-FU and 24-FU, and they were derived from the substance use binarized scores described above for each substance class. Because the intervention target was a delay in initiation of substance use, all youth who reported any baseline (lifetime) use for a specific substance—and thus no delay—were excluded from analyses for that substance. For the remaining youth who were substance-naïve at baseline, 12-FU prevalence scores were calculated by assigning a 0 if no use was reported, or a 1 if any use was reported, across posttest and 12-FU. The same scoring logic was extended to the 24-FU initiation variables.
Substance Use Prevalence
Prevalence rates were examined by using the binarized substance use scores described above for tobacco, alcohol, marijuana, other drugs, and any use at baseline, 12-FU, and 24-FU.
Delinquent Behavior Prevalence
Youth reported on nonviolent and violent delinquent behavior. Nonviolent delinquent behavior was measured with 11 yes/no items, including self-report of break-ins, stealing, destruction of property, and running away. Violent delinquent behavior was measured with six yes/no items, including self-report of throwing objects at or hitting others, starting fights, and carrying a handgun. Questions referred to lifetime behavior at baseline, and past-year behavior at 12-FU and 24-FU. Prevalence scores were calculated for nonviolent and violent behavior separately. For nonviolent delinquency, endorsement of yes for any of the 11 items yielded a code of 1 (or 0 for no delinquent behaviors). For violent delinquency, the same scoring logic was applied with the six items. Prevalence scores were calculated for baseline, 12-FU, and 24-FU.
Sexual Behavior Prevalence
Prevalence scores were created for 12-FU and 24-FU youth-reported sexual behavior. At each time point, one yes/no (coded as 1/0) item was used: “In the past year have you had sex including oral, anal, or vaginal sex?”.
Covariates and Moderating Variables
Lifetime Placement Changes
Lifetime placement changes was measured at baseline via youth report of the total number of times they had changed household placements prior to the start of the study.
Posttest Placement Changes
Posttest placement changes was measured via youth report of the number of times they had changed household placements over the past year, queried during 12-FU and again at 24-FU. The 24-FU scores were summed across 12-FU and 24-FU. Scores were then binarized, with zero or one placement change indicating higher placement stability, and two or more changes indicating lower placement stability. The rationale is that one placement change in some cases is just as good as (or better than) none, when the nature of the change is a return to a parent or close relative, an adoption, or another more permanent placement (Semanchin Jones et al., 2016).
COVID-19 Survey Conditions
Of the youth participants who completed the 24-FU survey, 60 control youth (68%) and 70 Connecting youth (83%) completed the survey either before or within 1 month of the Washington State COVID-19 shelter-in-place order. Significantly more youth from the Connecting vs. control group completed the survey pre-COVID (χ2 = 5.35, p = 0.02). Given the hypothesized mechanisms in Connecting (e.g., youth-caregiver bonding), there was a possibility that household disruptions from the shelter-in-place order could impact the integrity of the intervention. Given the retrospective nature of the survey, up to 1 month within an active shelter-in-place order was considered an appropriate time frame before COVID-related behavior changes would be reflected in youth reports.
Dosage Effects
The dosage variable was a binarized score representing program completion of less than 60% (coded 0) or greater than 60% (coded 1) and was restricted to the Connecting group (n = 110). To derive this score, program completion was measured via a caregiver report from the posttest survey. If caregivers reported completing “quite a bit,” “most,” or “all” of three types of tasks (reading the workbook, doing the activities, and watching the Staying Connected and Youth Stories DVDs), they were coded as a 1. For caregivers who did not provide data on the posttest survey, the dosage was coded as a 1 if the family consultant reported they had done at least 58 of the 94 tasks on the checklist (61%). Because caregiver and family consultant reports were on different scales, binarizing the dosage variable at scale thresholds representing ~ 60% completion allowed for standardization of reporting from the two informants.
Data Analysis
Data were analyzed in SPSS and R. Intention-to-treat analyses were conducted on teen-reported risk behavior outcomes related to substance use, delinquency, and sexual activity. Analyses included 12-FU and 24-FU outcomes.
Handling Missing Data
Survey nonresponse included 46 youth at 12-FU (21% of sample; n = 26 Connecting, n = 20 control) and 45 youth at 24-FU (20% of sample; n = 24 Connecting, n = 21 control). There were no differences in missingness by treatment condition at 12-FU (χ2 = 0.99, p = 0.32) or 24-FU (χ2 = 0.25, p = 0.62) and no significant predictors of missingness among planned covariates with complete baseline data, indicating a reasonable likelihood the data are at least missing at random. Missing data were handled using multivariate imputation by chained equations with 30 imputations and maximum of 10 iterations via the mice function in R (van Buuren & Groothuis-Oudshoorn, 2011). A separate set of auxiliary variables was added to the multiple imputation models for each risk outcome category (substance use initiation, substance use prevalence, delinquent behavior, sexual behavior) to improve imputation model fit.
Main Effect Models
One youth participant at 12-FU and three youth participants at 24-FU were dropped from all statistical analyses for reporting dishonest answers (“I was not honest at all”). This resulted in pre-imputation sample sizes of 173 youth at 12-FU (84 Connecting, 89 control) and 172 youth at 24-FU (84 Connecting, 88 control). Binominal logistic regression models using a logit link were conducted separately to examine 13 risk behavior outcomes across four categories at each of the two time points (12-FU, 24-FU): substance use initiation and substance use prevalence (any substance, tobacco, alcohol, marijuana, other drugs); delinquent behavior prevalence (nonviolent, violent); and sexual behavior prevalence. Odds ratios testing the intervention effect for each outcome were calculated as unadjusted for planned covariates, as well as adjusted. Covariates in all models included age (baseline) and posttest number of placement changes (12-FU or 24-FU), as well as dummy-coded variables for White race/ethnicity (baseline), Hispanic race/ethnicity (baseline), and male gender (baseline). Past-year substance use prevalence and delinquent behavior models controlled for baseline prevalence of the specific risk behavior (e.g., tobacco use prevalence controlled for baseline tobacco use). Sexual behavior did not control for baseline sexual behavior, given the high rate of nonconsensual sexual behavior generally reported among younger adolescents in this population (Euser et al., 2013), which evokes concern about the validity of baseline reports of sexual behavior as an indicator of risky sexual decision making.
Global Test Statistic
In addition to assessing separate behavior outcomes, a global test statistic (GTS; Pocock et al., 1987) was used to analyze the overall effect of Connecting across prevalence outcomes at 12-FU and again at 24-FU. Because the goal of Connecting was not to target specific behaviors but to prevent youth risk outcomes generally, the GTS was an appropriate test for measuring whether Connecting was shifting outcomes in a favorable direction. The GTS calculates the average t value across the estimated intervention effect for each behavior outcome and adjusts it for the sample size, number of outcomes, correlations among the outcomes, and the increased risk of type I error resulting from multiple tests. The GTS in this study combined all substance use prevalence outcomes, nonviolent and violent delinquency, and sexual behavior outcomes.
Subgroup Analyses
Subgroup analyses were conducted for the 13 risk behavior outcomes at 12-FU and 24-FU. One set of subgroup analyses examined age (baseline) as an effect modifier. Additional analyses included a proxy measure of baseline risk: lifetime placement changes (baseline).
Age
For subgroup analyses focused on age, a treatment condition x age interaction term was added to the main effect models described in the Main Effect Models section. Furthermore, planned subgroup analyses were conducted in each of two age groups: 13–15 years and 16–17 years at 24-FU. This age split roughly corresponds to middle school/early high school (13–15 years) and later high school (16–17 years), with later high school representing expanded opportunities to engage in risk behaviors, as well as for the intervention to confer a noticeable benefit consistent with findings in the RCT of the original program (Haggerty et al., 2007).
Lifetime Placement Changes
For subgroup analyses focused on lifetime placement changes, a main effect term for lifetime placement changes as well as a treatment condition x lifetime placement changes interaction term was added to the main effect models. As with age, subgroup analyses were planned a priori, with 0–2 lifetime placement changes representing a “lower” baseline risk subgroup and > 2 placement changes representing “higher” baseline risk.
COVID-19 Restricted Sample Analyses
The main effect and GTS models for the risk behavior outcomes were repeated using only the 76% of youth who completed the 24-FU survey before or within 1 month of the COVID shelter-in-place order (Control: n = 60; Connecting: n = 70). As with the full-sample analyses, multiple imputation was used to estimate parameters for the 45 additional youth missing data from 24-FU. Subgroup analyses for age and baseline risk were not repeated in this reduced sample due to small sample size. Prevalence rates for behavior outcomes did not differ between youth who completed the 24-FU survey before vs. after the COVID shelter-in-place order.
Dosage Effects
Dosage effects at 12-FU and 24-FU were assessed within the Connecting intervention group. We calculated the unadjusted odds ratios for substance use prevalence (any use, tobacco, alcohol, marijuana, and other drugs), delinquent behavior (nonviolent and violent), and sexual behavior. Substance use initiation outcomes were not included in analyses, given small sample sizes after removing youth with baseline use.
Results
24-FU Full Sample: Main Effects
There were no intervention effects at 24-FU for any subclasses of substance use initiation, substance use, delinquent behavior, or sexual behavior (Table 2). Likewise, the GTS showed no intervention effect on overall risk behavior.
24-FU Full Sample: Subgroup Analyses
Youth Age (Baseline)
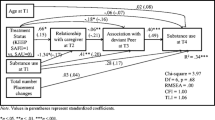
An intervention effect on several risk behaviors at 24-FU was moderated by age. Among 16- to 17-year-old youth at 24-FU, there was an intervention benefit yielding reduced use of any substance (OR = 0.71, 95% CI [0.54, 0.93], p = 0.01), marginally reduced use of alcohol (OR = 0.81, 95% CI [0.64, 1.03], p = 0.08), and reduced nonviolent delinquency (OR = 0.73, 95% CI [0.57, 0.94], p = 0.02). There were no intervention effects in adolescents aged 13 to 15 years.
Lifetime Placement Changes (Baseline)
No intervention effects on risk behaviors at 24-FU were moderated by lifetime history of placement changes.
24-FU COVID-19 Restricted Sample: Main Effects
There was an intervention effect at 24-FU showing reduced use of any substance in the Connecting group (OR = 0.83, 95% CI [0.70, 0.98], p = 0.03). No other risk behavior categories yielded significant intervention effects. The GTS showed an intervention benefit when combining risk behavior categories (t = − 1.76, p = 0.04).
24-FU Dosage Effects
Youth from families who completed at least 60% of the Connecting program showed significantly lower prevalence rates for tobacco, alcohol, marijuana, other drugs, nonviolent delinquency, and violent delinquency (odds ratios ranged from 0.72 to 0.82) compared to those who were assigned to the intervention but completed less than 60% of the program.
12-FU Main Effects, Subgroup Analyses, and Dosage Effects
Although behavior outcomes at 12-FU were trending in a favorable direction, statistical models revealed no significant main, GTS, or subgroup intervention effects when comparing Connecting youth with control youth. Strong dosage effects were observed, with lower use of tobacco, alcohol, and marijuana, as well as lower nonviolent and violent delinquency and lower sexual behavior prevalence in the higher dosage group (odds ratios ranged from 0.69 to 0.92).
Discussion
Given the lack of evidence-based prevention programs to address higher levels of risk behaviors among teens in foster care compared to teens in general, it is important to develop and test interventions specifically designed to support caregivers and youth in foster care that address the risk and protective factors associated with health risking behaviors such as substance use, delinquency, and adolescent sexual activity. Consistent with the social development model and earlier findings (Haggerty et al., 2016, 2021), we hypothesized that Connecting would lead to a reduction in the youths’ involvement in high-risk behaviors. To that end, we tested the efficacy of a family-focused prevention program adapted from a universal prevention program based on the social development model which has been previously shown to reduce substance use, violent delinquency, and sexual initiation among adolescents.
Results of intention-to-treat analyses did not reveal overall program efficacy. Despite the overall lack of findings, we wanted to more deeply explore why we might not have detected predicted outcomes, particularly because the evidence for the original program (Staying Connected with Your Teen) neither includes youth as young as 11 years, youth in foster care, nor the challenges of a shelter-in-place order. Several factors were considered as possible moderators of intervention effects: developmental timing, baseline placement instability, and historical events (restrictions to reduce transmission of COVID-19). In subgroup analyses, positive intervention effects were observed for older (16–17 years old at 24-FU), but not younger teens (13–15 years old at 24-FU). This age pattern aligns with the social development model’s hypothesis that family processes experienced in the middle school years—such as caregiver bonding in this study—are especially influential in facilitating prosocial involvement and diverting youth from antisocial involvement in the high school years (Hawkins & Weis, 1985).
Consistent with other studies that have demonstrated delayed prevention effects, interventions to prevent adolescent risk behaviors in foster youth may need to be timed so they are more proximal to the opportunities for these behaviors. Many risk behaviors see sharp increases between 15 to 17 years of age (Johnston et al., 2022), making the mid-teen years a critical period for programming aimed at diverting youth from these behaviors. Given this sample was selected based on having not already demonstrated high levels of these risk behaviors (though they are in a high-risk population), effects may grow stronger over time. The overall prevention benefit of Connecting appeared to be trending in a positive direction, with prevalence rates indicating emergent intervention benefits by 12-FU and stronger benefits by 24-FU. The data point to a latency period, whereby the maximal prevention efficacy of Connecting may be observed months or years beyond the 24-FU window. Future studies of Connecting with a longer longitudinal design are needed to test this hypothesis.
Another possibility is that family-based interventions like Connecting, delivered in early adolescence, do provide prosocial opportunities for youth through strengthening skills, recognition, and bonding as outlined in the social development model that could yield preventive effects even for youth in foster care, but those effects cannot be observed until those youth enter late adolescence, giving them more opportunities for risky behavior. We might expect that small effects in changing the patterns of the foster caregiver dynamic might have reciprocal effects on the youth in their care and that bonding and connecting will strengthen over time. Such “sleeper” effects for prevention programs delivered during early adolescence are not uncommon (Spoth et al., 2001; van Aar et al., 2017). van Aar et al. (2017) suggest a number of factors that contribute to such sleeper effects that might be relevant to our study, such as caregivers needing more time to master practices or contextual challenges to implement the practices in the midst of multiple stressors (e.g., COVID-19, baseline placement instability, etc., all affecting whether caregivers could complete the program) (Spoth et al., 2001; van Aar et al., 2017).
The historic events related to the COVID-19 pandemic proved to be a disruption for teens in our study. Data collection procedures were not affected because data were collected online or over the phone. However, life changed dramatically over the course of the field period, and youth who responded to the survey before COVID-19 were in a very different situation than those who responded after the onset of school closures and shelter-in-place orders. The results of analyses conducted on the subsample who completed data collection under “normal” conditions suggest that program impact on substance use may have been stronger than indicated by full-sample intention-to-treat analyses. Specifically, the GTS was statistically significant and indicated that the overall prevention benefit of Connecting was trending in a positive direction by 24-FU. The stronger effects in the pre-shelter-in-place sample are not explained by higher prevalence rates during shelter-in-place, as these rates did not differ between youth who completed the 24-FU survey pre- vs. post- shelter in place. In fact, there was an overall positive direction of effect in the pre-COVID sample and iatrogenic effects in the pandemic restrictions sample. This suggests COVID-19 may have disrupted the intervention’s efficacy and masked emerging benefits that were observed prior to COVID.
Examination of the dosage of the intervention at 12-FU and 24-FU did reveal that caregiver/youth dyads who had completed 60% or more of the intervention were significantly less likely to show youth-reported engagement in a number of risk behaviors, including use of tobacco, alcohol, marijuana, and other drugs, as well as nonviolent delinquency and violent delinquency. This trend suggests the intervention benefits are driven by consistent engagement in the program activities. With only 52% of the caregiver/youth dyads completing at least 60% of the program, future efforts should be directed at increasing program adherence. Program benefits may have been dampened by differential attrition, whereby the dyads least likely to complete the program are precisely the ones most likely to benefit (Haggerty et al., 2002). The dosage effects should be interpreted with caution, as the grouping strategy into low and high dosage violates random assignment and also shows evidence of differential attrition, with significantly fewer youth in the low-dosage group completing the 24-FU survey.
Given the lack of an overall program effect, we have considered the recommendations of Axford et al. (2020) to facilitate our learning process from these results. Upon reflection, our study development process was in keeping with one of their recommendations in that we employed a “human-centered” co-design with input from key stakeholders. This resulted in a decision to focus the intervention on children from 11–15 years of age. Prior to this adaptation for child welfare-involved youth and their caregivers, the original study focused on eighth-grade youth who were on average 13.65 years of age (Haggerty et al., 2006), where we did find significant findings after 24 months of follow-up (Haggerty et al., 2007).
Limitations
While, as noted above, we were responsive to stakeholder input and focused on a younger age group, we neglected to stratify and sufficiently power, in particular, the older age group in our sample. It is worth noting that this older age subgroup, for whom we did find significant effects, is the same age (16–17 years) as those from the study of the original program where we also saw significant effects. In retrospect, examination of the effects for this older age group should have been our primary a priori hypothesis. The study would have been better served had we stratified and identified a separate hypothesis for the younger age group.
There are several other limitations to this study. The study was a low-risk sample in a high-risk population. Because the focus was on early prevention, young people who were already engaged in problem behaviors were excluded from the study. Also, the sample was not designed to power tests of moderation based on youth age, number of previous placements, or historic school closures and restrictions in social interactions. This limits the interpretation of statistical tests as well as generalizability of these results. Although not part of the design, naturally occurring variation in age and number of placements did allow for tests of moderation, albeit with limited statistical power. The events related to COVID-19 were dramatic enough that consideration of their impact on program efficacy had to be made; however, subsample size pre-pandemic restrictions did not allow for a formal moderation test.
Conclusions/Implications
The evidence presented in this study is consistent with other research demonstrating a “sleeper” or delayed prevention effect. This suggests that the developmental timing of a self-directed, family-focused preventive intervention for caregivers of youth in foster care may have a stronger impact on risk behaviors that typically emerge in later adolescence as exposure to higher risks becomes more prevalent. Our previous work (Haggerty et al., 2016) has demonstrated that about half the caregivers refer back to the program materials over the course of time, suggesting ongoing use of the materials may be useful as environments become more risky. Thus, the availability of relevant, self-directed parenting guidance for foster caregivers caring for teens may be beneficial for reducing overall later risk-taking behaviors. The results fall short of the Society for Prevention Research standards of evidence that require, “In testing main effects, the analyses must include all cases assigned to treatment and control conditions” (Gottfredson et al., 2015, p. 898). Although we were unable to detect significant main effects, the results are promising and highlight the need to adapt evidence-based parenting interventions for foster caregivers.
References
Axford, N., Berry, V., Lloyd, J., Hobbs, T., & Wyatt, K. (2020). Promoting learning from null or negative results in prevention science trials. Prevention Science. Advance online publication. https://doi.org/10.1007/s11121-020-01140-4
Baggett, K., Davis, B., Feil, E., Sheeber, L., Landry, S., Leve, C., & Johnson, U. (2017). A randomized controlled trial examination of a remote parenting intervention: Engagement and effects on parenting behavior and child abuse potential. Child Maltreatment, 22, 315–323.
Bandura, A. (1977). Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review, 84, 191–215.
Barkan, S. E., Salazar, A. M., Estep, K., Mattos, L. M., Eichenlaub, C., & Haggerty, K. P. (2014). Adapting an evidence based parenting program for child welfare involved teens and their caregivers. Children and Youth Services Review, 41, 53–61.
Barnett, E. R., Jankowski, M. K., Butcher, R. L., Meister, C., Parton, R. R., & Drake, R. E. (2018). Foster and adoptive parent perspectives on needs and services: A mixed methods study. The Journal of Behavioral Health Services & Research, 45, 74–89.
Barth, R. P., Crea, T. M., John, K., Thoburn, J., & Quinton, D. (2005). Beyond attachment theory and therapy: Towards sensitive and evidence-based interventions with foster and adoptive families in distress. Child & Family Social Work, 10, 257–268.
Brincks, A., Perrino, T., Howe, G., Estrada, Y., Robles, N., & Prado, G. (2021). Familias Unidas prevents youth internalizing symptoms: A baseline target moderated mediation (BTMM) study. Prevention Science. Advance online publication. https://doi.org/10.1007/s11121-021-01247-2
Brody, G. H., Murry, V. M., Chen, Y.-F., Kogan, S. M., & Brown, A. C. (2006). Effects of family risk factors on dosage and efficacy of a family-centered preventive intervention for rural African Americans. Prevention Science, 7, 281–291.
Casey Family Programs. (2018). What impacts placement stability? Retrieved from https://www.casey.org/placement-stability-impacts/
Catalano, R. F., Berglund, M. L., Ryan, J. A. M., Lonczak, H. S., & Hawkins, J. D. (2004). Positive youth development in the United States: Research findings on evaluations of positive youth development programs. The Annals of the American Academy of Political and Social Science, 591, 98–124.
Catalano, R. F., Hawkins, J. D., Kosterman, R., Bailey, J. A., Oesterle, S., Cambron, C., & Farrington, D. P. (2021). Applying the social development model in middle childhood to promote healthy development: Effects from primary school through the 30s and across generations. Journal of Developmental and Life-Course Criminology, 7, 66–86.
Cooley, M. E., & Petren, R. E. (2011). Foster parent perceptions of competency: Implications for foster parent training. Children and Youth Services Review, 33, 1968–1974.
Euser, S., Alink, L. R. A., Tharner, A., van Ijzendoorn, M. H., & Bakermans-Kranenburg, M. J. (2013). The prevalence of child sexual abuse in out-of-home care: A comparison between abuse in residential and in foster care. Child Maltreatment, 18, 221–231.
Feltner, A., Day, A., Vanderwill, L., Fontaine, E., & Cohick, S. (2021). Equipping resource parents with the knowledge and attitudes to effectively parent teens: Results from the CORE Teen training program. Children and Youth Services Review, 121, 105835.
Gottfredson, D. C., Cook, T. D., Gardner, F. E. M., Gorman-Smith, D., Howe, G. W., Sandler, I. N., & Zafft, K. M. (2015). Standards of evidence for efficacy, effectiveness, and scale-up research in prevention science: Next generation. Prevention Science, 16, 893–926.
Gypen, L., Vanderfaeillie, J., De Maeyer, S., Belenger, L., & Van Holen, F. (2017). Outcomes of children who grew up in foster care: Systematic-review. Children and Youth Services Review, 76, 74–83.
Haggerty, K. P., Barkan, S. E., Skinner, M. L., & Hanson, K. (2021). Proximal outcomes of Connecting, an evidence-based, family-focused prevention program for caregivers of adolescents in foster care. Children and Youth Services Review, 126, 106009.
Haggerty, K. P., Barkan, S. E., Skinner, M. L., Packard, W. B., & Cole, J. J. (2016). Feasibility of Connecting, a substance-abuse prevention program for foster teens and their caregivers. Journal of the Society for Social Work and Research, 7, 639–659.
Haggerty, K. P., Fleming, C. B., Lonczak, H. S., Oxford, M. L., Harachi, T. W., & Catalano, R. F. (2002). Predictors of participation in parenting workshops. The Journal of Primary Prevention, 22, 375–387.
Haggerty, K. P., MacKenzie, E. P., Skinner, M. L., Harachi, T. W., & Catalano, R. F. (2006). Participation in “Parents Who Care”: Predicting program initiation and exposure in two different program formats. The Journal of Primary Prevention, 27, 47–65.
Haggerty, K. P., & McCowan, K. J. (2018). Using the social development strategy to unleash the power of prevention. Journal of the Society for Social Work and Research, 9, 741–763.
Haggerty, K. P., Skinner, M. L., MacKenzie, E. P., & Catalano, R. F. (2007). A randomized trial of Parents Who Care: Effects on key outcomes at 24-month follow-up. Prevention Science, 8, 249–260.
Hawkins, J. D., & Weis, J. G. (1985). The social development model: An integrated approach to delinquency prevention. The Journal of Primary Prevention, 6, 73–97.
Hirschi, T. (1969). Causes of delinquency. University of California Press.
iFoster. (2020). 6 quick statistics on the current state of foster care. Retrieved from https://www.ifoster.org/6-quick-statistics-on-the-current-state-of-foster-care/
Johnston, L. D., Miech, R., O’Malley, P. M., Bachman, J. G., Schulenberg, J. E., & Patrick, M. E. (2022). Monitoring the Future national survey results on drug use, 1975–2021: Overview, key findings on adolescent drug use. Institute for Social Research.
Latzman, N. E., Gibbs, D. A., Feinberg, R., Kluckman, M. N., & Aboul-Hosn, S. (2019). Human trafficking victimization among youth who run away from foster care. Children and Youth Services Review, 98, 113–124.
Orsi, R., Lee, C., Winokur, M., & Pearson, A. (2018). Who’s been served and how?: Permanency outcomes for children and youth involved in child welfare and youth corrections. Youth Violence and Juvenile Justice, 16, 3–17.
Pocock, S. J., Geller, N. L., & Tsiatis, A. A. (1987). The analysis of multiple endpoints in clinical trials. Biometrics, 43, 487–498.
Price, J. M., Roesch, S., Walsh, N. E., & Landsverk, J. (2015). Effects of the KEEP foster parent intervention on child and sibling behavior problems and parental stress during a randomized implementation trial. Prevention Science, 16, 685–695.
Semanchin Jones, A., Rittner, B., & Affronti, M. (2016). Foster parent strategies to support the functional adaptation of foster youth. Journal of Public Child Welfare, 10, 255–273.
Spoth, R., Redmond, C., Shin, C., & Azevedo, K. (2004). Brief family intervention effects on adolescent substance initiation: School-level growth curve analyses 6 years following baseline. Journal of Consulting and Clinical Psychology, 72, 535–542.
Spoth, R. L., Redmond, C., & Shin, C. (2001). Randomized trial of brief family interventions for general populations: Adolescent substance use outcomes 4 years following baseline. Journal of Consulting and Clinical Psychology, 69, 627–642.
Storer, H. L., Barkan, S. E., Sherman, E. L., Haggerty, K. P., & Mattos, L. M. (2012). Promoting relationship building and connection: Adapting an evidence-based parenting program for families involved in the child welfare system. Children and Youth Services Review, 34, 1853–1861.
Storer, H. L., Barkan, S. E., Stenhouse, L. L., Eichenlaub, C., Mallillin, A., & Haggerty, K. P. (2014). In search of connection: The foster youth and caregiver relationship. Children and Youth Services Review, 42, 110–117.
Sutherland, E. H. (1973). Development of the theory [Private paper published posthumously]. In K. Schuessler (Ed.), Edwin Sutherland on analyzing crime (pp. 13–29). University of Chicago Press.
U.S. Department of Health and Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children’s Bureau. (2018). The AFCARS Report: Preliminary FY 2017 estimates as of August 2018, No. 25. Retrieved from https://www.acf.hhs.gov/sites/default/files/documents/cb/afcarsreport25.pdf
van Aar, J., Leijten, P., Orobio de Castro, B., & Overbeek, G. (2017). Sustained, fade-out or sleeper effects? A systematic review and meta-analysis of parenting interventions for disruptive child behavior. Clinical Psychology Review, 51, 153–163.
van Buuren, S., & Groothuis-Oudshoorn, C. G. M. (2011). mice: Multivariate imputation by chained equations in R. Journal of Statistical Software, 45, 1–67.
Van Ryzin, M. J., Kumpfer, K. L., Fosco, G. M., & Greenberg, M. T. (2016). Family-based prevention programs for children and adolescents: Theory, research, and large-scale dissemination. Psychology Press.
Wingood, G. M., & DiClemente, R. J. (2008). The ADAPT-ITT model: A novel method of adapting evidence-based HIV interventions. JAIDS Journal of Acquired Immune Deficiency Syndromes, 47, S40–S46.
Acknowledgements
The authors wish to acknowledge the Washington State Department of Children, Youth, and Families for its collaboration in making this work possible; the Family Support Specialists who supported participants in the self-directed program (Janice Cole, Carol Ashley, Carrie St. John, and Lauren Collins); the data collection staff (Ashton Gatsby, Carly Lauck, Deborah Cohen, Tasha Cummings, Ariel Li, Calla Natzke, Casey Chandler, and Barbara Floyd); and Jessica Colito who managed all of the moving parts.
Funding
The authors received support from the National Institute on Drug Abuse (NIDA R01DA038095). The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the funding agency.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All research protocols involving human participants were approved by the University of Washington Institutional Review Board and were in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments.
Informed Consent
Informed consent was obtained from all study participants.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Haggerty, K.P., Barkan, S.E., Caouette, J.D. et al. Two-Year Risk Behavior Outcomes from Connecting, a Prevention Program for Caregivers and Youth in Foster Care. Prev Sci 24, 15–26 (2023). https://doi.org/10.1007/s11121-022-01390-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11121-022-01390-4