Abstract
Background
Prolactinomas are common tumours that significantly reduce quality-of-life (QOL) due to sellar mass effect, secondary hypogonadism, and the peripheral effects of prolactin. Understanding the factors that influence QOL would provide insights into therapeutic targets to optimise patient outcomes and improve wellbeing in prolactinoma.
Methods
A systematic review was performed in accordance with the PRISMA statement. Studies that reported patient QoL using validated metrics were included. Bias and methodological rigour were assessed using the MINORS criteria.
Results
A total of 18 studies were identified studies were available for review, comprising 877 patients. Most were small cross-sectional studies at high risk of bias. Prolactinoma exhibit worse QOL than healthy controls, particularly mental and psychosocial wellbeing. QOL is also worse than patients with non-functional adenomas, but better than those with Cushing’s disease and acromegaly. QOL correlates with prolactin levels, and approaches population baseline with prolonged biochemical control. Dopamine agonists and surgery both improve overall QOL, however improvements are more rapid with surgery.
Conclusion
Poor quality of life in prolactinoma is multifactorial, related to biochemical control, side effects of therapy, and sellar mass effect. Targeting persistent symptoms, reducing healthcare costs, and reducing side-effects of therapy are avenues to improving QOL in patients with prolactinoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prolactinoma (functional lactotroph pituitary neuroendocrine tumours) are the most common pituitary adenoma encountered in daily practice. These tumours come to clinical attention due to sellar mass effect, secondary hypogonadism, and the peripheral effects of prolactin. Through these mechanisms the tumour, and its treatment, can cause significant detriment to physical, social, and emotional functioning. Understanding these effects on patient reported quality of life (QOL) would provide insights into therapeutic targets to optimise patient outcomes [1]. Here, we review the literature on QOL in patients with prolactinomas to elucidate the patient and therapeutic factors that influence patient wellbeing.
Methods
A systematic search of the literature was conducted using the Medline and PubMed databases in accordance with the PRISMA statement [2]. The search included all studies form the database inception until December 2023 using the search string:
(Prolactinoma (MP) OR Lactotroph OR Hyperprolactinaemia OR Hyperprolactinemia) AND (quality of life OR wellbeing OR QOL).
Exclusion criteria were single case reports, studies published in languages other than English, and studies of multiple tumour types where data specific to prolactinomas could not be extracted. The references of identified studies, as well as relevant textbooks, were consulted to identify additional eligible studies.
Titles and abstracts of identified studies were then screened. For appropriate studies, full-text review was performed to determine suitability for inclusion. Inclusion criteria were defined as: (1) Randomized trials, non-randomized trials, and cohort studies that report QOL in prolactinoma; (2) An age-appropriate, validated QoL metric was used to quantify QOL.
Included studies underwent independent data extraction, including study year, study size, treatment status, QOL metric, and QOL outcome. Included studies were assessed for methodological bias using the Methodological Index for Non-Randomized Studies (MINORS) [3].
Results
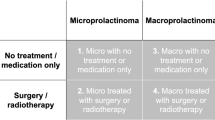
A total of 18 studies were identified from the systematic search of the literature (Supplementary Fig. 1), comprising 877 patients [4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20] (Table 1). Risk of bias results are presented in Supplementary Table 1.
The literature consisted of small retrospective and prospective cohort studies, spanning from 1985 to 2023. These were generally at a high risk of bias. Most studies (81%, 13/16) were cross-sectional, while the three prospective interventional studies had an overall short follow up, ranging from 6 weeks to 12 months. Of those studies reporting disease activity, only 42.6% (252/592) of patients had hyperprolactinemia at the time of the study.
QoL was measured with several metrics including sinonasal and skull base metrics (Anterior skull base questionnaire (ABSQ) [21], Anterior Skull Base Nasal Inventory (ASK-12) [22], Leiden Bother and Needs Questionnaire Pituitary (LBNQ-Pituitary) [4], Sinonasal Outcome Test (SNOT-22) [23], Visual Function Questionnaire (VFQ-25) [24]); depression and anxiety metrics (Beck Depression Inventory (BDI) [25], Hospital Anxiety and Depression Scale (HADS) [26], Hamilton depression score (HRSD) [27], Kellner distress scale (KDS) [28]); fatigue and sleep quality metrics (Epworth Sleepiness Scale (ESS) [29], Fatigue Impact Scale (FIS) [30], Multidimensional Fatigue Inventory (MFI-20) [31], Pittsburgh Sleep Quality Index (PSQI) [32]); social functioning and personality metrics (Eysenck personality questionnaire (EPQ) [33], Modified Social Adjustment Scale (SAS) [34], Tridimensional Personality Questionnaire (TPQ) [35]); and Global QOL metrics (Pittsburgh Sleep Quality Index (PSQI) [32], Functional Assessment of Cancer Therapy (FACT) [36], General Health Questionnaire (GHQ) [37], Health and Labor Questionnaire (HLQ), Nottingham Health Profile (NHP) [38], Short Form 36 (SF-36) [39], Sickness Impact Profile (SIP) [40], World Health Organization Quality of Life Scale (WHO-QoL) [41], 90-item symptom checklist (SCL-90) [42], and 15D [43]).
Prolactinoma compared to Healthy Controls
Ten studies compared patients with prolactinoma to healthy controls. Patients with prolactinoma had worse overall QOL [9,10,11, 18] and mental health [9]. They also experienced greater fatiguability [5], distress [15], and fear of uncertainty [5]. Overall, patients with prolactinoma tended to demonstrate greater impairment in mental rather than physical components of QOL [11, 12]. Anxiety, depression, and mood disorders were more prevalent in patients with prolactinoma, with more than half exhibiting definite or borderline anxiety [16]. Sleep quality and duration was also poorer in patients with prolactinoma [15], with more than one-third demonstrating excessive daytime sleepiness [10].
Compared to other pituitary adenomas
Eleven studies compared QOL in patients with prolactinoma to patients with other pituitary adenomas. Prolactinomas exhibited better overall QOL than patients with Cushing’s disease [8, 44], including physical and cognitive complaints [4], psychosocial functioning [4, 44], and depression scores [13].
Compared to patients with non-functioning adenomas (NFPA), patients with prolactinoma demonstrated a more reserved personality type, characterised by reduced extraversion and increased shyness with strangers [5]. Depression rates were similar, but those on dopamine agonist (DA) therapy showed greater hostility scores [16].
In one study, QOL scores were 0.7 standard deviations (SD) below healthy controls, slightly worse than NFPA (0.5 SD) but better than Cushing’s (1.1 SD) and acromegaly (1.4 SD) [18]. Although this hierarchy of QOL impairment is consistent in treatment naïve patients [11], in surgical series where prolactinoma are usually larger and resistant to medical therapy, QOL detriment can approach [8] or exceed [14] Cushing’s disease and acromegaly patients.
Effect of treatment on QOL
Mental and physical QOL scores correlated inversely with prolactin levels [9, 20]. In many cases biochemical control was not associated with a return of QOL to that of healthy controls, except when biochemical control had been achieved for several years [17, 20]. SF-36 scores were 20–25% lower in patients with active disease compared to those with biochemical control [20]. There is no clear difference in QOL between medical or surgical treatment modalities [19].
In one small double-blind crossover study, treatment with DA led to improvements in depression, anxiety, wellbeing, and friendliness scores as prolactin levels declined [7]. DA therapy improved libido by reducing prolactin [7], but the therapy itself may impact sexual health, as in patients with similar prolactin levels, the use of DA was associated with worse sexual activity scores [15]. In one small study there was no clear difference in QOL between patients treated with bromocriptine and cabergoline [9].
Surgery was associated with improved QoL as early as 5 days postoperatively [14], and scores continued to improve throughout the first postoperative year [8]. Prolactinoma, more than any other adenoma type, had the greatest improvement of QOL within one year of surgery [8, 14]. Clinically significant improvements in SF-36 mental and physical scores were seen in 56% and 37% respectively within 6 months of surgery, although improvements were often seen earlier [8, 14]. Only 6% of cases had clinically significant worsening of QOL after surgery [14].
Predictors of QOL in Prolactinoma
In addition to higher prolactin levels, visual field deficits and central adrenal insufficiency also predicted worse QoL [20]. Amenorrhoea was not associated with QOL, while the association of QOL and adenoma size was conflicting [18, 20]. Patients with higher prolactin and worse QOL scores also had greater healthcare utilisation and spent more money on healthcare [19].
Discussion
Patients with prolactinoma exhibit worse QOL than healthy controls, particularly mental and psychosocial wellbeing. Compared with other functional adenomas, QOL is less severely affected, while QOL is worse than those with NFPA. QOL correlates with prolactin levels, and approaches population baseline with prolonged biochemical control. The effects of DA are beneficial due to suppressive effects on prolactin, however they may themselves contribute to psychosocial dysfunction. Surgery provides a rapid, substantial improvement to QOL, likely though inducing biochemical control and freedom from DA as well as immediate relief of sella mass effect. Relief of mass effect, biochemical control of hyperprolactinaemia, and freedom from DA appear key to normalising QOL in patients with prolactinoma.
Putative effects of Hyperprolactinemia on QOL
Classically confined to the initiation and maintenance of lactation in females, it has become clear that prolactin exerts a range of metabolic, immunologic, and reproductive effects.
Hypogonadotrophic hypogonadism is the most common presenting symptom of hyperprolactinemia, manifesting as oligo-amenorrhoea in pre-menopausal women and impotence in males. Hyperprolactinemia reduces the frequency and amplitude of GnRH secretory pulses, and downstream reductions in LH secretory pulses lead to gonadal suppression. Prolactin exerts its inhibitory tone on kisspeptin neurons, which are the key regulators of pulsatile GnRH neuronal secretion [45]. This is evidenced by the restoration of gonadal function with kisspeptin supplementation in patients with hyperprolactinemia induced hypogonadism [46, 47]. In women, hypogonadism is associated with sexual dysfunction, fatigue, sleep and mood disturbances with corresponding reductions in QOL [48]. In men, the negative effects of hypogonadism on vitality [49], body composition [50], mood [51], cognitive function [52, 53] and sexual health lead to similarly reduced QOL.
Hyperprolactinemia may affect QOL independent of its effects on gonadal hormones. Hyperprolactinaemia is associated with anxiety, somatization, hostility and depression [54]. This may be augmented by the emotional impact of their diagnosis and variable adoption of the sick role [55, 56]. The mechanisms of direct effects of prolactin on the brain and behaviour are unclear. Prolactin influences hypothalamic appetite regulation by inducing leptin resistance, inducing hyperphagia and weight gain [57]. Hypogonadism, particularly androgen deficiency, may further contribute to the development of the metabolic syndrome in hyperprolactinemia. It also acts peripherally, inducing insulin resistance [58, 59] and dyslipidaemia [60]. Dissatisfaction with body composition and appearance may affect mood and QOL. Hyperprolactinemia also has direct effects on bone metabolism, increasing resorption and inhibiting new bone formation, predisposing to fractures [61, 62], which may affect physical functioning, pain, and QOL [63].
Headache has a significant impact on QOL in patients with pituitary adenoma, and prolactinoma may be particularly cephalalgogenic [64, 65]. Headaches occur in both micro- and macro-prolactinomas [66], may be induced by TRH (a potent prolactin secretagogue) [67], and improve with DA therapy [68], implicating prolactin in headache pathogenesis.
Dopamine agonists and QOL
DA are the primary treatment modality for prolactinoma due to their efficacy in achieving biochemical control with a relatively well tolerated side effect profile. Improvements in hyperprolactinemia [7], sexual function [69], metabolic syndrome [70], insulin resistance [71], and restoration of normal gonadal function [72] likely underlie the improvements in QOL seen with DA therapy. However, even when biochemically normalised, QOL does not reach that of healthy controls, suggesting DA themselves may impact QOL, although persistent mass effect or a detrimental effect of hypoprolactinemia64 remain considerations. Treatment duration did not appear to influence QOL [9].
Common side effects of DA include nausea, dizziness and vertigo, headaches, postural hypotension, and abdominal pain [73]. Psychiatric side effects, including mood disorders (depression and mania) and impulse control disorders can also be induced by DA, presumably though stimulation of mesocortico-limbic dopaminergic pathways. These may manifest as gambling, compulsive spending, binge eating, hyperaggressive behaviour, depression, and hypersexuality (augmented by the return of gonadal function), and may occur to a variable degree in a significant proportion of patients [74,75,76]. These psychiatric effects impair psychosocial function and may be deleterious to relationships, reputation, and QOL.
The cumulative cost of DA and their ongoing monitoring can be significant financial stress for patients. The cost of Cabergoline can be $5 to $50 USD per tablet [77], which can total many thousands of dollars annually if higher than standard dosing is required. Hospitalization and specialist care (endocrinologists, general practitioners, ophthalmologists, neurosurgeons, and mental health clinicians) further contribute to healthcare utilisation and costs, which are associated with worse QOL [19].
Surgery for prolactinoma and its effect on QOL
Surgery is traditionally indicated for patients with prolactinoma refractory or intolerant to medical therapy, although first-line surgery is highly effective for patients without cavernous sinus invasion [78, 79]. Surgical cohorts typically exhibit worse QOL due to a prolonged disease course, persistent hyperprolactinemia, side effects of high dose DA, more aggressive histology, and prominent sellar mass effect. The sequelae of sellar mass effect on quality of life [8, 80, 81] is well established, with visual dysfunction [82], hypopituitarism [83], and headache [84] correlated to QOL. Surgery rapidly controls hyperprolactinemia, reduces intrasellar pressure and parasellar mass effect, improves headache [85], and often facilitates emancipation from DA therapy [86], leading to substantial and early improvements in QOL. This supports current guidelines recommending surgery as a viable first-line therapy in well-circumscribed prolactinomas without cavernous sinus extension [87].
Limitations
The included studies were mostly small, cross-sectional, and subject to bias. Of the multiple different QOL metrics were used across studies, few assess the full gamut of symptoms that may occur in prolactinoma and its treatment. The majority of patients in these cross-sectional studies were on DA therapy and had controlled disease. Data was rarely stratified by disease activity, treatment modality, adenoma volume, or socioeconomic status, limiting comparisons. No study directly compared medical and surgical QOL outcomes.
Conclusions
Prolactinomas are associated with decreased QOL due to sellar mass effect, hyperprolactinemia, ensuing hypogonadism, and the adverse effects of DA therapy. Detriments to QOL are global, but mental health, sexual function, and psychosocial functioning appear particularly affected. QOL in patients with prolactinoma is significantly worse than healthy controls, slightly worse than those with NFPA, but often better than those with Cushing’s disease or Acromegaly. Resolution of hyperprolactinemia improves QOL, but slight residual impairment generally persists due to persistent mass effect or the adverse effects and healthcare burden of medical therapy. With long term biochemical control, QOL can approach that of healthy controls. Targeting persistent symptoms, reducing healthcare costs, and reducing side-effects of therapy are avenues to improving QOL in patients with prolactinoma.
Data availability
No datasets were generated or analysed during the current study.
Code availability
N/A
References
Andela CD, Niemeijer ND, Scharloo M et al (2015) Towards a better quality of life (QoL) for patients with pituitary diseases: results from a focus group study exploring QoL. Pituitary 18:86–100. https://doi.org/10.1007/s11102-014-0561-1
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339. https://doi.org/10.1136/bmj.b2535
Slim K, Nini E, Forestier D et al (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73:712–716. https://doi.org/10.1046/j.1445-2197.2003.02748.x
Andela CD, Scharloo M, Ramondt S et al (2016) The development and validation of the Leiden Bother and needs questionnaire for patients with pituitary disease: the LBNQ-Pituitary. Pituitary 19:293–302. https://doi.org/10.1007/s11102-016-0707-4
Athanasoulia AP, Ising M, Pfister H et al (2012) Distinct dopaminergic personality patterns in patients with prolactinomas: a comparison with nonfunctioning pituitary adenoma patients and age- and gender-matched controls. Neuroendocrinology 96:204–211. https://doi.org/10.1159/000335996
Baird A, Sullivan T, Zafar S, Rock J (2003) Quality of life in patients with pituitary tumors: a preliminary study. Qual Manag Health Care 12. https://doi.org/10.1097/00019514-200304000-00005
Buckman MT, Kellner R (1985) Reduction of distress in hyperprolactinemia with bromocriptine. Am J Psychiatry 142:242–244. https://doi.org/10.1176/ajp.142.2.242
Castle-Kirszbaum M, Wang YY, King J, Goldschlager T (2022) Quality of Life after Endoscopic Surgical Management of Pituitary Adenomas. Neurosurgery 90:81–91. https://doi.org/10.1227/NEU.0000000000001740
Cesar de Oliveira Naliato E, Dutra Violante AH, Caldas D et al (2008) Quality of life in women with microprolactinoma treated with dopamine agonists. Pituitary 11:247–254. https://doi.org/10.1007/s11102-008-0091-9
Ernersson A, Bachrack-Lindstrom M, Landberg E et al (2023) Reduced Health Related Quality of Life, increased fatigue, and Daytime Sleepiness in Women with Hyperprolactinemia. Horm Metab Res 55:266–272. https://doi.org/10.1055/a-2042-0712
Johnson MD, Woodburn CJ, Vance ML (2003) Quality of life in patients with a pituitary adenoma. Pituitary 6:81–87
Kars M, van der Klaauw AA, Onstein CS et al (2007) Quality of life is decreased in female patients treated for microprolactinoma. EUR J ENDOCRINOL 157:133–139
Leistner SM, Klotsche J, Dimopoulou C et al (2015) Reduced sleep quality and depression associate with decreased quality of life in patients with pituitary adenomas. EUR J ENDOCRINOL 172:733–743. https://doi.org/10.1530/EJE-14-0941
Lobatto DJ, Zamanipoor Najafabadi AH, de Vries F et al (2019) Toward Value Based Health Care in pituitary surgery: application of a comprehensive outcome set in perioperative care. EUR J ENDOCRINOL 181:375–387. https://doi.org/10.1530/EJE-19-0344
Raappana A, Pirilä T, Ebeling T et al (2012) Long-term health-related quality of life of surgically treated pituitary adenoma patients: a descriptive study. ISRN Endocrinol 2012(675310). https://doi.org/10.5402/2012/675310
Reavley A, Fisher AD, Owen D et al (1997) Psychological distress in patients with hyperprolactinaemia. Clin Endocrinol (Oxf) 47:343–348
Ritvonen E, Karppinen A, Sintonen H et al (2015) Normal long-term health-related quality of life can be achieved in patients with functional pituitary adenomas having surgery as primary treatment. Clin Endocrinol (Oxf) 82:412–421. https://doi.org/10.1111/cen.12550
van der Klaauw AA, Kars M, Biermasz NR et al (2008) Disease-specific impairments in quality of life during long-term follow-up of patients with different pituitary adenomas. Clin Endocrinol (Oxf) 69:775–784. https://doi.org/10.1111/j.1365-2265.2008.03288.x
van der Meulen M, Zamanipoor Najafabadi AH, Lobatto DJ et al (2021) Healthcare utilization and costs among prolactinoma patients: a cross-sectional study and analysis of determinants. Pituitary 24:79–95. https://doi.org/10.1007/s11102-020-01089-1
Vega-Beyhart A, Enriquez-Estrada VM, Bello-Chavolla OY et al (2019) Quality of life is significantly impaired in both secretory and non-functioning pituitary adenomas. Clin Endocrinol (Oxf) 90:457–467. https://doi.org/10.1111/cen.13915
Gil Z, Abergel A, Spektor S et al (2004) Development of a cancer-specific anterior skull base quality-of-life questionnaire. J Neurosurg 100:813–819. https://doi.org/10.3171/jns.2004.100.5.0813
Little AS, Kelly D, Milligan J et al (2013) Prospective validation of a patient-reported nasal quality-of-life tool for endonasal skull base surgery: the anterior Skull Base nasal Inventory-12: clinical article. JNS 119:1068–1074. https://doi.org/10.3171/2013.3.JNS122032
Kennedy JL, Hubbard MA, Huyett P et al (2013) Sino-nasal outcome test (SNOT-22): a predictor of post-surgical improvement in patients with chronic sinusitis. Ann Allergy Asthma Immunol 111:246–251e2. https://doi.org/10.1016/j.anai.2013.06.033
Mangione CM, Lee PP, Gutierrez PR et al (2001) Development of the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol 119:1050–1058. https://doi.org/10.1001/archopht.119.7.1050
Beck AT, Ward CH, Mendelson M et al (1961) An inventory for measuring depression. Arch Gen Psychiatry 4:561–571. https://doi.org/10.1001/archpsyc.1961.01710120031004
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67:361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x
Hamilton M (1980) Rating depressive patients. J Clin Psychiatry 41:21–24
Kellner R (1987) A symptom questionnaire. J Clin Psychiatry 48:268–274
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545. https://doi.org/10.1093/sleep/14.6.540
Fisk JD, Ritvo PG, Ross L et al (1994) Measuring the functional impact of fatigue: initial validation of the fatigue impact scale. Clin Infect Dis 18(Suppl 1):S79–83. https://doi.org/10.1093/clinids/18.supplement_1.s79
Smets EM, Garssen B, Bonke B, De Haes JC (1995) The multidimensional fatigue inventory (MFI) psychometric qualities of an instrument to assess fatigue. J Psychosom Res 39:315–325. https://doi.org/10.1016/0022-3999(94)00125-o
Buysse DJ, Reynolds CF, Monk TH et al (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28:193–213. https://doi.org/10.1016/0165-1781(89)90047-4
Eysenck HJ, Eysenck SBG (1994) Manual of the Eysenck Personality Questionnaire: (EPQ-R Adult). EdITS/Educational and Industrial Testing Service, San Diego, Calif
Cooper P, Osborn M, Gath D, Feggetter G (1982) Evaluation of a modified self-report measure of social adjustment. Br J Psychiatry 141:68–75. https://doi.org/10.1192/bjp.141.1.68
Cloninger CR, Przybeck TR, Svrakic DM (1991) The Tridimensional Personality Questionnaire: U.S. normative data. Psychol Rep 69:1047–1057. https://doi.org/10.2466/pr0.1991.69.3.1047
Cella DF, Tulsky DS, Gray G et al (1993) The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol 11:570–579. https://doi.org/10.1200/JCO.1993.11.3.570
Goldberg DP, Hillier VF (1979) A scaled version of the General Health Questionnaire. Psychol Med 9:139–145. https://doi.org/10.1017/s0033291700021644
Hunt SM, McEwen J, McKenna SP (1985) Measuring health status: a new tool for clinicians and epidemiologists. J R Coll Gen Pract 35:185–188
Ware JE, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. conceptual framework and item selection. Med Care 30:473–483
Bergner M, Bobbitt RA, Carter WB, Gilson BS (1981) The Sickness Impact Profile: Development and final revision of a Health Status measure. Med Care 19:787–805
(1995) The World Health Organization quality of life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med 41:1403–1409. https://doi.org/10.1016/0277-9536(95)00112-K
Derogatis LR, Rickels K, Rock AF (1976) The SCL-90 and the MMPI: a step in the validation of a new self-report scale. Br J Psychiatry 128:280–289. https://doi.org/10.1192/bjp.128.3.280
Sintonen H (2001) The 15D instrument of health-related quality of life: properties and applications. Ann Med 33:328–336. https://doi.org/10.3109/07853890109002086
Heald AH, Ghosh S, Bray S et al (2004) Long-term negative impact on quality of life in patients with successfully treated Cushing’s disease. Clin Endocrinol 61:458–465. https://doi.org/10.1111/j.1365-2265.2004.02118.x
Kokay IC, Petersen SL, Grattan DR (2011) Identification of prolactin-sensitive GABA and kisspeptin neurons in regions of the rat hypothalamus involved in the control of fertility. Endocrinology 152:526–535. https://doi.org/10.1210/en.2010-0668
Hoskova K, Kayton Bryant N, Chen ME et al (2022) Kisspeptin overcomes GnRH neuronal suppression secondary to hyperprolactinemia in humans. J Clin Endocrinol Metab 107:e3515–e3525. https://doi.org/10.1210/clinem/dgac166
Millar RP, Sonigo C, Anderson RA et al (2017) Hypothalamic-pituitary-ovarian Axis Reactivation by Kisspeptin-10 in Hyperprolactinemic Women with Chronic Amenorrhea. J Endocr Soc 1:1362–1371. https://doi.org/10.1210/js.2017-00328
Kałużna M, Kompf P, Rabijewski M et al (2021) Reduced quality of life and sexual satisfaction in isolated hypogonadotropic hypogonadism. J Clin Med 10:2622. https://doi.org/10.3390/jcm10122622
Finas D, Bals-Pratsch M, Sandmann J et al (2006) Quality of life in elderly men with androgen deficiency. Andrologia 38:48–53. https://doi.org/10.1111/j.1439-0272.2006.00684.x
Shabsigh R, Katz M, Yan G, Makhsida N (2005) Cardiovascular issues in hypogonadism and testosterone therapy. Am J Cardiol 96. https://doi.org/10.1016/j.amjcard.2005.10.009. :67 M-72 M
Zitzmann M (2020) Testosterone, mood, behaviour and quality of life. Andrology 8:1598–1605. https://doi.org/10.1111/andr.12867
Hooven CK, Chabris CF, Ellison PT, Kosslyn SM (2004) The relationship of male testosterone to components of mental rotation. Neuropsychologia 42:782–790. https://doi.org/10.1016/j.neuropsychologia.2003.11.012
Lašaitė L, Čeponis J, Preikša RT, Žilaitienė B (2014) Impaired emotional state, quality of life and cognitive functions in young hypogonadal men. Andrologia 46:1107–1112. https://doi.org/10.1111/and.12199
Gomes J, Sousa A, Lima G (2015) Hyperprolactinemia: Effect on Mood? Eur Psychiatry 30:714. https://doi.org/10.1016/S0924-9338(15)30564-2
Sobrinho LG (1991) Neuropsychiatry of prolactin: causes and effects. Baillière’s Clin Endocrinol Metabolism 5:119–142. https://doi.org/10.1016/S0950-351X(05)80100-4
Sobrinho LG (1998) Emotional aspects of hyperprolactinemia. Psychother Psychosom 67:133–139. https://doi.org/10.1159/000012273
Naef L, Woodside B (2007) Prolactin/Leptin interactions in the control of food intake in rats. Endocrinology 148:5977–5983. https://doi.org/10.1210/en.2007-0442
Landgraf R, Landraf-Leurs MM, Weissmann A et al (1977) Prolactin: a diabetogenic hormone. Diabetologia 13:99–104. https://doi.org/10.1007/BF00745135
Schernthaner G, Prager R, Punzengruber C, Luger A (1985) Severe hyperprolactinaemia is associated with decreased insulin binding in vitro and insulin resistance in vivo. Diabetologia 28:138–142. https://doi.org/10.1007/BF00273860
Krysiak R, Kowalcze K, Okopień B (2022) Cardiometabolic profile of young women with hypoprolactinemia. Endocrine 78:135–141. https://doi.org/10.1007/s12020-022-03145-1
Vestergaard P, Jørgensen JOL, Hagen C et al (2002) Fracture risk is increased in patients with GH deficiency or untreated prolactinomas–a case-control study. Clin Endocrinol (Oxf) 56:159–167. https://doi.org/10.1046/j.0300-0664.2001.01464.x
Di Filippo L, Doga M, Resmini E, Giustina A (2020) Hyperprolactinemia and bone. Pituitary 23:314–321. https://doi.org/10.1007/s11102-020-01041-3
Adachi JD, Adami S, Gehlbach S et al (2010) Impact of prevalent fractures on quality of life: baseline results from the global longitudinal study of osteoporosis in women. Mayo Clin Proc 85:806–813. https://doi.org/10.4065/mcp.2010.0082
Levy MJ, Jäger HR, Powell M et al (2004) Pituitary volume and headache: size is not everything. Arch Neurol 61:721–725. https://doi.org/10.1001/archneur.61.5.721
Abe T, Matsumoto K, Kuwazawa J et al (1998) Headache associated with pituitary adenomas. Headache 38:782–786
Colao A, Vitale G, Cappabianca P et al (2004) Outcome of cabergoline treatment in men with prolactinoma: effects of a 24-month treatment on prolactin levels, tumor mass, recovery of pituitary function, and semen analysis. J Clin Endocrinol Metab 89:1704–1711. https://doi.org/10.1210/jc.2003-030979
Bosco D, Belfiore A, Fava A et al (2008) Relationship between high prolactin levels and migraine attacks in patients with microprolactinoma. J Headache Pain 9:103–107. https://doi.org/10.1007/s10194-008-0016-z
Al-Karagholi MA-M, Kalatharan V, Ghanizada H et al (2023) Prolactin in headache and migraine: a systematic review of clinical studies. Cephalalgia 43:3331024221136286. https://doi.org/10.1177/03331024221136286
Krysiak R, Okopień B (2019) Sexual functioning in hyperprolactinemic patients treated with cabergoline or bromocriptine. Am J Ther 26:e433–e440. https://doi.org/10.1097/MJT.0000000000000777
Auriemma RS, Granieri L, Galdiero M et al (2013) Effect of cabergoline on metabolism in prolactinomas. Neuroendocrinology 98:299–310. https://doi.org/10.1159/000357810
Pirchio R, Auriemma RS, Solari D et al (2021) Effects of Pituitary surgery and high-dose Cabergoline Therapy on Metabolic Profile in patients with Prolactinoma resistant to Conventional Cabergoline Treatment. Front Endocrinol (Lausanne) 12:769744. https://doi.org/10.3389/fendo.2021.769744
Webster J, Piscitelli G, Polli A et al (1994) A comparison of cabergoline and bromocriptine in the treatment of hyperprolactinemic amenorrhea. Cabergoline Comparative Study Group. N Engl J Med 331:904–909. https://doi.org/10.1056/NEJM199410063311403
Wang AT, Mullan RJ, Lane MA et al (2012) Treatment of hyperprolactinemia: a systematic review and meta-analysis. Syst Rev 1:33. https://doi.org/10.1186/2046-4053-1-33
Child L, Martin N (2023) Psychiatric side effects of cabergoline treatment of hyperprolactinaemia: risk factors and prevalence of patient counselling and monitoring. In: Endocrine Abstracts, Bioscientifica
De Sousa SMC, Baranoff J, Rushworth RL et al (2020) Impulse Control disorders in dopamine agonist-treated hyperprolactinemia: prevalence and risk factors. J Clin Endocrinol Metab 105:dgz076. https://doi.org/10.1210/clinem/dgz076
Ioachimescu AG, Fleseriu M, Hoffman AR et al (2019) Psychological effects of dopamine agonist treatment in patients with hyperprolactinemia and prolactin-secreting adenomas. Eur J Endocrinol 180:31–40. https://doi.org/10.1530/EJE-18-0682
Zygourakis CC, Imber BS, Chen R et al (2017) Cost-effectiveness analysis of Surgical versus Medical Treatment of Prolactinomas. J Neurol Surg B Skull Base 78:125–131. https://doi.org/10.1055/s-0036-1592193
Andereggen L, Frey J, Andres RH et al (2021) First-line surgery in prolactinomas: lessons from a long-term follow-up study in a tertiary referral center. J Endocrinol Invest 44:2621–2633. https://doi.org/10.1007/s40618-021-01569-6
Park JY, Choi W, Hong AR et al (2021) Surgery is a safe, effective first-line treatment modality for noninvasive prolactinomas. Pituitary 24:955–963. https://doi.org/10.1007/s11102-021-01168-x
Castle-Kirszbaum M, Shi MD, Goldschlager T (2021) Quality of Life in Craniopharyngioma: A Scoping Review. Under Review
Castle-Kirszbaum M, Wang YY, King J et al (2023) Quality of life and surgical outcomes in incidental pituitary adenomas undergoing endoscopic endonasal resection. J Neurosurg 138:567–573. https://doi.org/10.3171/2022.5.JNS2286
Nayeni M, Dang A, Mao AJ, Malvankar-Mehta MS (2021) Quality of life of low vision patients: a systematic review and meta-analysis. Can J Ophthalmol 56:151–157. https://doi.org/10.1016/j.jcjo.2020.10.014
Crespo I, Santos A, Webb SM (2015) Quality of life in patients with hypopituitarism. Curr Opin Endocrinol Diabetes Obes 22:306–312. https://doi.org/10.1097/MED.0000000000000169
Pereira-Neto A, Borba AM, de Mello PA et al (2010) Mean intrasellar pressure, visual field, headache intensity and quality of life of patients with pituitary adenoma. Arq Neuropsiquiatr 68:350–354. https://doi.org/10.1590/s0004-282x2010000300004
Delport R, King J, Castle-Kirszbaum M et al (2023) Headache improvement following endoscopic resection of Pituitary Adenomas. World Neurosurg 176:e456–e461. https://doi.org/10.1016/j.wneu.2023.05.082
Findlay MC, Sabahi M, Azab M et al (2024) The role of surgical management for prolactin-secreting tumors in the era of dopaminergic agonists: an international multicenter report. Clin Neurol Neurosurg 236:108079. https://doi.org/10.1016/j.clineuro.2023.108079
Petersenn S, Fleseriu M, Casanueva FF et al (2023) Diagnosis and management of prolactin-secreting pituitary adenomas: a Pituitary Society international Consensus Statement. Nat Rev Endocrinol 19:722–740. https://doi.org/10.1038/s41574-023-00886-5
Funding
Nil funding.
Open Access funding enabled and organized by CAUL and its Member Institutions
Author information
Authors and Affiliations
Contributions
MCK (Collection Analysis of the data, writing the draft, revision), NB (writing the draft, revision, study supervision), JK (writing the draft, revision, study supervision), TG (writing the draft, revision, study supervision).
Corresponding author
Ethics declarations
Ethics approval
Not required.
Consent to participate
Not required.
Consent for publication
Not required.
Competing interests
No conflicts to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Castle-Kirszbaum, M., Biermasz, N., Kam, J. et al. Quality of life in Prolactinoma: A systematic review. Pituitary (2024). https://doi.org/10.1007/s11102-024-01392-1
Accepted:
Published:
DOI: https://doi.org/10.1007/s11102-024-01392-1