Abstract
Background
As endoscopic transsphenoidal approaches are more routinely selected for progressively larger pituitary adenomas with parasellar extension, understanding potential anatomical factors that limit resection and contribute to complications is becoming increasingly important for tailoring a surgical approach. This study aimed to reevaluate existing predictive tools for resectability in pituitary adenomas specifically with suprasellar extension, and furthermore identify any additional measurable features that may be more useful in preoperative planning.
Methods
A single-center retrospective chart review of adult patients who underwent endoscopic transsphenoidal surgery for pituitary adenomas with suprasellar extension from 2015 to 2020 was performed. Preoperative MRIs were systematically assessed to assign a Knosp classification, a Zurich Pituitary Score (ZPS), and for dimensional measurements of the suprasellar aspect of the lesions. Univariate comparisons and multivariate regression models were employed to assess the influence of these factors on extent of resection and postoperative complications.
Results
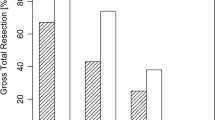
Of the 96 patients with suprasellar pituitary adenomas who underwent endoscopic transsphenoidal surgery, 74 patients (77%) had a gross total resection (GTR). Neither Knosp grade nor ZPS score, even when dichotomized, demonstrated an association with GTR (Knosp 3A-4 versus Knosp 0–2, p = 0.069; ZPS III-IV versus ZPS I-II, p = 0.079). Multivariate regression analysis identified suprasellar anterior-posterior tumor diameter (SSAP) as the only significant predictor of extent of resection in this cohort (OR 0.951, 95% CI 0.905-1.000, p = 0.048*). A higher SSAP also had the strongest association with intraoperative CSF leaks (p = 0.0012*) and an increased overall rate of postoperative complications (p = 0.002*). Further analysis of the regression model for GTR suggested an optimal cut point value for SSAP of 23.7 mm, above which predictability for failing to achieve GTR carried a sensitivity of 89% and a specificity of 41%.
Conclusions
This study is unique in its examination of endoscopic transsphenoidal surgical outcomes for pituitary adenomas with suprasellar extension. Our findings suggest that previously established grading systems based on lateral extension into the cavernous sinus lose their predictive value in lesions with suprasellar extension and, more specifically, with increasing suprasellar anterior-posterior diameter.



Similar content being viewed by others
Data Availability
Not applicable.
References
Castle-Kirszbaum M, Wang YY, King J, Goldschlager T (2022) Quality of Life after Endoscopic Surgical Management of Pituitary Adenomas. Neurosurgery 90(1):81–91
Castle-Kirszbaum M, Wang YY, King J, Goldschlager T (2022) Predictors of visual and endocrine outcomes after endoscopic transsphenoidal surgery for pituitary adenomas. Neurosurg Rev 45(1):843–853
Castle-Kirszbaum M, Wang YY, King J, Kam J, Goldschlager T (2023) The HACKD Score-Predicting extent of resection of Pituitary Macroadenomas through an endoscopic endonasal Transsphenoidal Approach. Oper Neurosurg (Hagerstown) 24(2):154–161
Younus I, Gerges MM, Uribe-Cardenas R, Morgenstern P, Kacker A, Tabaee A, Anand VK, Schwartz TH (2020) The slope of the learning curve in 600 consecutive endoscopic transsphenoidal pituitary surgeries. Acta Neurochir (Wien) 162(10):2361–2370
Little AS, Kelly DF, White WL, Gardner PA, Fernandez-Miranda JC, Chicoine MR, Barkhoudarian G, Chandler JP, Prevedello DM, Liebelt BD, Sfondouris J, Mayberg MR (2019) Results of a prospective multicenter controlled study comparing surgical outcomes of microscopic versus fully endoscopic transsphenoidal surgery for nonfunctioning pituitary adenomas: the Transsphenoidal extent of resection (TRANSSPHER) study. J Neurosurg 132(4):1043–1053
Knosp EK, Steiner ES, Kitz K, Matula C (1993) Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery 33(4):610–617 ; discussion 617-8
Micko AS, Wöhrer A, Wolfsberger S, Knosp E (2015) Invasion of the cavernous sinus space in pituitary adenomas: endoscopic verification and its correlation with an MRI-based classification. J Neurosurg 122(4):803–811
Mooney MA, Hardesty DA, Sheehy JP, Bird R, Chapple K, White WL, Little AS (2017) Interrater and intrarater reliability of the Knosp scale for pituitary adenoma grading. J Neurosurg 126(5):1714–1719
Serra C, Staartjes VE, Maldaner N, Muscas G, Akeret K, Holzmann D, Soyka MB, Schmid C, Regli L (2018) Predicting extent of resection in transsphenoidal surgery for pituitary adenoma. Acta Neurochir (Wien) 160(11):2255–2262
Staartjes VE, Serra C, Zoli M, Mazzatenta D, Pozzi F, Locatelli D, D’Avella E, Solari D, Cavallo LM, Regli L (2020) Multicenter external validation of the Zurich Pituitary score. Acta Neurochir (Wien) 162(6):1287–1295
Dehdashti AR, Ganna A, Witterick I, Gentili F (2009) Expanded endoscopic endonasal approach for anterior cranial base and suprasellar lesions: indications and limitations, Neurosurgery 64(4) 677 – 87; discussion 687-9.
Peto I, Abou-Al-Shaar H, White TG, Abunimer AM, Kwan K, Zavadskiy G, Wagner K, Black K, Eisenberg M, Bruni M, Dehdashti AR (2020) Sources of residuals after endoscopic transsphenoidal surgery for large and giant pituitary adenomas. Acta Neurochir (Wien) 162(10):2341–2351
Koutourousiou M, Gardner PA, Fernandez-Miranda JC, Paluzzi A, Wang EW, Snyderman CH (2013) Endoscopic endonasal surgery for giant pituitary adenomas: advantages and limitations. J Neurosurg 118(3):621–631
Bouthillier A, van Loveren HR, Keller JT (1996) Segments of the internal carotid artery: a new classification, Neurosurgery 38(3) 425 – 32; discussion 432-3.
Dehdashti AR, Ganna A, Karabatsou K, Gentili F (2008) Pure endoscopic endonasal approach for pituitary adenomas: early surgical results in 200 patients and comparison with previous microsurgical series. Neurosurgery 62(5):1006–1015 discussion 1015-7
Hughes G (2015) Youden’s index and the weight of evidence. Methods Inf Med 54(2):198–199
Youden WJ (1950) Index for rating diagnostic tests. Cancer 3(1):32–35
Hofstetter CP, Nanaszko MJ, Mubita LL, Tsiouris J, Anand VK, Schwartz TH (2012) Volumetric classification of pituitary macroadenomas predicts outcome and morbidity following endoscopic endonasal transsphenoidal surgery. Pituitary 15(3):450–463
Cappabianca P, Cavallo LM, Esposito F, De Divitiis O, Messina A, De Divitiis E (2008) Extended endoscopic endonasal approach to the midline skull base: the evolving role of transsphenoidal surgery. Adv Tech Stand Neurosurg 33:151–199
Couldwell WT, Weiss MH, Rabb C, Liu JK, Apfelbaum RI, Fukushima T (2004) Variations on the standard transsphenoidal approach to the sellar region, with emphasis on the extended approaches and parasellar approaches: surgical experience in 105 cases, Neurosurgery 55(3) 539 – 47; discussion 547 – 50.
Little AS, Chicoine MR, Kelly DF, Sarris CE, Mooney MA, White WL, Gardner PA, Fernandez-Miranda JC, Barkhoudarian G, Chandler JP, Prevedello DM, Liebelt BD, Sfondouris J, Mayberg MR (2020) Evaluation of Surgical resection goal and its relationship to extent of resection and patient outcomes in a Multicenter prospective study of patients with surgically treated, nonfunctioning pituitary adenomas: a Case Series. Oper Neurosurg (Hagerstown) 18(1):26–33
DiRisio AC, Feng R, Shuman WH, Platt S, Price G, Dullea JT, Gilja S, D’Andrea MR, Delman BN, Bederson JB, Shrivastava RK (2023) The Knosp Criteria Revisited: 3-Dimensional volumetric analysis as a Predictive Tool for Extent of Resection in Complex endoscopic pituitary surgery. Neurosurgery 92(1):179–185
Connor SE, Wilson F, Hogarth K (2014) Magnetic resonance imaging criteria to predict complete excision of parasellar pituitary macroadenoma on postoperative imaging. J Neurol Surg B Skull Base 75(1):41–46
Heffernan AT, Han JK, Campbell J, Reese J, Day WG, Edwards J, Singh RV, Zhu W, Lam KK (2022) Predictive value of pituitary tumor morphology on outcomes and complications in endoscopic transsphenoidal surgery. World J Otorhinolaryngol Head Neck Surg 8(4):321–329
Silva D, Attia M, Kandasamy J, Alimi M, Anand VK, Schwartz TH (2014) Endoscopic endonasal transsphenoidal above and below approach to the retroinfundibular area and interpeduncular cistern–cadaveric study and case illustrations. World Neurosurg 81(2):374–384
Mooney MA, Hardesty DA, Sheehy JP, Bird CR, Chapple K, White WL, Little AS (2017) Rater reliability of the hardy classification for Pituitary Adenomas in the magnetic resonance imaging era. J Neurol Surg B Skull Base 78(5):413–418
Mooney MA, Sarris CE, Zhou JJ, Barkhoudarian G, Chicoine MR, Fernandez-Miranda JC, Gardner PA, Hardesty DA, Jahnke H, Kelly DF, Liebelt BD, Mayberg MR, Prevedello DM, Sfondouris J, Sheehy JP, Chandler JP, Yuen KCJ, White WL (2019) Little, proposal and validation of a simple grading scale (TRANSSPHER Grade) for Predicting Gross Total Resection of Nonfunctioning Pituitary Macroadenomas after transsphenoidal surgery. Oper Neurosurg (Hagerstown) 17(5):460–469
Wang M, Cai Y, Jiang Y, Peng Y (2021) Risk factors impacting intra- and postoperative cerebrospinal fluid rhinorrhea on the endoscopic treatment of pituitary adenomas: a retrospective study of 250 patients. Med (Baltim) 100(49):e27781
Magro E, Graillon T, Lassave J, Castinetti F, Boissonneau S, Tabouret E, Fuentes S, Velly L, Gras R, Dufour H (2016) Complications related to the endoscopic endonasal Transsphenoidal Approach for Nonfunctioning Pituitary Macroadenomas in 300 consecutive patients. World Neurosurg 89:442–453
do Amaral LC, Reis BL, Ribeiro-Oliveira A Jr, da Silva Santos TM, Giannetti AV (2021) Comparative study of complications after primary and revision transsphenoidal endoscopic surgeries. Neurosurg Rev 44(3):1687–1702
Castle-Kirszbaum M, Fuller P, Wang YY, King J, Goldschlager T (2021) Diabetes insipidus after endoscopic transsphenoidal surgery: multicenter experience and development of the SALT score. Pituitary 24(6):867–877
Mattogno PP, Caccavella VM, Giordano M, D’Alessandris QG, Chiloiro S, Tariciotti L, Olivi A, Lauretti L (2022) Interpretable machine learning-based prediction of Intraoperative Cerebrospinal Fluid Leakage in Endoscopic Transsphenoidal Pituitary surgery: a pilot study. J Neurol Surg B Skull Base 83(5):485–495
Slot EMH, Sabaoglu R, Voormolen EHJ, Hoving EW, van Doormaal TPC (2022) Cerebrospinal fluid leak after transsphenoidal surgery: a systematic review and Meta-analysis. J Neurol Surg B Skull Base 83(Suppl 2):e501–e513
Makarenko S, Alzahrani I, Karsy M, Deopujari C, Couldwell WT (2022) Outcomes and surgical nuances in management of giant pituitary adenomas: a review of 108 cases in the endoscopic era, J Neurosurg 1–12
Palpan Flores A, Sáez Alegre M, Vivancos Sanchez C, Pérez AZ, Pérez-López C (2023) Volumetric resection and complications in nonfunctioning pituitary adenoma by fully endoscopic Transsphenoidal Approach along 15 years of single-center experience. J Neurol Surg B Skull Base 84(1):8–16
Salenave S, Gatta B, Pecheur S, San-Galli F, Visot A, Lasjaunias P, Roger P, Berge J, Young J, Tabarin A, Chanson P (2004) Pituitary magnetic resonance imaging findings do not influence surgical outcome in adrenocorticotropin-secreting microadenomas. J Clin Endocrinol Metab 89(7):3371–3376
Wang H, Zhang W, Li S, Fan Y, Feng M, Wang R (2021) Development and evaluation of Deep Learning-based Automated Segmentation of Pituitary Adenoma in Clinical Task. J Clin Endocrinol Metab 106(9):2535–2546
Acknowledgements
The authors would like to acknowledge Dr. Michael Schulder, Dr. Mark Chaskes, Dr. Margherita Bruni, and Dr. Griffin Baum for their support of the trainees who put together this article and for their overall guidance in the publication process.
Funding
This work received no funding, sponsorship, or other material supplementation.
Author information
Authors and Affiliations
Contributions
Manuscript drafting and revision (DG, JP, TW, EQ, HS, AD); Clinical data collection and interpretation (TW, MR, HS, DG, ME, AD); Figure design (DG, JP, EQ, KY, JF); Manuscript editing and revision (JP, EQ, KY, JF, ME, AD); Literature review (DG, JP); Research team management and oversight (JF, ME, AD). All authors reviewed the final version of the manuscript for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Institutional Review Board (IRB) approval for this single-center retrospective chart review study to review individual patient charts for data capture was obtained by the lead author under the guidelines set forth by the Northwell Health Human Research Protection Program. Given the retrospective nature of the research and supervised anonymization process for data collection under IRB guidelines, individual patient consent to participate and consent to publish were not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Park, J., Golub, D., White, T.G. et al. Anterior-posterior diameter is a key driver of resectability and complications for pituitary adenomas with suprasellar extension in endoscopic transsphenoidal surgery. Pituitary 26, 629–641 (2023). https://doi.org/10.1007/s11102-023-01354-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-023-01354-z