Abstract
Purpose
Neurolysin (Nln) is a peptidase that functions to preserve the brain following ischemic stroke by hydrolyzing various neuropeptides. Nln activation has emerged as an attractive drug discovery target for treatment of ischemic stroke. Among first-in-class peptidomimetic Nln activators, we selected three lead compounds (9d, 10c, 11a) for quantitative pharmacokinetic analysis to provide valuable information for subsequent preclinical development.
Methods
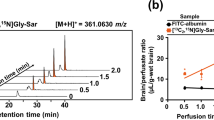
Pharmacokinetic profile of these compounds was studied in healthy and ischemic stroke-induced mice after bolus intravenous administration. Brain concentration and brain uptake clearance (Kin) was calculated from single time point analysis. The inter-relationship between LogP with in-vitro and in-vivo permeability was studied to determine CNS penetration. Brain slice uptake method was used to study tissue binding, whereas P-gp-mediated transport was evaluated to understand the potential brain efflux of these compounds.
Results
According to calculated parameters, all three compounds showed a detectable amount in the brain after intravenous administration at 4 mg/kg; however, 11a had the highest brain concentration and brain uptake clearance. A strong correlation was documented between in-vitro and in-vivo permeability data. The efflux ratio of 10c was ~6-fold higher compared to 11a and correlated well with its lower Kin value. In experimental stroke animals, the Kin of 11a was significantly higher in ischemic vs. contralateral and intact hemispheres, though it remained below its A50 value required to activate Nln.
Conclusions
Collectively, these preclinical pharmacokinetic studies reveal promising BBB permeability of 11a and indicate that it can serve as an excellent lead for developing improved drug-like Nln activators.







Similar content being viewed by others
References
Savitz SI, Baron J-C, Fisher M, Consortium SX. Stroke treatment academic industry roundtable X: brain cytoprotection therapies in the reperfusion era. Stroke. 2019;50(4):1026–31.
Savitz SI, Fisher M. Future of neuroprotection for acute stroke: in the aftermath of the SAINT trials. Annals of Neurology: Official Journal of the American Neurological Association and the Child Neurology Society. 2007;61(5):396–402.
Tymianski M. Combining neuroprotection with endovascular treatment of acute stroke: is there hope? Stroke. 2017;48(6):1700–5.
Fisher M, Ratan R. New perspectives on developing acute stroke therapy. Annals of Neurology: Official Journal of the American Neurological Association and the Child Neurology Society. 2003;53(1):10–20.
Checler F, Ferro ES. Neurolysin: from initial detection to latest advances. Neurochem Res. 2018;43(11):2017–24.
Shrimpton CN, Smith AI, Lew RA. Soluble metalloendopeptidases and neuroendocrine signaling. Endocr Rev. 2002;23(5):647–64.
Wangler NJ, Santos KL, Schadock I, Hagen FK, Escher E, Bader M, et al. Identification of membrane-bound variant of metalloendopeptidase neurolysin (EC 3.4. 24.16) as the non-angiotensin type 1 (non-AT1), non-AT2 angiotensin binding site. J Biol Chem. 2012;287(1):114–22.
Karamyan VT. The role of peptidase neurolysin in neuroprotection and neural repair after stroke. Neural Regen Res. 2021;16(1):21.
Al-Ahmad AJ, Pervaiz I, Karamyan VT. Neurolysin substrates bradykinin, neurotensin and substance P enhance brain microvascular permeability in a human in vitro model. J Neuroendocrinol. 2021;33(2):e12931.
Karamyan VT. Peptidase neurolysin is an endogenous cerebroprotective mechanism in acute neurodegenerative disorders. Med Hypotheses. 2019;131:109309.
Jayaraman S, Al Shoyaib A, Kocot J, Villalba H, Alamri FF, Rashid M, et al. Peptidase neurolysin functions to preserve the brain after ischemic stroke in male mice. J Neurochem. 2020;153(1):120–37.
Rashid M, Arumugam TV, Karamyan VT. Association of the novel non-AT1, non-AT2 angiotensin binding site with neuronal cell death. J Pharmacol Exp Ther. 2010;335(3):754–61.
Rashid M, Wangler NJ, Yang L, Shah K, Arumugam TV, Abbruscato TJ, et al. Functional up-regulation of endopeptidase neurolysin during post-acute and early recovery phases of experimental stroke in mouse brain. J Neurochem. 2014;129(1):179–89.
Jayaraman S, Kocot J, Esfahani SH, Wangler NJ, Uyar A, Mechref Y, et al. Identification and characterization of two structurally related dipeptides that enhance catalytic efficiency of neurolysin. J Pharmacol Exp Ther. 2021;379(2):191–202.
Rahman MS, Kumari S, Esfahani SH, Nozohouri S, Jayaraman S, Kinarivala N, et al. Discovery of first-in-class Peptidomimetic Neurolysin activators possessing enhanced brain penetration and stability. J Med Chem. 2021.
Nozohouri S, Sifat AE, Vaidya B, Abbruscato TJ. Novel approaches for the delivery of therapeutics in ischemic stroke. Drug Discov Today. 2020.
Hammarlund-Udenaes M, Fridén M, Syvänen S, Gupta A. On the rate and extent of drug delivery to the brain. Pharm Res. 2008;25(8):1737–50.
Abbott NJ. Evidence for bulk flow of brain interstitial fluid: significance for physiology and pathology. Neurochem Int. 2004;45(4):545–52.
Liu X, Smith BJ, Chen C, Callegari E, Becker SL, Chen X, et al. Evaluation of cerebrospinal fluid concentration and plasma free concentration as a surrogate measurement for brain free concentration. Drug Metab Dispos. 2006;34(9):1443–7.
Pardridge WM. The isolated brain microvessel: a versatile experimental model of the blood-brain barrier. Front Physiol. 2020;11:398.
Ohashi R, Watanabe R, Esaki T, Taniguchi T, Torimoto-Katori N, Watanabe T, et al. Development of simplified in vitro P-glycoprotein substrate assay and in silico prediction models to evaluate transport potential of P-glycoprotein. Mol Pharm. 2019;16(5):1851–63.
Nozohouri S, Noorani B, Al-Ahmad A, Abbruscato TJ. Estimating Brain Permeability Using In Vitro Blood-Brain Barrier Models. 2020.
Friden M, Ducrozet F, Middleton B, Antonsson M, Bredberg U, Hammarlund-Udenaes M. Development of a high-throughput brain slice method for studying drug distribution in the central nervous system. Drug Metab Dispos. 2009;37(6):1226–33.
Rice ME. Use of ascorbate in the preparation and maintenance of brain slices. Methods. 1999;18(2):144–9.
Harashima H, Sugiyama Y, Sawada Y, Iga T, Hanano M. Comparison between in-vivo and in-vitro tissue-to-plasma unbound concentration ratios (Kp, f) of quinidine in rats. J Pharm Pharmacol. 1984;36(5):340–2.
Loryan I, Fridén M, Hammarlund-Udenaes M. The brain slice method for studying drug distribution in the CNS. Fluids and Barriers of the CNS. 2013;10(1):1–9.
Yang L, Wang H, Shah K, Karamyan VT, Abbruscato TJ. Opioid receptor agonists reduce brain edema in stroke. Brain Res. 2011;1383:307–16.
Yang L, Islam MR, Karamyan VT, Abbruscato TJ. In vitro and in vivo efficacy of a potent opioid receptor agonist, biphalin, compared to subtype-selective opioid receptor agonists for stroke treatment. Brain Res. 2015;1609:1–11.
Smith QR. A review of blood-brain barrier transport techniques. The Blood-Brain Barrier. 2003:193–208.
Brouwer KL, Keppler D, Hoffmaster KA, Bow DA, Cheng Y, Lai Y, et al. In vitro methods to support transporter evaluation in drug discovery and development. Clinical Pharmacology & Therapeutics. 2013;94(1):95–112.
Summerfield SG, Stevens AJ, Cutler L, del Carmen OM, Hammond B, Tang S-P, et al. Improving the in vitro prediction of in vivo central nervous system penetration: integrating permeability, P-glycoprotein efflux, and free fractions in blood and brain. J Pharmacol Exp Ther. 2006;316(3):1282–90.
Demeule M, Régina A, Jodoin J, Laplante A, Dagenais C, Berthelet F, et al. Drug transport to the brain: key roles for the efflux pump P-glycoprotein in the blood–brain barrier. Vasc Pharmacol. 2002;38(6):339–48.
Seelig A, Landwojtowicz E. Structure–activity relationship of P-glycoprotein substrates and modifiers. Eur J Pharm Sci. 2000;12(1):31–40.
Wang Y, Welty DR. The simultaneous estimation of the influx and efflux blood-brain barrier permeabilities of gabapentin using a microdialysis-pharmacokinetic approach. Pharm Res. 1996;13(3):398–403.
Gupta A, Chatelain P, Massingham R, Jonsson EN, Hammarlund-Udenaes M. Brain distribution of cetirizine enantiomers: comparison of three different tissue-to-plasma partition coefficients: Kp, Kp, u, and Kp, uu. Drug Metab Dispos. 2006;34(2):318–23.
Friden M, Gupta A, Antonsson M, Bredberg U, Hammarlund-Udenaes M. In vitro methods for estimating unbound drug concentrations in the brain interstitial and intracellular fluids. Drug Metab Dispos. 2007;35(9):1711–9.
Liu S, Levine SR, Winn HR. Targeting ischemic penumbra: part I-from pathophysiology to therapeutic strategy. Journal of experimental stroke & translational medicine. 2010;3(1):47.
Goyal M, Ospel JM, Menon B, Almekhlafi M, Jayaraman M, Fiehler J, et al. Challenging the ischemic core concept in acute ischemic stroke imaging. Stroke. 2020;51(10):3147–55.
De Saint-Hubert M, Prinsen K, Mortelmans L, Verbruggen A, Mottaghy FM. Molecular imaging of cell death. Methods. 2009;48(2):178–87.
Liu S, Levine SR, Winn HR. Targeting ischemic penumbra part II: selective drug delivery using liposome technologies. Journal of experimental stroke & translational medicine. 2011;4(1):16.
Acknowledgments and Disclosures
Authors declare no conflict of interest.
Funding
This project was supported by NIH grant R01NS106879 to P.C.T., V.T.K. and T.J.A.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nozohouri, S., Esfahani, S.H., Noorani, B. et al. In-Vivo and Ex-Vivo Brain Uptake Studies of Peptidomimetic Neurolysin Activators in Healthy and Stroke Animals. Pharm Res 39, 1587–1598 (2022). https://doi.org/10.1007/s11095-022-03218-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-022-03218-w