Abstract
Purpose
Studies have demonstrated that higher surgical volumes correlate with improved neurosurgical outcomes yet none exist evaluating the effects of hospital teaching status on the surgical neuro-oncology patient. We present the first analysis comparing brain tumor surgery perioperative outcomes at academic and non-teaching centers.
Methods
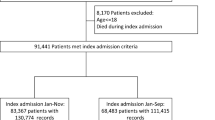
Brain tumor surgeries in the Nationwide Inpatient Sample (NIS) from 1998 to 2014 were identified. A teaching hospital, defined by the NIS, must have ≥ 1 Accreditation Council of Graduate Medical Education (ACGME) approved residency programs, Council of Teaching Hospitals membership, or have a ratio ≥ 0.25 of full-time residents to hospital beds. Annual treatment trends were stratified by hospital teaching status, assessing yearly caseload with linear regression. Multivariable logistic regression determined predictors of inpatient mortality/complications. Hospitals were further divided into quartiles by case volume and teaching status was compared in each.
Results
Teaching hospitals (THs) exhibited an average annual increase in brain tumor surgeries (+ 1057/year, p < 0.0001). In multivariable analysis, teaching status was associated with decreased risk of mortality (OR 0.82, p = 0.0003) and increased likelihood of discharge home (OR 1.21, p < 0.0001). In subgroup analysis, within the highest hospital quartile by caseload, higher mortality rates and lower routine discharges were again seen at non-teaching hospitals (NTHs) (p = 0.0002 and p = 0.0016, respectively).
Conclusion
THs are performing more brain tumor surgeries over time with lower rates of inpatient mortality and perioperative complications even after controlling for hospital case volume. These results suggest a shift in neuro-oncology practice patterns favoring THs to optimize patient outcomes especially at the highest volume centers.

Similar content being viewed by others
References
Youngerman BE, Bruce JN (2018) Capturing quality: the challenge for high-volume academic medical centers. Mayo Clin Proc 93:4–6. https://doi.org/10.1016/j.mayocp.2017.11.010
Trinh VT, Davies JM, Berger MS (2015) Surgery for primary supratentorial brain tumors in the United States, 2000–2009: effect of provider and hospital caseload on complication rates. J Neurosurg 122:280–296. https://doi.org/10.3171/2014.9.JNS131648
Barker FG 2nd (2004) Craniotomy for the resection of metastatic brain tumors in the U.S., 1988–2000: decreasing mortality and the effect of provider caseload. Cancer 100:999–1007. https://doi.org/10.1002/cncr.20058
Barker FG 2nd, Curry WT Jr, Carter BS (2005) Surgery for primary supratentorial brain tumors in the United States, 1988 to 2000: the effect of provider caseload and centralization of care. Neuro Oncol 7:49–63. https://doi.org/10.1215/S1152851704000146
Smith ER, Butler WE, Barker FG 2nd (2004) Craniotomy for resection of pediatric brain tumors in the United States, 1988 to 2000: effects of provider caseloads and progressive centralization and specialization of care. Neurosurgery 54:553–563. https://doi.org/10.1227/01.neu.0000108421.69822.67; discussion 563–555
Norderhaug I, Krogstad U, Ingebrigtsen T, Soreide O, Wiseth R, Myhre HO (2007) The Influence of Hospital or Physician Volume on Quality of Health Care. Oslo, Norway
Davies JM, Ozpinar A, Lawton MT (2015) Volume-outcome relationships in neurosurgery. Neurosurg Clin N Am 26: 207–218, viii. https://doi.org/10.1016/j.nec.2014.11.015
Malone H, Cloney M, Yang J, Hershman DL, Wright JD, Neugut AI, Bruce JN (2018) Failure to Rescue and Mortality Following Resection of Intracranial Neoplasms. Neurosurgery 83:263–269. https://doi.org/10.1093/neuros/nyx354
Elixhauser A, Steiner C, Harris DR, Coffey RM (1998) Comorbidity measures for use with administrative data. Med Care 36:8–27
Moore BJ, White S, Washington R, Coenen N, Elixhauser A (2017) Identifying increased risk of readmission and in-hospital mortality using hospital administrative data: The AHRQ Elixhauser Comorbidity Index. Med Care 55:698–705. https://doi.org/10.1097/MLR.0000000000000735
Muhlestein WE, Akagi DS, Chotai S, Chambless LB (2017) The impact of race on discharge disposition and length of hospitalization after craniotomy for brain tumor. World Neurosurg 104:24–38. https://doi.org/10.1016/j.wneu.2017.04.061
Missios S, Bekelis K (2015) Drivers of hospitalization cost after craniotomy for tumor resection: creation and validation of a predictive model. BMC Health Serv Res 15:85. https://doi.org/10.1186/s12913-015-0742-2
Dumont TM, Tranmer BI, Horgan MA, Rughani AI (2012) Trends in neurosurgical complication rates at teaching vs nonteaching hospitals following duty-hour restrictions. Neurosurgery 71:1041–1046. https://doi.org/10.1227/NEU.0b013e31826cdd73; discussion 1046
Natarajan S, Lipsitz SR, Fitzmaurice GM, Sinha D, Ibrahim JG, Haas J, Gellad W (2012) An extension of the Wilcoxon Rank-Sum test for complex sample survey data. J R Stat Soc Ser C 61:653–664. https://doi.org/10.1111/j.1467-9876.2011.01028.x
Spall JC (2005) Monte Carlo Computation of the Fisher Information Matrix in Nonstandard Settings. J Comput Graph Stat 14:889–909. https://doi.org/10.1198/106186005X78800
Burke LG, Frakt AB, Khullar D, Orav EJ, Jha AK (2017) Association Between Teaching Status and Mortality in US Hospitals. JAMA 317:2105–2113. https://doi.org/10.1001/jama.2017.5702
Young JQ, Ranji SR, Wachter RM, Lee CM, Niehaus B, Auerbach AD (2011) "July effect": impact of the academic year-end changeover on patient outcomes: a systematic review. Ann Intern Med 155:309–315. https://doi.org/10.7326/0003-4819-155-5-201109060-00354
Khuri SF, Najjar SF, Daley J, Krasnicka B, Hossain M, Henderson WG, Aust JB, Bass B, Bishop MJ, Demakis J, DePalma R, Fabri PJ, Fink A, Gibbs J, Grover F, Hammermeister K, McDonald G, Neumayer L, Roswell RH, Spencer J, Turnage RH, Program VANSQI (2001) Comparison of surgical outcomes between teaching and nonteaching hospitals in the Department of Veterans Affairs. Ann Surg 234:370–382. https://doi.org/10.1097/00000658-200109000-00011; discussion 382–373
Ferraris VA, Harris JW, Martin JT, Saha SP, Endean ED (2016) Impact of residents on surgical outcomes in high-complexity procedures. J Am Coll Surg 222:545–555. https://doi.org/10.1016/j.jamcollsurg.2015.12.056
Hyder O, Sachs T, Ejaz A, Spolverato G, Pawlik TM (2013) Impact of hospital teaching status on length of stay and mortality among patients undergoing complex hepatopancreaticobiliary surgery in the USA. J Gastrointest Surg 17:2114–2122. https://doi.org/10.1007/s11605-013-2349-4
Hayanga AJ, Mukherjee D, Chang D, Kaiser H, Lee T, Gearhart S, Ahuja N, Freischlag J (2010) Teaching hospital status and operative mortality in the United States: tipping point in the volume-outcome relationship following colon resections? Arch Surg 145:346–350. https://doi.org/10.1001/archsurg.2010.24
Macedo FIB, Jayanthi P, Mowzoon M, Yakoub D, Dudeja V, Merchant N (2017) The impact of surgeon volume on outcomes after pancreaticoduodenectomy: a meta-analysis. J Gastrointest Surg 21:1723–1731. https://doi.org/10.1007/s11605-017-3498-7
Khandwala YS, Jeong IG, Kim JH, Han DH, Li S, Wang Y, Chang SL, Chung BI (2017) The impact of surgeon volume on perioperative outcomes and cost for patients receiving robotic partial nephrectomy. J Endourol 31:851–857. https://doi.org/10.1089/end.2017.0207
Kandil E, Noureldine SI, Abbas A, Tufano RP (2013) The impact of surgical volume on patient outcomes following thyroid surgery. Surgery 154:1346–1352. https://doi.org/10.1016/j.surg.2013.04.068; discussion 1352–1343
Barocas DA, Mitchell R, Chang SS, Cookson MS (2010) Impact of surgeon and hospital volume on outcomes of radical prostatectomy. Urol Oncol 28:243–250. https://doi.org/10.1016/j.urolonc.2009.03.001
Ihse I (2003) The volume-outcome relationship in cancer surgery: a hard sell. Ann Surg 238:777–781. https://doi.org/10.1097/01.sla.0000098616.19622.af
Brown DA, Himes BT, Major BT, Mundell BF, Kumar R, Kall B, Meyer FB, Link MJ, Pollock BE, Atkinson JD, Van Gompel JJ, Marsh WR, Lanzino G, Bydon M, Parney IF (2018) Cranial Tumor Surgical Outcomes at a High-Volume Academic Referral Center. Mayo Clin Proc 93:16–24. https://doi.org/10.1016/j.mayocp.2017.08.023
Davies JM, Lawton MT (2017) Improved outcomes for patients with cerebrovascular malformations at high-volume centers: the impact of surgeon and hospital volume in the United States, 2000–2009. J Neurosurg 127:69–80. https://doi.org/10.3171/2016.7.JNS15925
Kalakoti P, Missios S, Menger R, Kukreja S, Konar S, Nanda A (2015) Association of risk factors with unfavorable outcomes after resection of adult benign intradural spine tumors and the effect of hospital volume on outcomes: an analysis of 18, 297 patients across 774 US hospitals using the National Inpatient Sample (2002–2011). Neurosurg Focus 39:E4. https://doi.org/10.3171/2015.5.FOCUS15157
Barker FG 2nd, Klibanski A, Swearingen B (2003) Transsphenoidal surgery for pituitary tumors in the United States, 1996–2000: mortality, morbidity, and the effects of hospital and surgeon volume. J Clin Endocrinol Metab 88:4709–4719. https://doi.org/10.1210/jc.2003-030461
Anderson JE, Chang DC (2014) Does the effect of surgical volume on outcomes diminish over time? JAMA Surg 149:398–400. https://doi.org/10.1001/jamasurg.2013.4654
Kurian KM, Jenkinson MD, Brennan PM, Grant R, Jefferies S, Rooney AG, Bulbeck H, Erridge SC, Mills S, McBain C, McCabe MG, Price SJ, Marino S, Moyes E, Qian W, Waldman A, Vaqas B, Keatley D, Burchill P, Watts C (2018) Brain tumor research in the United Kingdom: current perspective and future challenges. A strategy document from the NCRI Brain Tumor CSG. Neurooncol Pract 5:10–17. https://doi.org/10.1093/nop/npx022
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This study was not funded by any source and all authors declare no conflict of interest.
Ethical approval
All procedures performed in the study were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments. Institutional Review Board (IRB) approval for the study was not necessary because all patient data with identifying information is stripped from the NIS repository.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Luther, E.M., McCarthy, D., Berry, K.M. et al. Hospital teaching status associated with reduced inpatient mortality and perioperative complications in surgical neuro-oncology. J Neurooncol 146, 389–396 (2020). https://doi.org/10.1007/s11060-020-03395-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-020-03395-x