Abstract
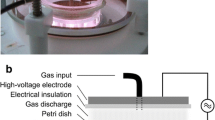
There is no definitive method to prevent Candida albicans (C. albicans) biofilm formation on polymethyl methacrylate (PMMA) surfaces. The objective of this study was to evaluate the effect of Helium plasma treatment (before the application of removable dentures to the patient) to prevent or reduce C. albicans ATCC 10,231 the anti-adherent activity, viability, and biofilm formation on PMMA surfaces. One hundred disc-shaped PMMA samples (2 mm × 10 mm) were prepared. The samples were randomly divided into 5 surface groups and treated with different concentrations of Helium plasma: G I: Control group (untreated), G II: 80% Helium plasma-treated group, G III: 85% Helium plasma-treated group, G IV: 90% Helium plasma-treated group, G V: 100% Helium plasma-treated group. C. albicans viability and biofilm formations were evaluated using 2 methods: MTT (3-(4,5-dimethyl thiazolyl-2)-2, 5-diphenyltetrazolium bromide) assays and Crystal Violet (CV) staining. The surface morphology and C. albicans biofilm images were observed with scanning electron microscopy. The Helium plasma-treated PMMA groups (G II, G III, G IV, G V) observed a significant reduction in C. albicans cell viability and biofilm formation compared with the control group. Treating PMMA surfaces with different concentrations of Helium plasma prevents C. albicans viability and biofilm formation. This study suggests that Helium plasma treatment might be an effective strategy in modifying PMMA surfaces to prevent denture stomatitis formation.



Similar content being viewed by others
Data Availability
Data is available upon request from the corresponding author.
References
Sun Y, et al. Inactivation of candida biofilms by non-thermal plasma and its enhancement for fungistatic effect of antifungal drugs. PLoS ONE. 2012;7(7):e40629.
Baba Y, et al. Effectiveness of a combination denture-cleaning method versus a mechanical method: comparison of denture cleanliness, patient satisfaction, and oral health-related quality of life. J Prosthodont Res. 2018;62(3):353–8.
de Castro DT, et al. Elemental ion release and cytotoxicity of antimicrobial acrylic resins incorporated with nanomaterial. Gerodontology. 2017;34(3):320–5.
An S, et al. Incorporation of antimicrobial agents in denture base resin: a systematic review. J Prosthet Dent. 2021;126(2):188–95.
Ahmad N, Jafri Z, Khan ZH. Evaluation of nanomaterials to prevent oral Candidiasis in PMMA based denture wearing patients. A systematic analysis. J Oral Biol Craniofac Res. 2020;10(2):189–93.
Al-Thobity AM, et al. In vitro evaluation of the inhibitory activity of thymoquinone in combatting Candida albicans in denture stomatitis prevention. Int J Environ Res Public Health. 2017;14(7):743.
Ali AA, Alharbi FA, Suresh C. Effectiveness of coating acrylic resin dentures on preventing candida adhesion. J Prosthodont. 2013;22(6):445–50.
Redding S, et al. Inhibition of Candida albicans biofilm formation on denture material. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2009;107(5):669–72.
Suganya S, et al. Evaluation and comparison of anti-Candida effect of heat cure polymethylmethacrylate resin enforced with silver nanoparticles and conventional heat cure resins: an in vitro study. Indian J Dent Res. 2014;25(2):204.
Bajunaid SO. How effective are antimicrobial agents on preventing the adhesion of Candida albicans to denture base acrylic resin materials? a systematic review. Polymers. 2022;14(5):908.
Anwander M, et al. Biofilm formation on denture base resin including ZnO, CaO, and TiO2 nanoparticles. J Adv Prosthodont. 2017;9(6):482–5.
Song Y, et al. Plasma inactivation of Candida albicans by an atmospheric cold plasma brush composed of hollow fibers. IEEE Trans Plasma Sci. 2012;40(4):1098–102.
Zamperini CA, et al. In vitro adhesion of Candida glabrata to denture base acrylic resin modified by glow-discharge plasma treatment. Mycoses. 2013;56(2):134–44.
Qian K, et al. Time-related surface modification of denture base acrylic resin treated by atmospheric pressure cold plasma. Dent Mater J. 2016;35(1):97–103.
Pan H, et al. Cold plasma-induced surface modification of heat-polymerized acrylic resin and prevention of early adherence of Candida albicans. Dent Mater J. 2015;34(4):529–36.
Yildirim AZ, et al. Effect of argon plasma and Er: YAG laser on tensile bond strength between denture liner and acrylic resin. J Prosthet Dent. 2020;124(6):799-e1.
Karakış D, Akay C, Pat S. Effect of argon plasma on the shear bond strength of Y-TZP zirconia ceramic resin interface. ECS J Solid State Sci Technol. 2021;10(5):051005.
Akay C, İsrafil N, Pat S. Enhancement of adhesive bonding properties of polyetheretherketone-based materials using plasma surface modifications. J Adhes Dent. 2022;24(1):117–24.
Zamperini CA, et al. Adherence in vitro of Candida albicans to plasma treated acrylic resin. Effect of plasma parameters, surface roughness and salivary pellicle. Arch Oral Biol. 2010;55(10):763–70.
Zamperini C, et al. Evaluation of fungal adherence to plasma-modified polymethylmethacrylate. Mycoses. 2011;54(5):e344–51.
Wang R, et al. Comparison between helium and argon plasma jets on improving the hydrophilic property of PMMA surface. Appl Surf Sci. 2016;367:401–6.
Akay C, et al. Evaluation of helium plasma surface modification on tensile bond strength of denture base materials: a scanning electron microscope study. ECS J Solid State Sci Technol. 2021;10(12):124002.
Al-Fouzan AF, Al-Mejrad LA, Albarrag AM. Adherence of Candida to complete denture surfaces in vitro: a comparison of conventional and CAD/CAM complete dentures. J Adv Prosthodont. 2017;9(5):402–8.
Jin Y, et al. Biofilm formation of Candida albicans is variably affected by saliva and dietary sugars. Arch Oral Biol. 2004;49(10):789–98.
Krom BP, et al. Optimized candidal biofilm microtiter assay. J Microbiol Methods. 2007;68(2):421–3.
Kong F, et al. Antifungal activity of magnesium oxide nanoparticles: effect on the growth and key virulence factors of Candida albicans. Mycopathologia. 2020;185:485–94.
Marcos-Zambrano LJ, et al. Production of biofilm by Candida and non-Candida spp. isolates causing fungemia: comparison of biomass production and metabolic activity and development of cut-off points. Int J Med Microbiol. 2014;304(8):1192–8.
Weerasekera MM, et al. Culture media profoundly affect Candida albicans and Candida tropicalis growth, adhesion and biofilm development. Mem Inst Oswaldo Cruz. 2016;111:697–702.
Pathak AK, Sharma S, Shrivastva P. Multi-species biofilm of Candida albicans and non-Candida albicans Candida species on acrylic substrate. J Appl Oral Sci. 2012;20:70–5.
Dhanasekaran D, et al. Human dental biofilm: screening, characterization, in vitro biofilm formation and antifungal resistance of Candida spp. Saudi J Dent Res. 2014;5(1):55–70.
Kojic EM, Darouiche RO. Candida infections of medical devices. Clin Microbiol Rev. 2004;17(2):255–67.
Henriques M, Williams D. Pathogenesis and virulence of Candida albicans and Candida glabrata. Pathogens. 2020;9:752.
Hong, Q., et al. plasma treatment effects on oral candida albicans biofilms. Dent Oral Biol Craniofac Res. 2021; 4(2).
Kerlikowski A, et al. Effects of cold atmospheric pressure plasma and disinfecting agents on Candida albicans in root canals of extracted human teeth. J Biophotonics. 2020;13(12):e202000221.
Hahnel S, et al. In vitro evaluation of artificial ageing on surface properties and early Candida albicans adhesion to prosthetic resins. J Mater Sci Mater Med. 2009;20(1):249–55.
Maillet C, et al. Non-thermal O2 plasma efficacy on C. albicans and its effect on denture base resin color. Appl Sci. 2021;11(21):10367.
Acknowledgements
This research was previosly presented as an oral presentation at the 9th International Academic Studies Conference, 3-5 August 2022 (Online). We thanks to ‘Advanced Material Technologies Application and Research Center’ for their support and contribution.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed Consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Handling Editor: Damien Costa.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Avukat, E.N., Akay, C., Topcu Ersöz, M.B. et al. Could Helium Plasma Treatment be a Novel Approach to Prevent the Biofilm Formation of Candida albicans?. Mycopathologia 188, 361–369 (2023). https://doi.org/10.1007/s11046-023-00747-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-023-00747-9