Abstract
Background
The epidemiology of invasive aspergillosis (IA) in patients with acute lymphoid leukemia (ALL) has not been well characterized.
Objectives
To identify potential peculiarities in the natural history, treatment response and outcome of IA diagnosed in patients with ALL and AML.
Methods
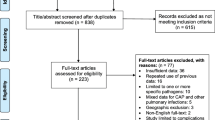
This is a retrospective cohort study conducted in seven tertiary-care hospitals between 2009 and 2017 of all consecutive episodes of IA occurring in adult patients with acute leukemia. Demographic characteristics, underlying disease and recent treatment, antifungal prophylaxis, neutropenia, receipt of corticosteroids, clinical and radiological findings, mycological results, antifungal therapy, and 6-week and 12-week survival were recorded.
Results
We identified 77 cases of IA in 54 patients with AML and 23 patients with ALL. The majority of patients developed IA in the context of induction chemotherapy for newly diagnosed (48.0%) or relapsed (41.6%) leukemia, with no differences between ALL and AML. Lung involvement was more frequent in AML (96.3% vs. 82.6%, p = 0.06) and rhinosinusitis was more common in ALL (43.5% vs. 24.1%, p = 0.09). Galactomannan was the microbiologic documentation of IA in 76.6%, with similar patterns of positivity in AML and ALL. The 6-week survival of IA in patients with AML and ALL was 63.0% and 56.5%, respectively (p = 0.60).
Conclusions
The epidemiology, clinical presentation, diagnosis and outcome of IA in ALL patients are similar to patients with AML.
Similar content being viewed by others
References
Nucci M, Garnica M, Gloria AB, Lehugeur DS, Dias VC, Palma LC, Cappellano P, Fertrin KY, Carlesse F, Simoes B, Bergamasco MD, Cunha CA, Seber A, Ribeiro MP, Queiroz-Telles F, Lee ML, Chauffaille ML, Silla L, de Souza CA, Colombo AL. Invasive fungal diseases in haematopoietic cell transplant recipients and in patients with acute myeloid leukaemia or myelodysplasia in Brazil. Clin Microbiol Infect. 2013;19:745–51. https://doi.org/10.1111/1469-0691.12002.
Pagano L, Caira M, Candoni A, Offidani M, Fianchi L, Martino B, Pastore D, Picardi M, Bonini A, Chierichini A, Fanci R, Caramatti C, Invernizzi R, Mattei D, Mitra ME, Melillo L, Aversa F, Van Lint MT, Falcucci P, Valentini CG, Girmenia C, Nosari A. The epidemiology of fungal infections in patients with hematologic malignancies: the SEIFEM-2004 study. Haematologica. 2006;91:1068–75. https://doi.org/10.3324/haematol.2009.012054.
Nucci M, Anaissie E. How we treat invasive fungal diseases in patients with acute leukemia: the importance of an individualized approach. Blood. 2014;124:3858–69. https://doi.org/10.1182/blood-2014-04-516211.
Cornely OA, Leguay T, Maertens J, Vehreschild MJGT, Anagnostopoulos A, Castagnola C, Verga L, Rieger C, Kondakci M, Harter G, Duarte RF, Allione B, Cordonnier C, Heussel CP, Morrissey CO, Agrawal SG, Donnelly JP, Bresnik M, Hawkins MJ, Garner W, Gokbuget N. Randomized comparison of liposomal amphotericin B versus placebo to prevent invasive mycoses in acute lymphoblastic leukaemia. J Antimicrob Chemother. 2017;72:2359–67. https://doi.org/10.1093/jac/dkx133.
Souza L, Nouer SA, Morales H, Simoes B, Solza C, Queiroz-Telles F, Nucci M. Epidemiology of invasive fungal disease in haematologic patients. Mycoses. 2021;64:252–6. https://doi.org/10.1111/myc.13205.
Cattaneo C, Gramegna D, Malagola M, Pagani C, Borlenghi E, Cerqui E, Passi A, Sciume M, Bernardi S, Crippa C, Dalceggio D, Carbone C, Pelizzari AM, Re A, Russo D, Rossi G. Invasive pulmonary aspergillosis in acute leukemia: a still frequent condition with a negative impact on the overall treatment outcome. Leuk Lymphoma. 2019;60:3044–50. https://doi.org/10.1080/10428194.2019.1613535.
Wang SS, Kotecha RS, Bernard A, Blyth CC, McMullan BJ, Cann MP, Yeoh DK, Bartlett AW, Ryan AL, Moore AS, Bryant PA, Clark J, Haeusler GM. Invasive fungal infections in children with acute lymphoblastic leukaemia: results from four Australian centres, 2003–2013. Pediatr Blood Cancer. 2019;66:e27915. https://doi.org/10.1002/pbc.27915.
Kontoyiannis DP, Marr KA, Park BJ, Alexander BD, Anaissie EJ, Walsh TJ, Ito J, Andes DR, Baddley JW, Brown JM, Brumble LM, Freifeld AG, Hadley S, Herwaldt LA, Kauffman CA, Knapp K, Lyon GM, Morrison VA, Papanicolaou G, Patterson TF, Perl TM, Schuster MG, Walker R, Wannemuehler KA, Wingard JR, Chiller TM, Pappas PG. Prospective surveillance for invasive fungal infections in hematopoietic stem cell transplant recipients, 2001–2006: overview of the Transplant-Associated Infection Surveillance Network (TRANSNET) Database. Clin Infect Dis. 2010;50:1091–100. https://doi.org/10.1086/651263.
Hsu LY, Lee DG, Yeh SP, Bhurani D, Khanh BQ, Low CY, Norasetthada L, Chan T, Kwong YL, Vaid AK, Alejandria I, Mendoza M, Chen CY, Johnson A, Tan TY. Epidemiology of invasive fungal diseases among patients with haematological disorders in the Asia-Pacific: a prospective observational study. Clin Microbiol Infect. 2015;21:594–611. https://doi.org/10.1016/j.cmi.2015.02.019.
Hoenigl M, Zollner-Schwetz I, Sill H, Linkesch W, Lass-Florl C, Schnedl WJ, Krause R. Epidemiology of invasive fungal infections and rationale for antifungal therapy in patients with haematological malignancies. Mycoses. 2011;54:454–9. https://doi.org/10.1111/j.1439-0507.2010.01881.x.
Girmenia C, Raiola AM, Piciocchi A, Algarotti A, Stanzani M, Cudillo L, Pecoraro C, Guidi S, Iori AP, Montante B, Chiusolo P, Lanino E, Carella AM, Zucchetti E, Bruno B, Irrera G, Patriarca F, Baronciani D, Musso M, Prete A, Risitano AM, Russo D, Mordini N, Pastore D, Vacca A, Onida F, Falcioni S, Pisapia G, Milone G, Vallisa D, Olivieri A, Bonini A, Castagnola E, Sica S, Majolino I, Bosi A, Busca A, Arcese W, Bandini G, Bacigalupo A, Rambaldi A, Locasciulli A. Incidence and outcome of invasive fungal diseases after allogeneic stem cell transplantation: a prospective study of the Gruppo Italiano Trapianto Midollo Osseo (GITMO). Biol Blood Marrow Transplant. 2014;20:872–80. https://doi.org/10.1016/j.bbmt.2014.03.004.
Del Principe MI, Dragonetti G, Conti A, Verga L, Ballanti S, Fanci R, Candoni A, Marchesi F, Cattaneo C, Lessi F, Fracchiolla N, Spolzino A, Prezioso L, Delia M, Potenza L, Decembrino N, Castagnola C, Nadali G, Picardi M, Zama D, Orciulo E, Veggia B, Garzia M, Dargenio M, Melillo L, Manetta S, Russo D, Mancini V, Piedimonte M, Tisi MC, Toschi N, Busca A, Pagano L, behalf of the Sg, SorveglianzaEpidemiologicaInfezioninelleEmopatie g. Invasive aspergillosis in relapsed/refractory acute myeloid leukaemia patients: results from SEIFEM 2016-B survey. Mycoses. 2022;65:171–7. https://doi.org/10.1111/myc.13384.
Candoni A, Farina F, Perruccio K, Di BR, Criscuolo M, Cattaneo C, Delia M, Zannier ME, Dragonetti G, Fanci R, Martino B, Del Principe MI, Fianchi L, Vianelli N, Chierichini A, Garzia M, Petruzzellis G, Nadali G, Verga L, Busca A, Pagano L. Impact of invasive aspergillosis occurring during first induction therapy on outcome of acute myeloid leukaemia (SEIFEM-12B study). Mycoses. 2020;63:1094–100. https://doi.org/10.1111/myc.13147.
Rodriguez-Veiga R, Montesinos P, Boluda B, Lorenzo I, Martinez-Cuadron D, Salavert M, Peman J, Calvillo P, Cano I, Acuna E, Villalba A, Pinana JL, Sanz J, Solves P, Senent L, Vicente A, Sempere A, Cervera J, Barragan E, Jarque I, Torres A, Sanz MA, Sanz GF. Incidence and outcome of invasive fungal disease after front-line intensive chemotherapy in patients with acute myeloid leukemia: impact of antifungal prophylaxis. Ann Hematol. 2019;98:2081–8. https://doi.org/10.1007/s00277-019-03744-5.
Pagano L, Caira M, Candoni A, Offidani M, Martino B, Specchia G, Pastore D, Stanzani M, Cattaneo C, Fanci R, Caramatti C, Rossini F, Luppi M, Potenza L, Ferrara F, Mitra ME, Fadda RM, Invernizzi R, Aloisi T, Picardi M, Bonini A, Vacca A, Chierichini A, Melillo L, de Waure C, Fianchi L, Riva M, Leone G, Aversa F, Nosari A. Invasive aspergillosis in patients with acute myeloid leukemia: a SEIFEM-2008 registry study. Haematologica. 2010;95:644–50. https://doi.org/10.3324/haematol.2009.012054.
Donnelly JP, Chen SC, Kauffman CA, Steinbach WJ, Baddley JW, Verweij PE, Clancy CJ, Wingard JR, Lockhart SR, Groll AH, Sorrell TC, Bassetti M, Akan H, Alexander BD, Andes D, Azoulay E, Bialek R, Bradsher RW, Bretagne S, Calandra T, Caliendo AM, Castagnola E, Cruciani M, Cuenca-Estrella M, Decker CF, Desai SR, Fisher B, Harrison T, Heussel CP, Jensen HE, Kibbler CC, Kontoyiannis DP, Kullberg BJ, Lagrou K, Lamoth F, Lehrnbecher T, Loeffler J, Lortholary O, Maertens J, Marchetti O, Marr KA, Masur H, Meis JF, Morrisey CO, Nucci M, Ostrosky-Zeichner L, Pagano L, Patterson TF, Perfect JR, Racil Z, Roilides E, Ruhnke M, Prokop CS, Shoham S, Slavin MA, Stevens DA, Thompson GR, Vazquez JA, Viscoli C, Walsh TJ, Warris A, Wheat LJ, White PL, Zaoutis TE, Pappas PG. Revision and update of the consensus definitions of invasive fungal disease from the European organization for research and treatment of cancer and the mycoses study group education and research consortium. Clin Infect Dis. 2020;71:1367–76. https://doi.org/10.1093/cid/ciz1008.
Girmenia C, Micozzi A, Piciocchi A, Gentile G, Di CL, Nasso D, Minotti C, Capria S, Cartoni C, Alimena G, Meloni G, Amadori S, Foa R, Venditti A. Invasive fungal diseases during first induction chemotherapy affect complete remission achievement and long-term survival of patients with acute myeloid leukemia. Leuk Res. 2014;38:469–74. https://doi.org/10.1016/j.leukres.2014.01.007.
Nicolato A, Nouer SA, Garnica M, Portugal R, Maiolino A, Nucci M. Invasive fungal diseases in patients with acute lymphoid leukemia. Leuk Lymphoma. 2016;57:2084–9. https://doi.org/10.3109/10428194.2016.1154957.
Delliere S, Dannaoui E, Fieux M, Bonfils P, Gricourt G, Demontant V, Podglajen I, Woerther PL, Angebault C, Botterel F. Analysis of microbiota and mycobiota in fungal ball rhinosinusitis: specific interaction between aspergillus fumigatus and haemophilus influenza? J Fungi (Basel). 2021. https://doi.org/10.3390/jof7070550.
Candoni A, Klimko N, Busca A, Di Blasi R, Shadrivova O, Cesaro S, Zannier ME, Verga L, Forghieri F, Calore E, Nadali G, Simonetti E, Muggeo P, Quinto AM, Castagnola C, Cellini M, Del Principe MI, Fracchiolla N, Melillo L, Piedimonte M, Zama D, Farina F, Giusti D, Mosna F, Capelli D, Delia M, Picardi M, Decembrino N, Perruccio K, Vallero S, Aversa F, Fanin R, Pagano L, Group S. Fungal infections of the central nervous system and paranasal sinuses in onco-haematologic patients. Epidemiological study reporting the diagnostic-therapeutic approach and outcome in 89 cases. Mycoses. 2019;62:252–60. https://doi.org/10.1111/myc.12884.
Patterson TF, Thompson GR III, Denning DW, Fishman JA, Hadley S, Herbrecht R, Kontoyiannis DP, Marr KA, Morrison VA, Nguyen MH, Segal BH, Steinbach WJ, Stevens DA, Walsh TJ, Wingard JR, Young JA, Bennett JE. Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the infectious diseases society of America. Clin Infect Dis. 2016;63:e1–60. https://doi.org/10.1093/cid/ciw326.
Herbrecht R, Denning DW, Patterson TF, Bennett JE, Greene RE, Oestmann JW, Kern WV, Marr KA, Ribaud P, Lortholary O, Sylvester R, Rubin RH, Wingard JR, Stark P, Durand C, Caillot D, Thiel E, Chandrasekar PH, Hodges MR, Schlamm HT, Troke PF, de Pauw B, Invasive Fungal Infections Group of the European Organisation for R, Treatment of C, The Global Aspergillus Study G. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med. 2002;347:408–15. https://doi.org/10.1056/NEJMoa020191.
Denning DW. Therapeutic outcome in invasive aspergillosis. Clin Infect Dis. 1996;23:608–15. https://doi.org/10.1093/clinids/23.3.608.
Lin SJ, Schranz J, Teutsch SM. Aspergillosis case-fatality rate: systematic review of the literature. Clin Infect Dis. 2001;32:358–66. https://doi.org/10.1086/318483.
Nucci M, Nouer SA, Grazziutti M, Kumar NS, Barlogie B, Anaissie E. Probable invasive aspergillosis without prespecified radiologic findings: proposal for inclusion of a new category of aspergillosis and implications for studying novel therapies. Clin Infect Dis. 2010;51:1273–80. https://doi.org/10.1086/657065.
Bergamasco MD, Pereira CAP, Arrais-Rodrigues C, Ferreira DB, Baiocchi O, Kerbauy F, Nucci M, Colombo AL. Epidemiology of invasive fungal diseases in patients with hematologic malignancies and hematopoietic cell transplantation recipients managed with an antifungal diagnostic driven approach. J Fungi (Basel). 2021. https://doi.org/10.3390/jof7080588.
Acknowledgements
We would like to thank Natacha Cerchiari and Jeronimo Gerolin in the support to the data collection process. We thank COLSAN-Associaçao Beneficiente de Coleta de Sangue for the administration and accountability of the Pfizer Grant.
Funding
This work was supported by Pfizer Inc.
Author information
Authors and Affiliations
Contributions
ALC and MN designed the study, analyzed the data and wrote the paper; MDB, SAN, PTOC, ACP, FQT, EA, JFR and DRF performed the research and collected data.
Corresponding authors
Ethics declarations
Conflict of interest
Arnaldo L. Colombo (ALC) has received an Independent Investigator Grant Initiative from Pfizer that partially supported the present study. ALC also received educational grants and travel support for scientific meetings from Biotoscana-Knight, Eurofarma, United Medical, and Pfizer. Alessandro C. Pasqualotto (ACP) has received research grants from Pfizer, Gilead, and MSD. He has given paid talks and received honoraria on behalf of Pfizer, Gilead, IMMY, United Medical, MSD, Astellas, and Teva. Paulo de Tarso Oliveira e Castro has received educational grants and travel support for scientific meetings from United Medical, and Pfizer. Diego R. Falci (DRF) has received research support, payment for lectures and consulting fees from United Medical, Gilead, Astellas, MSD, IMMY and Pfizer, not related to this work. Jessica F. Ramos (JFR) has received research support, payment for lectures and consulting fees from Biotoscana-Knight, Merck Sharp and Dohme and Pfizer, not related to this work. Edson Abdala has received educational grants and travel support for scientific meetings from Biotoscana-Knight, United Medical, Abbott, Teva, MSD, Roche and Pfizer. Marcio Nucci has received honoraria for consulting and lectures from MSD, Teva, Knight, Pfizer, F2G, Takeda, Cidara, Gilead, Janssen, Abbvie, Basilea, Astellas, Abbott and Amgen. All other authors have nothing to disclose.
Ethical Approval
This study was performed in line with the principles of the Declaration of Helsinki and approved by the Ethical Committees of each participating center. Waiver of informed consent was granted by the ethical committees.
Additional information
Handling Editor: Martin Hoenigl.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Colombo, A.L., Bergamasco, M.D., Nouér, S.A. et al. Invasive Aspergillosis in Patients with Acute Leukemia: Comparison Between Acute Myeloid and Acute Lymphoid Leukemia. Mycopathologia 188, 1–8 (2023). https://doi.org/10.1007/s11046-022-00684-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-022-00684-z