Abstract
Talaromycosis is a life-threatening fungal disease commonly seen in patients with acquired immunodeficiency syndrome (AIDS), which is endemic in Southern China and Southeast countries. The diagnostic methods available for talaromycosis are relatively time-consuming and yield a high mortality. Therefore, early diagnosis of talaromycosis is extremely important. We aimed to determine a potential method for assisting in its early diagnosis. A total of 283 patients with AIDS admitted to our hospital were prospectively included in this cross-sectional study and divided into those with Talaromyces marneffei (TSM group, n = 93) and those without Talaromyces marneffei (non-TSM group, n = 190). The diagnostic accuracy of the Mp1p enzyme immunoassay (EIA), galactomannan (GM) assay, and blood culture performed within 3 days of hospitalisation were evaluated, using talaromycosis confirmed by culture and/or pathology as the gold standard. The positivity rates in the Mp1p EIA, GM assay, and blood culture were 72%, 64.5%, and 81.7%, respectively, in the TSM group. The sensitivity, specificity, and positive and negative predictive values of the Mp1p EIA were 72.0% (67/93), 96.8% (184/190), 91.8% (67/73), and 87.6% (184/210), respectively. The Mp1p EIA showed a substantial agreement with the gold standard (kappa: 0.729) and superiority to the GM assay (kappa: 0.603); it also showed a superior diagnostic accuracy in the patients with CD4+ counts of < 50 cells/µL compared to those with CD4+ counts ranged from 50–100 cells/µL. The Mp1p EIA has the advantage of assisting in the early diagnosis of talaromycosis in patients with AIDS, especially those with low CD4+ counts.
Similar content being viewed by others
Introduction
Talaromycosis is an invasive fungal disease caused by Talaromyces marneffei (T. marneffei), which is common in immunocompromised individuals, especially in patients with acquired immunodeficiency syndrome (AIDS). Most cases of talaromycosis occur in individuals with CD4+ counts < 100 cells/µL [1]. A previous study found that a low CD4+ count is a risk factor for talaromycosis, especially if the CD4+ count is < 50 cells/µL [2]. It is mainly prevalent in Southern China and Southeast countries, including Thailand, Vietnam, India, and Malaysia [3,4,5,6,7]. In Southern China, the prevalence of talaromycosis in hospitalized patients with AIDS has increased by 65% within 5 years [8]. Talaromycosis is a life-threatening disease with a high mortality rate of up to 50.6% without timely antifungal treatment [6, 9, 10]. Delayed diagnosis of talaromycosis is an important reason for its high mortality rate [10, 11]. For every day of delay in the diagnosis of talaromycosis, the risk of death increases by 2% [11]. Therefore, early diagnosis of talaromycosis is extremely important.
However, its early diagnosis is difficult. At present, the definite diagnosis of talaromycosis relies on histopathology or culture evidence of T. marneffei infection [1, 12], which has significant limitations. It is relatively time-consuming, with culture of pathogens requiring approximately 1 to 2 weeks [1, 4, 10]. In addition, such diagnostic methods usually require invasive examinations to improve the positivity rate. Therefore, new methods are urgently needed for the early diagnosis of talaromycosis.
Previous studies have developed a range of new technologies; however, none of them have been proven for clinical use [2, 11, 13,14,15,16,17,18,19]. Using standard fungus culture as the gold standard, a meta-analysis of 26 diagnostic accuracy studies of rapid diagnosis using methods such as polymerase chain reaction (PCR) and enzyme-linked immunosorbent assay (ELISA), found that the sensitivity and specificity for the early diagnosis of talaromycosis were 82% (95% confidence interval [CI] 68%–90%) and 99% (95% CI 98%–100%), respectively [19]. Serological testing is an adjunct to a rapid diagnosis. Galactomannan (GM) is a polysaccharide antigen that occurs primarily in the cell walls of Aspergillus and Talaromyces species [20]. The Aspergillus galactomannan (GM) assay is widely used in clinical practice to assist with the diagnosis of aspergillosis. It cross-reacts with Talaromyces GM, which limits its clinical application. However, as the prevalence of aspergillosis in patients with AIDS is very low, especially relative to talaromycosis. Aspergillus GM assays can assist with the diagnosis of talaromycosis in patients with AIDS, with a sensitivity of 95.8% (23/24) and a specificity of 90.9% (30/33) [11, 20]. Mp1p is a type of mannoprotein contained in the T. marneffei cell wall, which is secreted into the blood of individuals with T. marneffei infection [21]. It is a key virulence factor in T. marneffei infection, and has been shown to be highly immunogenic [21, 22]. Using positive cultures from blood, bone marrow, and other body fluids as the gold standard, preliminary studies found that, serum/plasma Mp1p antigen detection had a sensitivity of 75–86.3% and a specificity of 98–99% for the diagnosis of talaromycosis [15, 16], and that paired plasma and urine testing could improve the diagnostic accuracy [16]. The Mp1p enzyme immunoassay kit is commercially available, and has shown to be non-cross-reactive with common pathogenic fungi including Cryptococcus, Candida, Aspergillus, and Histoplasma species [15, 23]. Therefore, serum Mp1p antigen detection has the potential for use as a rapid diagnostic method in patients with AIDS [24]. However, the early diagnostic accuracy of Mp1p antigen detection in actual clinical settings remains unclear. The aim of our real-world study was to assess the diagnostic accuracy of Mp1p antigen detection for talaromycosis in patients with AIDS within 3 days of admission, thus determining a potential method for assisting in the early diagnosis of talaromycosis in these patients.
Materials and methods
Study design
This was a cross-sectional study with participants recruited prospectively. We continuously enrolled antiretroviral therapy (ART)-naïve patients with AIDS hospitalised in the Guangzhou Eighth People’s Hospital (GEPH) between March and September 2018 with suspected opportunistic infections. All patients underwent serum GM test using the Platelia Aspergillus enzyme immunoassay kit (Bio-Rad, Marnes-la-Coquette, France), serum Mp1p antigen assay using an enzyme‐linked immunosorbent assay (ELISA) kit (Wantai Technologies, Beijing, China), and blood culture using standard automated aerobic BACTEC bottles, within 3 days of hospitalisation. All participants provided written informed consent. During their hospitalisation, some patients received cultures and/or histopathological examination from suspected foci of infection through invasive examinations. The case group, named the “Talaromyces marneffei (TSM) group”, included all patients with AIDS with culture- and/or pathology-confirmed talaromycosis. The control group, named the “non-TSM group”, included patients with AIDS who were diagnosed with tumours or opportunistic infections (OIs) other than talaromycosis, including candidiasis, tuberculosis, viral infections, Pneumocystis jirovecii pneumonia, cryptococcosis, and infection with other filamentous fungi (Table S1). The results of the tests in the two groups were used to evaluate the diagnostic accuracy. As the prevalence of talaromycosis differed according to CD4+ count in previous studies [1, 2], we also assessed the diagnostic accuracy in subgroup analyses stratified by the CD4+ count. Ethical approval was provided by the Medical Ethics Committee of the GEPH (Approval No. 202034167). All patients signed an informed consent form. The flow diagram of the study design is shown in Fig. 1.
Inclusion and Exclusion Criteria
The inclusion criteria were as follows: (1) confirmed HIV infection on HIV antibody or HIV nucleic acid testing; (2) age of 18 years or over; (3) CD4+ count of ≤ 200 cells/µL; (4) antiretroviral therapy-naïvety; (5) history of blood culture, serum Mp1p antigen detection, and Platelia Aspergillus GM detection within 3 days of admission; and 6) admission to the hospital because of suspected OIs. The exclusion criteria were as follows: (1) pregnancy or lactation; (2) incomplete clinical data; and (3) hospital stay duration of less than 3 days.
Mp1p Antigen Test in the Serum Samples
Serum samples were obtained from the enrolled patients within 3 days of admission. A double-antibody sandwich ELISA (DAS-ELISA) was used for the detection of Mp1p antigen. Mp1p antigen testing kits were purchased from Wantai (Wantai Mp1p antigen ELISA; Wantai Biological Pharmacy Enterprise Co. Ltd., Beijing, China). The Mp1p protein was produced using the Pichia pastoris expression system. The details of the raw materials have been reported elsewhere [15, 25]. The assay was performed according to the manufacturer’s instructions. Here, we briefly describe the steps. The serum samples were thawed to room temperature at 25 °C. Twenty microlitres of biotin reagent and fifty microlitres of serum specimen were added to the microplate (pre-coated rabbit anti-Mp1p polyclonal antibody) and incubated at 37 °C for 30 min. The plates were washed for five times and dried, and 100 µL of biotinylated mouse anti-Mp1p monoclonal antibody was added and incubated at 37 °C for 30 min. The plates were washed for five times and dried; chromogenic agent A (50 µL) and chromogenic agent B (50 µL) were added to each well; and the plates were incubated at 37 °C for 15 min and protected from light. After the addition of 50 µL of stopping solution to each well, the absorbance (A) at 450 nm was read using a microplate reader. The cut-off value was 0.1 plus the average of negative control wells. Samples were considered positive if the value was greater than or equal to the cut-off value, and negative if the value was below the cut-off value.
Platelia Aspergillus GM Detection
The GM antigen was detected using double-antibody sandwich enzyme-linked immunoassay following the manufacturer’s instructions (Bio-Rad). The experimental methods are described in a previously published article [26]. An absorbent index of ≥ 0.5 was considered to indicate positivity for the GM antigen.
Diagnosis of Talaromycosis
The gold standard for diagnosis of talaromycosis was T. marneffei infection confirmed by specimen culture and/or histopathological examination of clinically suspected foci of infection, according to the guidelines for the prevention and treatment of opportunistic infections [1]. Patients underwent blood culture according to the requirements specified in the study protocol. Invasive tests were performed only when the patient had a clinically suspected specific focus of infection and provided informed consent.
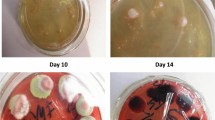
Talaromyces marneffei was isolated using standard culture techniques. In standard Sabouraud dextrose agar, T. marneffei grew more readily than did other endemic dimorphic fungi. T. marneffei was cultured as a mould at 25 °C to 30 °C and made a transition from mycelium to yeast at 32 °C to 37 °C. Identification was based on the morphological and microscopic observation of the colonies, demonstration of mould-to-yeast conversion, and presence of a red diffusible pigment production at 25 °C. Histopathological diagnosis was based on the identification of characteristic yeast cells with a midline septum in the tissue sections [1, 8].
Data Collection and Definitions
Data were collected from the patients’ electronic medical records. The demographic data included age and sex. Young adult was defined as age 18 − 44 years; middle-age adult was defined as age 45−59 years; and old adult was defined as age ≥ 60 years. The clinical data included signs and symptoms on admission, laboratory test results within 3 days of admission, and all diagnostic information on OIs and tumours. All data were double-checked by two trained research assistants before analysis.
The laboratory test indicators included the white blood cell (WBC) count, platelet (PLT) count, and haemoglobin (Hb), aspartate aminotransferase (AST), alanine aminotransferase (ALT), albumin, blood urea nitrogen, and creatinine levels. Leucopaenia was defined as a WBC count of < 3.5 × 109 cells/L; thrombocytopaenia, PLT count of < 125 × 109 cells/L; and anaemia, Hb level of < 120 g/L for men and < 110 g/L for women. A FACSCanto™ II flow cytometer was used to analyse CD4+ lymphocytes in the blood samples.
OIs were defined as infections caused by conditional pathogens not harmful to healthy populations but to immunodeficient populations. The presence of T. marneffei infection was based on cultures and/or pathology of suspected foci of infection, including blood, bone marrow, bronchoalveolar lavage fluid (BALF), rash, or other infected foci.
Statistical Analysis
All statistical analyses were performed using SPSS version 25.5. The continuous variables were expressed as medians and interquartile ranges (IQRs) and the categorical variables as numbers and percentages. The Wilcoxon rank-sum test was used for the continuous variables and the chi-squared test for the categorical variables. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and kappa value were calculated to evaluate the diagnostic accuracy of Mp1p antigen detection and other diagnostic methods. The statistical significance level was set at a two-tailed P value of < 0.05.
Results
Baseline Characteristics
A total of 283 patients with AIDS were enrolled in this study, including 93 patients with talaromycosis and 190 patients without talaromycosis. Histopathological examination was performed in 23 (24.7%) and 46 (24.2%) patients in the TSM and non-TSM groups, respectively. Of the study participants, most of the patients were men (n = 243 [85.9%]), young (age 18−44 years, n = 148 [52.3%]), or middle-aged (age 45−59 years, n = 96 [33.9%]). The median CD4+ count was 25 [IQR 9–64] cells/µL, and 194 (68.6%) patients had a CD4+ count of < 50 cells/µL. The prevalence of talaromycosis increased as the CD4+ count decreased, and none of the patients with a CD4+ count > 100 cells/µL were diagnosed with talaromycosis. The TSM group had a higher proportion of young adults (65.6% vs 45.8%, P = 0.002) and a higher incidence of fever, cough, sputum, rash, hepatomegaly, splenomegaly, and lymphadenectasis than the non-TSM group (all P < 0.05). The TSM group also had a lower CD4+ count (12 [IQR 6–27] vs. 40 [IQR 16–87] cells/µL, P < 0.001), and a higher incidence of abnormal laboratory test results, including a higher prevalence of leucopaenia, thrombocytopaenia, and anaemia, higher ALT level, and AST level (all P < 0.05) (Table 1), than the non-TSM group. The incidence of most OIs (including candidiasis, CMV/HSV infection, Pneumocystis jirovecii pneumonia, cryptococcosis, infection with other filamentous fungi, and Toxoplasma gondii infection) was similar between the two groups, except for a higher incidence of tuberculosis in the non-TSM group (18.9% vs. 6.5%, P = 0.005) (Table S1).
Detection Results of the Different Methods
In the total population, the positivity rates in the Mp1p and GM assays (25.8% and 26.1%, respectively) were similar to that in the blood culture (26.9%). More than a third of the patients were positive for “Mp1p + GM” (Fig. 2a). In the TSM group, the positivity rate for “Mp1p + GM” was 82.8%. The positivity rate in the Mp1p assay was similar to that in the blood culture (72% vs 81.7%, P = 0.122), while the positivity rate in the GM assay was lower than that in the blood culture (64.5% vs 81.7%, P = 0.002) (Table S2 and Fig. 2b). In the non-TSM group, 6 patients had positive results on the Mp1p assay, none of whom were diagnosed with a fungal infection (Table S4).
Positivity rates in the different diagnostic methods among the patients with AIDS. a All study participants with AIDS who were diagnosed with talaromycosis, other OIs or tumours; b Patients with AIDS who were diagnosed with talaromycosis. AIDS acquired immunodeficiency syndrome, OIs opportunistic infections, GM galactomannan, Mp1p+GM Mp1p antigen-positive or GM antigen-positive
Among all study participants, the positivity rates for Mp1p, GM, and “Mp1p+GM” in those with CD4+ counts of < 50 cells/µL were significantly higher than the positivity rates in those with CD4+ counts of 50–100 cells/µL (Fig. 3a). In the TSM group, the positivity rates for Mp1p, GM, “Mp1p+GM” and blood culture in those with CD4+ counts of < 50 cells/µL were 74.1%, 65.9%, 84.7%, and 82.4%, respectively, while the positivity rates for Mp1p, GM, “Mp1p+GM,” and blood culture in those with CD4+ counts of 50–100 cells/µL were 50%, 50%, 62.5%, and 75%, respectively (Table S3 and Fig. 3b).
Positivity rates according to the diagnostic method among the patients with AIDS in the different CD4+ count subgroupings. a Total patients with AIDS who were diagnosed with talaromycosis, other OIs or tumours, b Patients with AIDS who were diagnosed with talaromycosis. AIDS acquired immunodeficiency syndrome, OIs opportunistic infections, GM galactomannan, Mp1p+GM Mp1p antigen-positive or GM antigen-positive
Diagnostic Accuracy of the Mp1p Assay for Talaromycosis
For the diagnosis of talaromycosis in the patients with AIDS, the sensitivity, specificity, PPV, NPV, and kappa value of the Mp1p assay were 72.0% (67/93), 96.8% (184/190), 91.8% (67/73), 87.6% (184/210), and 0.729, respectively; the sensitivity, specificity, PPV, NPV, and kappa value of the GM assay were 64.5% (60/93), 92.6% (176/190), 81.1% (60/74), 84.2% (176/209), and 0.603, respectively; the sensitivity, specificity, PPV, NPV, and kappa value of blood culture were 81.7% (76/93), 100.0% (190/190), 100.0% (76/76), 91.8% (190/207), and 0.857, respectively (Table 2). These results suggest that the Mp1p assay showed a trend advantage over the GM assay. The combined approach “Mp1p+GM” assay showed a trend advantage in terms of the sensitivity and NPV for the diagnosis of talaromycosis over the Mp1p assay (sensitivity: 82.8% [77/93] vs 72.0% [67/93]; NPV: 91.4% [170/186] vs 87.6% [184/210]) but had slightly decreased specificity and PPV (specificity: 89.5% [170/190] vs 96.8% [184/190]; PPV: 79.4% [77/97] vs 91.8% [67/73]) (Table 2). The best agreement was observed in the blood culture (kappa: 0.857), followed by the Mp1p assay (kappa: 0.729) and “Mp1p+GM” assay (kappa: 0.715), and the worst agreement in the GM assay (kappa: 0.603) (Fig. 4).
In the total population, the diagnostic accuracy of the Mp1p assay, GM assay, and “Mp1p+GM” assay in those with CD4+ counts of < 50 cells/µL was superior to that in those with higher CD4+ counts (Fig. 5). In the subgroup with CD4+ counts of < 50 cells/µL, the Mp1p assay showed a trend advantage over the GM assay for the diagnosis of talaromycosis, with a sensitivity of 74.1%, a specificity of 97.2%, a PPV of 95.5%, and an NPV of 82.8% (Table 3); The best agreement was observed in the “Mp1p+GM” assay (kappa: 0.748), followed by the Mp1p assay (kappa: 0.732) and GM assay (kappa: 0.602). In the subgroup with a CD4+ count of 50–100 cells/µL, the sensitivity and kappa value of the Mp1p assay, GM assay, and “Mp1p+GM” assay were all quite low (Table 3).
Discussion
In this study, we found that Mp1p antigen detection possesses a superior advantage in assisting in talaromycosis diagnosis in patients with AIDS within 3 days of admission, especially those with low CD4+ counts (< 50 cells/µL).
Culture and histopathology are recognised as the gold standard methods for talaromycosis diagnosis but are time-consuming and have insufficient sensitivity. The median time for identifying T. marneffei from blood cultures was 7 (5–9) days in our study, which is similar to the study finding by Le et al. [4]. The time delay of culture and the difficulty of pathological detection make its rapid clinical diagnosis particularly difficult. PCR testing can help in the early diagnosis of talaromycosis, with a high specificity of 100%; however, it is expensive, with a low sensitivity of 70.4% before treatment [13]. T. marneffei specific antibody detection showed a sensitivity of 25%–95% and was strongly cross-reactive to other pathogens, which limited its clinical application [14]. In recent years, an increasing number of studies have focused on the detection of T. marneffei specific antigens, including CYA, GM, and Mp1p. The sensitivity of these methods was 75%–95%, and the specificity was 90%–100%, indicating their potential for clinical application [11, 15,16,17,18]. Mp1p has been shown to be highly immunogenic in previous study [21, 22].
As shown in our study, the incidence of talaromycosis was higher in the young adult patients with AIDS (65.6% vs 45.8%, P = 0.002), and the incidence of symptoms, such as fever, cough, sputum, and rash, and abnormal laboratory test results was higher in the patients with talaromycosis than in those without. However, these markers do not have sufficient specificity for identifying talaromycosis in clinical practice. In our study, the positivity rate for rash, a specific indicator of talaromycosis, was < 40% in the patients with talaromycosis, which was insufficient to be used as a diagnostic indicator.
The positivity rate in the Mp1p assay in the patients with talaromycosis was similar to that in the blood culture (72% vs 81.7%, P = 0.122) in our study. It had a substantial agreement with the gold standard (kappa: 0.729), and the sensitivity, specificity, PPV, and NPV of Mp1p antigen detection were 72.0%, 96.8%, 91.8%, and 87.6%, respectively, which were generally superior to those of the GM assay. Several studies have been conducted to validate the efficiency of different serum diagnostic methods [2, 11, 13, 15,16,17, 19]. Wang et al. detected the Mp1p antigen and antibody in 20 serum specimens of patients with talaromycosis and 525 negative control specimens [15]. They found that the sensitivity of Mp1p antigen ELISA was 75%, which was superior to that of the Mp1p antibody test (30%). Another similar study conducted in Vietnam reported that the Mp1p antigen test had an excellent sensitivity of 86.3% and a specificity of 98.1% for talaromycosis diagnosis in patients with HIV infection [16]. These previous study findings, together with our findings, indicate that Mp1p antigen detection is a good tool for the early diagnosis of talaromycosis. Moreover, this technique is simple to perform and is commercially available; therefore, it is potentially generalizable to routine clinical practice. The sensitivity of the Mp1p assay in our study was lower than that in the study conducted in Vietnam (72.0% vs 86.3%), possibly because of the difference in the control group. Our control group was limited to patients with AIDS without talaromycosis, while the control group in the study conducted in Vietnam included healthy volunteers and patients with non-HIV-related infections. In addition, some of our patients had received antifungal treatment before admission, which could also affect the results. The GM assay is also an available diagnostic tool in talaromycosis diagnosis but was found to be inferior to Mp1p antigen detection. It had a substantial agreement with the gold standard (kappa: 0.603) in our study; however, the sensitivity was only 64.5%, indicating a greater risk of misdiagnosis. A study conducted in Wuhan found that the GM assay had a sensitivity of 95.8% (23/24) and a specificity of 90.9% (30/33) in talaromycosis diagnosis [11]. The sensitivity of the GM assay in that study seemed to be much higher than that in our study; however, their sample size was small, which may increase the risk of sampling errors. In addition, the selection of the cut-off values and the different inclusion criteria could have affected the results.
There have been no reports related to combined approaches for talaromycosis diagnosis. Combined approaches seemed to have a diagnostic advantage over Mp1p antigen detection alone in our study. In addition, the sensitivity of combined approaches was superior to that of blood culture, although the PPV was not high enough. This suggests that combined approaches have the potential for application and are worth further in-depth studies to establish a better diagnostic model.
In our study, more than 90% of the patients with AIDS with talaromycosis had a CD4+ count of < 50 cells/μL. We found that the number of patients with talaromycosis and the positivity rates in the Mp1p assay increased with decreases in the CD4+ counts. In addition, the Mp1p assay showed a superior diagnostic accuracy in the patients with CD4+ counts of < 50 cells/µL. It is known that lower CD4+ counts are associated with more severe OIs and generally indicate more severe disseminated infections in patients with AIDS. We speculated that in patients with lower CD4+ counts, the increased growth of T. marneffei strains may cause them to secrete more Mp1p antigens into the blood, which makes them easier to detect.
This study identified the clinical value of Mp1p antigen detection, which could assist in the early diagnosis of talaromycosis. Although a small number of studies have explored the diagnostic value of Mp1p antigen detection, these were only preliminary explorations [2, 15, 16]. The relatively large sample size is a strength of our study. Furthermore, in contrast to the study conducted in Vietnam [16], we selected hospitalised patients with AIDS as the control group, which more closely matched the clinical needs. We also compared between the different assays simultaneously, especially the Mp1p and GM assays. Few studies have compared the diagnostic accuracy of Mp1p and GM antigen detections simultaneously. Only Wang et al. [2] used both approaches to investigate Mp1p antigenaemia in patients with HIV infection. However, in their study, the GM assay was used only as a gold standard method for talaromycosis diagnosis.
This study had some limitations. First, our study population included hospitalised patients with AIDS, and the PPV and NPV were not based on the general population. Therefore, our results are only applicable to the identification of talaromycosis in patients with AIDS but not in the general population. Second, our patients lacked records of antifungal treatment before admission; thus, we cannot exclude such confounding factors. Third, there was a limited number of participants with a CD4+ count of 51–100 cells/µL, so this subgroup analysis was only intended as an initial exploration. Nevertheless, our study offers application value. We believe that Mp1p antigen detection can be used for the diagnosis of talaromycosis in clinical settings to promote its early diagnosis and treatment and reduce mortality. To further optimise the clinical application of Mp1p antigen detection, we will further detect and quantify Mp1p levels, determine the best cut-off value, and build a diagnostic model for early diagnosis in a larger prospective group.
In summary, it is difficult to achieve an early diagnosis of talaromycosis relying on the diagnostic gold standard of culture or histopathology. Mp1p antigen detection has a superior advantage in assisting in the early diagnosis of talaromycosis in patients with AIDS, especially those with low CD4+ counts of < 50 cells/µL.
Data Availability
The data used to support the findings of this study have not been made available because no patient approval was obtained.
Code Availability
Not applicable.
Materials Availability
All the materials of the current study are described in the text.
References
Kaplan JE, Benson C, Holmes KK, et al. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Recomm Rep. 2009;58(RR-4):1.
Wang YF, Xu HF, Han ZG, et al. Serological surveillance for Penicillium marneffei infection in HIV-infected patients during 2004–2011 in Guangzhou. China Clin Microbiol Infect. 2015;21(5):484–9. https://doi.org/10.1016/j.cmi.2014.12.014.
Supparatpinyo K, Chiewchanvit S, Hirunsri P, et al. Penicillium marneffei infection in patients infected with human immunodeficiency virus. Clin Infect Dis. 1992;14(4):871–4. https://doi.org/10.1093/clinids/14.4.871.
Le T, Wolbers M, Chi NH, et al. Epidemiology, seasonality, and predictors of outcome of AIDS-associated Penicillium marneffei infection in Ho Chi Minh City. Viet Nam Clin Infect Dis. 2011;52(7):945–52. https://doi.org/10.1093/cid/cir028.
Larsson M, Nguyen LHT, Wertheim HF, et al. Clinical characteristics and outcome of Penicillium marneffei infection among HIV-infected patients in northern Vietnam. AIDS Res Ther. 2012;9(1):24. https://doi.org/10.1186/1742-6405-9-24.
Hu Y, Zhang J, Li X, et al. Penicillium marneffei infection: an emerging disease in mainland China. Mycopathologia. 2013;175(1–2):57–67. https://doi.org/10.1007/s11046-012-9577-0.
Qin Y, Huang X, Chen H, et al. Burden of Talaromyces marneffei infection in people living with HIV/AIDS in Asia during ART era: a systematic review and meta-analysis. BMC Infect Dis. 2020;20(1):551. https://doi.org/10.1186/s12879-020-05260-8.
Ying RS, Le T, Cai WP, et al. Clinical epidemiology and outcome of HIV-associated talaromycosis in Guangdong, China, during 2011–2017. HIV Med. 2020;21(11):729–38. https://doi.org/10.1111/hiv.13024.
Son VT, Khue PM, Strobel M. Penicilliosis and AIDS in Haiphong, Vietnam: evolution and predictive factors of death. Med Mal Infect. 2014;44(11–12):495–501. https://doi.org/10.1016/j.medmal.2014.09.008.
Chastain DB, Henao-Martinez AF, Franco-Paredes C. Opportunistic invasive mycoses in AIDS: cryptococcosis, histoplasmosis, coccidiodomycosis, and talaromycosis. Curr Infect Dis Rep. 2017;19(10):36. https://doi.org/10.1007/s11908-017-0592-7.
Zheng J, Gui X, Cao Q, et al. A clinical study of acquired immunodeficiency syndrome associated Penicillium marneffei infection from a non-endemic area in China. PLoS ONE. 2015;10(6): e0130376. https://doi.org/10.1371/journal.pone.0130376.
Vanittanakom N, Cooper CR Jr, Fisher MC, et al. Penicillium marneffei infection and recent advances in the epidemiology and molecular biology aspects. Clin Microbiol Rev. 2006;19(1):95–110. https://doi.org/10.1128/CMR.19.1.95-110.2006.
Hien HTA, Thanh TT, Thu NTM, et al. Development and evaluation of a real-time polymerase chain reaction assay for the rapid detection of Talaromyces marneffei MP1 gene in human plasma. Mycoses. 2016;59(12):773–80. https://doi.org/10.1111/myc.12530.
Pruksaphon K, Intaramat A, Ratanabanangkoon K, et al. Diagnostic laboratory immunology for talaromycosis (penicilliosis): review from the bench-top techniques to the point-of-care testing. Diagn Microbiol Infect Dis. 2020;96(3):114959. https://doi.org/10.1016/j.diagmicrobio.2019.114959.
Wang YF, Cai JP, Wang YD, et al. Immunoassays based on Penicillium marneffei Mp1p derived from Pichia pastoris expression system for diagnosis of penicilliosis. PLoS ONE. 2011;6(12):e28796. https://doi.org/10.1371/journal.pone.0028796.
Thu NTM, Chan JFW, Ly VT, et al. Superiority of a novel Mp1p antigen detection enzyme immunoassay compared to standard BACTEC blood culture in the diagnosis of talaromycosis. Clin Infect Dis. 2021;73(2):e330–6. https://doi.org/10.1093/cid/ciaa826.
Prakit K, Nosanchuk JD, Pruksaphon K, et al. A novel inhibition ELISA for the detection and monitoring of Penicillium marneffei antigen in human serum. Eur J Clin Microbiol Infect Dis. 2016;35(4):647–56. https://doi.org/10.1007/s10096-016-2583-2.
Pruksaphon K, Intaramat A, Ratanabanangkoon K, et al. Development and characterization of an immunochromatographic test for the early diagnosis of Talaromyces (Penicillium) marneffei. PLoS ONE. 2018;13(4):e0195596. https://doi.org/10.1371/journal.pone.0195596.
Ning C, Lai J, Wei W, et al. Accuracy of rapid diagnosis of Talaromyces marneffei: a systematic review and meta-analysis. PLoS ONE. 2018;13(4):e0195569. https://doi.org/10.1371/journal.pone.0195569.
Huang Y-T, Hung C-C, Liao C-H, et al. Detection of circulating galactomannan in serum samples for diagnosis of Penicillium marneffei infection and cryptococcosis among patients infected with human immunodeficiency virus. J Clin Microbiol. 2007;45(9):2858–62. https://doi.org/10.1128/JCM.00050-07.
Cao L, Chan CM, Lee C, et al. MP1 encodes an abundant and highly antigenic cell wall mannoprotein in the pathogenic fungus Penicillium marneffei. Infect Immun. 1998;66(3):966–73. https://doi.org/10.1128/IAI.66.3.966-973.1998.
Woo PC, Lau SK, Lau CC, et al. Mp1p is a virulence factor in Talaromyces (Penicillium) marneffei. PLoS Negl Trop Dis. 2016;10(8):e0004907. https://doi.org/10.1371/journal.pntd.0004907.
Cao L, Chan KM, Chen D, et al. Detection of cell wall mannoprotein Mp1p in culture supernatants of Penicillium marneffei and in sera of penicilliosis patients. J Clin Microbiol. 1999;37(4):981–6. https://doi.org/10.1128/JCM.37.4.981-986.1999.
Ly VT, Thanh NT, Thu NTM, et al. Occult Talaromyces marneffei infection unveiled by the novel Mp1p antigen detection assay. Open Forum Infect Dis. 2020;7(11):ofaa502. https://doi.org/10.1093/ofid/ofaa502.
Wang Y, Zeng L, Chen X, et al. A double-antigen sandwich ELISA for detecting Penicillium marneffei Mp1p-specific antibody. Nan Fang Yi Ke Da Xue Xue Bao. 2013;33(3):439–43.
He K, Feng L, Liang Z, et al. Value of serum galactomannan test in diagnosis of AIDS complicated with Penicilliosis marneffei. Acad J Guangzhou Med Univ. 2016;44(03):21–4.
Acknowledgements
We gratefully acknowledge our study group members for their work. We would like to thank Editage for English language editing.
Funding
This work was supported by grants from the Guangzhou Basic Research Program on People’s Livelihood Science and Technology (Grant Number: 202002020005) and the National Natural Science Foundation of China (Grant Number: 82072265).
Author information
Authors and Affiliations
Contributions
WC, XT, and LL designed and supervised the study. Material preparation, experimental operation, and data collection were carried out by XO, HW, LL, PG, and XC. Data collation and result analysis were performed by XC and XO. The first draft of the manuscript was written by XC and XO. LL reviewed and revised the draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No potential conflict of interest is declared by the authors.
Ethical Approval
Ethical approval was provided by the Medical Ethics Committee of the Guangzhou Eighth People’s Hospital (Approval No. 202034167).
Informed Consent
All patients signed an informed consent form.
Consent for Publication
Not applicable.
Additional information
Handling Editor: Patrick C. Y. Woo.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chen, X., Ou, X., Wang, H. et al. Talaromyces marneffei Mp1p Antigen Detection may Play an Important Role in the Early Diagnosis of Talaromycosis in Patients with Acquired Immunodeficiency Syndrome. Mycopathologia 187, 205–215 (2022). https://doi.org/10.1007/s11046-022-00618-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-022-00618-9