Abstract
Background
TP53 gene plays a pivotal role in maintaining genetic stability and prevention of malignancies. Alterations of this gene are implicated in more than half of human cancers. To the best of our knowledge, this study is the first to explore TP53 polymorphisms in Moroccan childhood acute lymphoblastic leukemia (ALL).
Methods and results
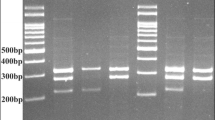
DNA samples of 45 ALL children were obtained from peripheral blood. A total of 333 healthy Moroccans were used as controls. Polymerase chain reaction and Sanger sequencing were performed to analyze TP53 hotspot exons in cases. We identified a significant protective effect of the TP53-Arg variant at rs1042522 [OR 0.4593 (0.249–0.8472), p = 0.0127] and the Pro/Arg genotype [OR 0.0350 (0.0047–0.2583), p = 0.0010]. Additionally, we found a novel association between the C-allele of Arg213Arg 1800372 [OR 2.7736 (1.3821–5.5664), p = 0.0041] and the risk of childhood ALL. Importantly, TC/CC genotypes of this polymorphism were revealed to enhance the risk of ALL among females [OR 9.0 (3.1555–25.6693), p < 0.0001]. Arg213Arg was also noticed to be associated with the hemoglobin count of patients at diagnosis by linear regression (p = 0.0318). The analysis of penetrance showed a significant association of the CG/GG genotypes at rs1042522 and TC/CC genotypes at rs1800372 to childhood ALL via dominant model [OR 0.2090 (0.09074–0.4814), p = 0.0002 and OR 3.4205 (1.6084–7.2742), p = 0.0014 for rs1042522 and rs1800372 respectively]. No association was found between TP53 polymorphisms and patients survival.
Conclusion
Altogether, our findings indicated that TP53 polymorphisms are significantly involved in the genetic susceptibility to childhood ALL in Morocco.

Similar content being viewed by others
References
Bhojwani D, Yang JJ, Pui CH (2015) Biology of childhood acute lymphoblastic leukemia. Pediatr Clin North Am 62(1):47–60. https://doi.org/10.1016/j.pcl.2014.09.004
Inaba H, Greaves M, Mullighan CG (2013) Acute lymphoblastic leukaemia. Lancet 381(9881):1943–1955. https://doi.org/10.1016/s0140-6736(12)62187-4
Chebihi ZT, Belkhayat A, Chadli E, Hilal L, Skhoun H, Hessissen L, El Khorassani M, El Kababri M, Kili A, Khattab M et al (2018) Cytogenetic profile of moroccan pediatric acute lymphoblastic leukemia: analysis of 155 cases with a review of the literature. Clin Lymph Myeloma Leuk 18(6):e241–e248. https://doi.org/10.1016/j.clml.2018.04.004
Iacobucci I, Mullighan CG (2017) Genetic basis of acute lymphoblastic leukemia. J Clin Oncol 35(9):975–983. https://doi.org/10.1200/jco.2016.70.7836
Roberts KG, Mullighan CG (2015) Genomics in acute lymphoblastic leukaemia: insights and treatment implications. Nat Rev Clin Oncol 12(6):344–357. https://doi.org/10.1038/nrclinonc.2015.38
McGraw KL, Zhang LM, Rollison DE, Basiorka AA, Fulp W, Rawal B, Jerez A, Billingsley DL, Lin HY, Kurtin SE et al (2015) The relationship of TP53 R72P polymorphism to disease outcome and TP53 mutation in myelodysplastic syndromes. Blood Cancer J 5(3):e291. https://doi.org/10.1038/bcj.2015.11
Sullivan KD, Galbraith MD, Andrysik Z, Espinosa JM (2018) Mechanisms of transcriptional regulation by p53. Cell Death Differ 25(1):133–143. https://doi.org/10.1038/cdd.2017.174
Hainaut P, Wiman KG (2009) 30 years and a long way into p53 research. Lancet Oncol 10(9):913–919. https://doi.org/10.1016/s1470-2045(09)70198-6
Efeyan A, Serrano M (2007) p53: guardian of the genome and policeman of the oncogenes. Cell Cycle 6(9):1006–1010. https://doi.org/10.4161/cc.6.9.4211
Song H, Xu Y (2007) Gain of function of p53 cancer mutants in disrupting critical DNA damage response pathways. Cell Cycle 6(13):1570–1573. https://doi.org/10.4161/cc.6.13.4456
Comeaux EQ, Mullighan CG (2017) TP53 mutations in hypodiploid acute lymphoblastic leukemia. Cold Spring Harb Perspect Med. https://doi.org/10.1101/cshperspect.a026286
Wada M, Bartram CR, Nakamura H, Hachiya M, Chen DL, Borenstein J, Miller CW, Ludwig L, Hansen-Hagge TE, Ludwig WD et al (1993) Analysis of p53 mutations in a large series of lymphoid hematologic malignancies of childhood. Blood 82(10):3163–3169. https://doi.org/10.1182/blood.V82.10.3163.3163
Hof J, Krentz S, van Schewick C, Körner G, Shalapour S, Rhein P, Karawajew L, Ludwig WD, Seeger K, Henze G et al (2011) Mutations and deletions of the TP53 gene predict nonresponse to treatment and poor outcome in first relapse of childhood acute lymphoblastic leukemia. J Clin Oncol 29(23):3185–3193. https://doi.org/10.1200/jco.2011.34.8144
Mühlbacher V, Zenger M, Schnittger S, Weissmann S, Kunze F, Kohlmann A, Bellos F, Kern W, Haferlach T, Haferlach C (2014) Acute lymphoblastic leukemia with low hypodiploid/near triploid karyotype is a specific clinical entity and exhibits a very high TP53 mutation frequency of 93%. Genes Chromosom Cancer 53(6):524–536. https://doi.org/10.1002/gcc.22163
Stengel A, Schnittger S, Weissmann S, Kuznia S, Kern W, Kohlmann A, Haferlach T, Haferlach C (2014) TP53 mutations occur in 15.7% of ALL and are associated with MYC-rearrangement, low hypodiploidy, and a poor prognosis. Blood 124(2):251–258. https://doi.org/10.1182/blood-2014-02-558833
Basu S, Murphy ME (2016) Genetic modifiers of the p53 pathway. Cold Spring Harb Perspect Med 6(4):a026302. https://doi.org/10.1101/cshperspect.a026302
Dunna NR, Vure S, Sailaja K, Surekha D, Raghunadharao D, Rajappa S, Vishnupriya S (2012) TP53 codon 72 polymorphism and risk of acute leukemia. Asian Pac J Cancer Prev 13(1):347–350. https://doi.org/10.7314/apjcp.2012.13.1.349
Barnoud T, Parris JLD, Murphy ME (2019) Common genetic variants in the TP53 pathway and their impact on cancer. J Mol Cell Biol 11(7):578–585. https://doi.org/10.1093/jmcb/mjz052
Beckman G, Birgander R, Själander A, Saha N, Holmberg PA, Kivelä A, Beckman L (1994) Is p53 polymorphism maintained by natural selection? Hum Hered 44(5):266–270. https://doi.org/10.1159/000154228
Ricks-Santi L, Mason T, Apprey V, Ahaghotu C, McLauchlin A, Josey D, Bonney G, Dunston GM (2010) p53 Pro72Arg polymorphism and prostate cancer in men of African descent. Prostate 70(16):1739–1745. https://doi.org/10.1002/pros.21209
de Lourdes PA, Guembarovski RL, Oda JM, Lopes LF, Ariza CB, Amarante MK, Fungaro MH, de Oliveira KB, Watanabe MA (2013) CXCL12 and TP53 genetic polymorphisms as markers of susceptibility in a Brazilian children population with acute lymphoblastic leukemia (ALL). Mol Biol Rep 40(7):4591–4596. https://doi.org/10.1007/s11033-013-2551-1
Do TN, Ucisik-Akkaya E, Davis CF, Morrison BA, Dorak MT (2009) TP53 R72P and MDM2 SNP309 polymorphisms in modification of childhood acute lymphoblastic leukemia susceptibility. Cancer Genet Cytogenet 195(1):31–36. https://doi.org/10.1016/j.cancergencyto.2009.05.009
Weich N, Ferri C, Moiraghi B, Bengió R, Giere I, Pavlovsky C, Larripa I, Fundia A (2016) TP53 codon 72 polymorphism predicts chronic myeloid leukemia susceptibility and treatment outcome. Blood Cells Mol Dis 59:129–133. https://doi.org/10.1016/j.bcmd.2016.05.007
Bilous N, Abramenko I, Saenko V, Chumak A, Dyagil I, Martina Z, Kryachok I (2017) Clinical relevance of TP53 polymorphic genetic variations in chronic lymphocytic leukemia. Leuk Res 58:1–8. https://doi.org/10.1016/j.leukres.2017.03.009
Weng Y, Lu L, Yuan G, Guo J, Zhang Z, Xie X, Chen G, Zhang J (2012) p53 codon 72 polymorphism and hematological cancer risk: an update meta-analysis. PLoS ONE 7(9):e45820. https://doi.org/10.1371/journal.pone.0045820
Tian X, Dai S, Sun J, Jiang S, Jiang Y (2016) Association between TP53 Arg72Pro polymorphism and leukemia risk: a meta-analysis of 14 case–control studies. Sci Rep 6:24097. https://doi.org/10.1038/srep24097
Drokow EK, Chen Y, Waqas Ahmed HA, Oppong TB, Akpabla GS, Pei Y, Kumah MA, Neku EA, Sun K (2020) The relationship between leukemia and TP53 gene codon Arg72Pro polymorphism: analysis in a multi-ethnic population. Future Oncol 16(14):923–937. https://doi.org/10.2217/fon-2019-0792
Ezzikouri S, Essaid El Feydi A, Afifi R, Benazzouz M, Hassar M, Pineau P, Benjelloun S (2011) Impact of TP53 codon 72 and MDM2 promoter 309 allelic dosage in a Moroccan population with hepatocellular carcinoma. Int J Biol Markers 26(4):229–233. https://doi.org/10.5301/jbm.2011.8881
Rebbani K, Marchio A, Ezzikouri S, Afifi R, Kandil M, Bahri O, Triki H, El Feydi AE, Dejean A, Benjelloun S et al (2015) TP53 R72P polymorphism modulates DNA methylation in hepatocellular carcinoma. Mol Cancer 14:74. https://doi.org/10.1186/s12943-015-0340-2
El Khair MM, Ennaji MM, El Kebbaj R, Mhand RA, Attaleb M, El Mzibri M (2010) p53 codon 72 polymorphism and risk of cervical carcinoma in Moroccan women. Med Oncol 27(3):861–866. https://doi.org/10.1007/s12032-009-9297-6
Ayoubi SE, Elkarroumi M, El Khachibi M, Hassani Idrissi H, Ayoubi H, Ennachit S, Arazzakou M, Nadifi S (2018) The 72Pro variant of the tumor protein 53 is associated with an increased breast cancer risk in the Moroccan population. Pathobiology 85(4):247–253. https://doi.org/10.1159/000489852
Boisson-Dupuis S, Ramirez-Alejo N, Li Z, Patin E, Rao G, Kerner G, Lim CK, Krementsov DN, Hernandez N, Ma CS et al (2018) Tuberculosis and impaired IL-23-dependent IFN-γ immunity in humans homozygous for a common TYK2 missense variant. Sci Immunol. https://doi.org/10.1126/sciimmunol.aau8714
Grant AV, El Baghdadi J, Sabri A, El Azbaoui S, Alaoui-Tahiri K, Abderrahmani Rhorfi I, Gharbaoui Y, Abid A, Benkirane M, Raharimanga V et al (2013) Age-dependent association between pulmonary tuberculosis and common TOX variants in the 8q12-13 linkage region. Am J Hum Genet 92(3):407–414. https://doi.org/10.1016/j.ajhg.2013.01.013
Dumont P, Leu JI, Della Pietra AC 3rd, George DL, Murphy M (2003) The codon 72 polymorphic variants of p53 have markedly different apoptotic potential. Nat Genet 33(3):357–365. https://doi.org/10.1038/ng1093
Bonafé M, Salvioli S, Barbi C, Trapassi C, Tocco F, Storci G, Invidia L, Vannini I, Rossi M, Marzi E et al (2004) The different apoptotic potential of the p53 codon 72 alleles increases with age and modulates in vivo ischaemia-induced cell death. Cell Death Differ 11(9):962–973. https://doi.org/10.1038/sj.cdd.4401415
Pim D, Banks L (2004) p53 polymorphic variants at codon 72 exert different effects on cell cycle progression. Int J Cancer 108(2):196–199. https://doi.org/10.1002/ijc.11548
Frank AK, Leu JI, Zhou Y, Devarajan K, Nedelko T, Klein-Szanto A, Hollstein M, Murphy ME (2011) The codon 72 polymorphism of p53 regulates interaction with NF-{kappa}B and transactivation of genes involved in immunity and inflammation. Mol Cell Biol 31(6):1201–1213. https://doi.org/10.1128/mcb.01136-10
Kung CP, Khaku S, Jennis M, Zhou Y, Murphy ME (2015) Identification of TRIML2, a novel p53 target, that enhances p53 SUMOylation and regulates the transactivation of proapoptotic genes. Mol Cancer Res 13(2):250–262. https://doi.org/10.1158/1541-7786.Mcr-14-0385
Bonafè M, Salvioli S, Barbi C, Mishto M, Trapassi C, Gemelli C, Storci G, Olivieri F, Monti D, Franceschi C (2002) p53 codon 72 genotype affects apoptosis by cytosine arabinoside in blood leukocytes. Biochem Biophys Res Commun 299(4):539–541. https://doi.org/10.1016/s0006-291x(02)02691-8
Dahabreh IJ, Schmid CH, Lau J, Varvarigou V, Murray S, Trikalinos TA (2013) Genotype misclassification in genetic association studies of the rs1042522 TP53 (Arg72Pro) polymorphism: a systematic review of studies of breast, lung, colorectal, ovarian, and endometrial cancer. Am J Epidemiol 177(12):1317–1325. https://doi.org/10.1093/aje/kws394
Shetzer Y, Napchan Y, Kaufman T, Molchadsky A, Tal P, Goldfinger N, Rotter V (2017) Immune deficiency augments the prevalence of p53 loss of heterozygosity in spontaneous tumors but not bi-directional loss of heterozygosity in bone marrow progenitors. Int J Cancer 140(6):1364–1369. https://doi.org/10.1002/ijc.30554
Deben C, Van den Bossche J, Van Der Steen N, Lardon F, Wouters A, de Beeck KO, Hermans C, Jacobs J, Peeters M, Van Camp G et al (2017) Deep sequencing of the TP53 gene reveals a potential risk allele for non-small cell lung cancer and supports the negative prognostic value of TP53 variants. Tumour Biol 39(2):1–8. https://doi.org/10.1177/1010428317694327
Mirabello L, Yeager M, Mai PL, Gastier-Foster JM, Gorlick R, Khanna C, Patiño-Garcia A, Sierrasesúmaga L, Lecanda F, Andrulis IL et al (2015) Germline TP53 variants and susceptibility to osteosarcoma. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djv101
Scott EM, Halees A, Itan Y, Spencer EG, He Y, Azab MA, Gabriel SB, Belkadi A, Boisson B, Abel L et al (2016) Characterization of Greater Middle Eastern genetic variation for enhanced disease gene discovery. Nat Genet 48(9):1071–1076. https://doi.org/10.1038/ng.3592
Hamadou WS, Besbes S, Bourdon V, Youssef YB, Laatiri MA, Noguchi T, Khélif A, Sobol H, Soua Z (2017) Mutational analysis of TP53 gene in Tunisian familial hematological malignancies and sporadic acute leukemia cases. Fam Cancer 16(1):153–157. https://doi.org/10.1007/s10689-016-9931-3
Albanese I, Scibetta AG, Migliavacca M, Russo A, Bazan V, Tomasino RM, Colomba P, Tagliavia M, La Farina M (2004) Heterogeneity within and between primary colorectal carcinomas and matched metastases as revealed by analysis of Ki-ras and p53 mutations. Biochem Biophys Res Commun 325(3):784–791. https://doi.org/10.1016/j.bbrc.2004.10.111
Kucera E, Speiser P, Gnant M, Szabo L, Samonigg H, Hausmaninger H, Mittlböck M, Fridrik M, Seifert M, Kubista E et al (1999) Prognostic significance of mutations in the p53 gene, particularly in the zinc-binding domains, in lymph node- and steroid receptor positive breast cancer patients. Austrian Breast Cancer Study Group. Eur J Cancer 35(3):398–405. https://doi.org/10.1016/s0959-8049(98)00400-6
Dang RK, Anthony RS, Craig JI, Leonard RC, Parker AC (2002) Limitations of the use of single base changes in the p53 gene to detect minimal residual disease of breast cancer. Mol Pathol 55(3):177–181. https://doi.org/10.1136/mp.55.3.177
Aceto GM, Awadelkarim KD, Di Nicola M, Moscatello C, Pantalone MR, Verginelli F, Elwali NE, Mariani-Costantini R (2019) Germline TP53 mutation spectrum in Sudanese premenopausal breast cancer patients: correlations with reproductive factors. Breast Cancer Res Treat 175(2):479–485. https://doi.org/10.1007/s10549-019-05168-1
Krasteva ME, Georgieva EI (2006) Germline p53 single-base changes associated with Balkan endemic nephropathy. Biochem Biophys Res Commun 342(2):562–567. https://doi.org/10.1016/j.bbrc.2006.02.004
Acknowledgements
The authors would like to thank children and their parents or guardians who made this study possible. Warmest thanks to the staff of the Pediatric Hematology and Oncology Center in the Children’s Hospital of Rabat for their collaboration and helpful assistance. Sincere gratitude to Dr. Laurent Abel, Dr. Stéphanie Boisson-Dupuis and Dr. Jocelyn Quisterbert from Imagine Institute, Paris, France for their valuable revisions. Many thanks to Mohammed Lamssiyeh from the Genetics Unit of Military Hospital Mohammed V for the laboratory assistance. The first author was an Excellence Scholarship holder from the National Center for Scientific and Technical Research (CNRST) of Rabat, Morocco.
Funding
This study was supported by the Genetics Unit of Military Hospital Mohammed V in Rabat, Morocco.
Author information
Authors and Affiliations
Contributions
HS: patients enrollement, genetic study performance, statistical analysis, data collecting and interpretation, involvement in the literature search and writing of the paper. MK: diagnosis and examination of patients. AB: cytogenetic analysis. ZTC: cytogenetic analysis. YB: study investigation. ND: study investigation. JEB: conceptualization, methodology, study investigation, supervision, statistical analysis, revision and editing of the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
This research work was approved by the Ethics Committee for Biomedical research in Faculty of Medicine and Pharmacy of Rabat.
Informed consent
Informed consent for participation and publication has been obtained from the parents or legal guardians of children.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Skhoun, H., Khattab, M., Belkhayat, A. et al. Association of TP53 gene polymorphisms with the risk of acute lymphoblastic leukemia in Moroccan children. Mol Biol Rep 49, 8291–8300 (2022). https://doi.org/10.1007/s11033-022-07643-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-022-07643-3