Abstract
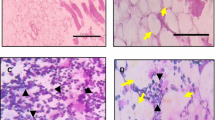
Myelodysplastic syndrome is a heterogenous group of disorder with clonal dysregulated hematopoiesis characterized by bone marrow failure, cytogenetic and molecular abnormalities and variable risk of progression to acute myeloid leukemia (AML). The bone marrow niche plays a major role in maintaining the homeostasis and is often injured by the chemotherapeutic drugs leading to catastrophic consequences like myelodysplastic syndrome. In the present study, we made an attempt to find out the osteoblastic niche related alterations in the myelodysplastic bone marrow through mainly flowcytometric and fluorescent microscopic studies. We have also checked the condition of the myelodysplastic bone through micro computed tomography. The results revealed that the affected osteoblasts of the myelodysplastic bone marrow compelled the hematopoietic stem cell to come out of quiescence and become actively proliferating, and in this scenario the decline in expression of cell adhesion molecules like N-Cadherin, Intercellular adhesion molecule 1 (ICAM) and upregulated focal adhesion kinase (FAK) played a major role. The hike in number of osteoclasts in myelodysplastic cases than control also shattered the balance between bone formation and resorption ratio. We have recorded a dysregulated expression of transcription factors GATA2 and CEBPα (CCAAT-enhancer-binding-protein) in the hematopoietic stem progenitor compartment of the myelodysplastic bone marrow, the main reason behind the presence of abnormal myeloblasts in myelodysplastic cases. Collectively, we can say the coordinated perturbations in the osteoblastic niche, cell adhesion molecules together with the transcription factors has resulted in the uncontrolled proliferation of hematopoietic stem cell, dysregulated myelopoiesis, early trafficking of hematopoietic progenitors to blood compartment and at the same time pancytopenic peripheral blood conditions during the progression of N-Ethyl N Nitroso Urea (ENU) induced myelodysplasia.







Similar content being viewed by others
Abbreviations
- AML:
-
Acute myeloid leukemia
- ASXL1:
-
Additional sex combs like-1
- CAM:
-
Cell adhesion molecule
- CEBPα:
-
CCAAT-enhancer-binding-protein α
- E-Cadherin:
-
Epithelial cadherin
- ENU:
-
N-Ethyl N nitroso urea
- FAK:
-
Focal adhesion kinase
- HSC:
-
Hematopoietic stem cell
- HPC:
-
Hematopoietic progenitor cell
- HSPC:
-
Hematopoietic stem progenitor compartment
- ICAM:
-
Intercellular adhesion molecule 1
- N-Cadherin:
-
Neural cadherin
- PU1:
-
Purine rich
- RANK:
-
Receptor activator of nuclear factor kappa-B ligand
- RUNX:
-
Runt-related transcription factor
- TET2:
-
Tet methylcytosine dioxygenase 2
- TP53:
-
Tumor protein p53
- TPO:
-
Thrombopoietin
References
Dussiau C, Fontenay M (2018) Mechanisms underlying the heterogeneity of myelodysplastic syndromes. Exp Hematol 58:17–26
Bulycheva E, Rauner M, Medyouf H, Theurl I, Bornhäuser M, Hofbauer LC, Platzbecker U (2015) Myelodysplasia is in the niche: novel concepts and emerging therapies. Leukemia 29(2):259–268
Ebina W, Rossi DJ (2015) Transcription factor-mediated reprogramming toward hematopoietic stem cells. EMBO J 34(6):694–709
Zhu J, Emerson S (2002) Hematopoietic cytokines, transcription factors and lineage commitment. Oncogene 21:3295–3313
Klamer S, Voermans C (2014) The role of novel and known extracellular matrix and adhesion molecules in the homeostatic and regenerative bone marrow microenvironment. Cell Adhes Migr 8(6):563–577
Bodine DM (2017) Introduction to the review series on transcription factors in hematopoiesis and hematologic disease. Blood 129(15):2039
Churpek JE, Bresnick EH (2019) Transcription factor mutations as a cause of familial myeloid neoplasms. J Clin Invest 129(2):476–488
de Bruijn M, Dzierzak E (2017) Runx transcription factors in the development and function of the definitive hematopoietic system. Blood 129(15):2061–2069
Wang CQ, Krishnan V, Tay LS et al (2014) Disruption of Runx1 and Runx3 leads to bone marrow failure and leukemia predisposition due to transcriptional and DNA repair defects. Cell Rep 8(3):767–782
Li X, Huang M, Zheng H, Wang Y, Ren F, Shang Y, Zhai Y, Irwin DM, Shi Y, Chen D, Chang Z (2008) CHIP promotes Runx2 degradation and negatively regulates osteoblast differentiation. J Cell Biol 181(6):959–972
Rodrigues NP, Tipping AJ, Wang Z, Enver T (2012) GATA-2 mediated regulation of normal hematopoietic stem/progenitor cell function, myelodysplasia and myeloid leukemia. Int J Biochem Cell Biol 44(3):457–460
Rodrigues NP, Boyd AS, Fugazza C, May GE, Guo Y, Tipping AJ, Scadden DT, Vyas P, Enver T (2008) GATA-2 regulates granulocyte-macrophage progenitor cell function. Blood 112:4862–4873
Rodrigues NP, Janzen V, Forkert R, Dombkowski DM, Boyd AS, Orkin SH, Enver T, Vyas P, Scadden DT (2005) Haploinsufficiency of GATA-2 perturbs adult hematopoietic stem-cell homeostasis. Blood 106:477–484
Tipping AJ, Pina C, Castor A, Hong D, Rodrigues NP, Lazzari L, May GE, Jacobsen SE, Enver T (2009) High GATA-2 expression inhibits human hematopoietic stem and progenitor cell function by effects on cell cycle. Blood 113:2661–2672
de Pater E, Kaimakis P, Vink CS, Yokomizo T, Yamada-Inagawa T, van der Linden R, Kartalaei PS, Camper SA, Speck N, Dzierzak E (2013) Gata2 is required for HSC generation and survival. J Exp Med 210(13):2843–2850
Hirai H, Yokota A, Tamura A, Sato A, Maekawa T (2015) Non-steady-state hematopoiesis regulated by the C/EBPβ transcription factor. Cancer Sci 106(7):797–802
Zhang P, Iwasaki-Arai J, Iwasaki H et al (2004) Enhancement of hematopoietic stem cell repopulating capacity and self-renewal in the absence of the transcription factor C ⁄ EBP alpha. Immunity 21:853–863
Zhang DE, Zhang P, Wang ND, Hetherington CJ, Darlington GJ, Tenen DG (1997) Absence of granulocyte colony-stimulating factor signaling and neutrophil development in CCAAT enhancer binding protein alpha-deficient mice. Proc Natl Acad Sci USA 94:569–574
Aggarwal R, Lu J, Pompili VJ, Das H (2012) Hematopoietic stem cells: transcriptional regulation, ex vivo expansion and clinical application. Curr Mol Med 12(1):34–49
Gruszka AM, Valli D, Restelli C, Alcalay M (2019) Adhesion deregulation in acute myeloid leukaemia. Cells 8(1):66
Arai F, Hosokawa K, Toyama H, Matsumoto Y, Suda T (2012) Role of N-cadherin in the regulation of hematopoietic stem cells in the bone marrow niche. Ann N Y Acad Sci 1266:72–77
Chen S, Lewallen M, Xie T (2013) Adhesion in the stem cell niche: biological roles and regulation. Development (Cambridge, England) 140(2):255–265
van de Stolpe A, van der Saag PT (1996) Intercellular adhesion molecule-1. J Mol Med (Berl) 74:13–33
Liu Y, Zhang S, Chen Y, Shi K, Zou B, Liu J, Yang Q, Jiang H, Wei L, Li C, Zhao M, Gabrilovich DI, Zhang H, Zhou J (2018) ICAM-1 Deficiency in the bone marrow niche impairs quiescence and repopulation of hematopoietic stem cells. Stem Cell Rep 11(1):258–273
Genet N, Bhatt N, Bourdieu A, Hirschi KK (2018) Multifaceted roles of connexin 43 in stem cell niches. Curr Stem Cell Rep 4(1):1–12
Wagner W, Wein F, Roderburg C, Saffrich R, Diehlmann A, Eckstein V et al (2008) Adhesion of human hematopoietic progenitor cells to mesenchymal stromal cells involves CD44. Cells Tissues Organs 188(1–2):160–169
Cancelas JA, Koevoet WL, de Koning AE, Mayen AE, Rombouts EJ, Ploemacher RE (2000) Connexin-43 gap junctions are involved in multiconnexin-expressing stromal support of hemopoietic progenitors and stem cells. Blood 96:498–505
Ishikawa ET, Gonzalez-Nieto D, Ghiaur G, Dunn SK, Ficker AM, Murali B, Madhu M, Gutstein DE, Fishman GI, Barrio LC et al (2012) Connexin-43 prevents hematopoietic stem cell senescence through transfer of reactive oxygen species to bone marrow stromal cells. Proc Natl Acad Sci USA 109:9071–9076
Wu Y, Aanei CM, Kesr S, Picot T, Guyotat D, Catafal LC (2017) Impaired expression of focal adhesion kinase in mesenchymal stromal cells from low-risk myelodysplastic syndrome patients. Front Oncol 7:164
Igishi T, Fukuhara S, Patel V, Katz BZ, Yamada KM, Gutkind JS (1999) Divergent signaling pathways link focal adhesion kinase to mitogen-activated protein kinase cascades. Evidence for a role of paxillin in c-Jun NH(2)-terminal kinase activation. J Biol Chem 274(43):30738–30746
Recher C, Ysebaert L, Beyne-Rauzy O, Mansat-De Mas V, Ruidavets JB, Cariven P, Demur C, Payrastre B, Laurent G, Sultan CR (2004) Expression of focal adhesion kinase in acute myeloid leukemia is associated with enhanced blast migration, increased cellularity, and poor prognosis. Cancer Res 9:3191–3197
Borojevic R, Roela RA, Rodarte RS et al (2004) Bone marrow stroma in childhood myelodysplastic syndrome: composition, ability to sustain hematopoiesis in vitro, and altered gene expression. Leuk Res 8:831–844
Li X, Deeg HJ (2014) Murine xenogeneic models of myelodysplastic syndrome: an essential role for stroma cells. Exp Hematol 42(1):4–10
Medyouf H, Mossner M, Jann JC et al (2014) Myelodysplastic cells in patients reprogram mesenchymal stromal cells to establish a transplantable stem cell niche disease unit. Cell Stem Cell 14(6):824–837
Raaijmakers MHGP et al (2010) Bone progenitor dysfunction induces myelodysplasia and secondary leukaemia. Nature 464:852–857
Greenbaum A, Hsu YM, Day RB et al (2013) CXCL12 in early mesenchymal progenitors is required for haematopoietic stem-cell maintenance. Nature 495(7440):227–230
Pang Y, Deng C, Geng S et al (2017) Premature exhaustion of mesenchymal stromal cells from myelodysplastic syndrome patients. Am J Transl Res 9(7):3462–3468
Nakayamada S, Okada Y, Saito K, Tamura M, Tanaka Y (2003) Beta1 integrin/focal adhesion kinase-mediated signaling induces intercellular adhesion molecule 1 and receptor activator of nuclear factor kappaB ligand on osteoblasts and osteoclast maturation. J Biol Chem 278(46):45368–45374
Brown AL, Hahn CN, Scott HS (2020) Secondary leukemia in patients with germline transcription factor mutations (RUNX1, GATA2, CEBPA). Blood 136(1):24–35
Fisher KE, Hsu AP, Williams CL et al (2017) Somatic mutations in children with GATA2-associated myelodysplastic syndrome who lack other features of GATA2 deficiency. Blood Adv 1(7):443–448
Aanei CM, Eloae FZ, Gresta PF, Tavernier E, Carasevici E, Guyotat D, Campos L (2011) Focal adhesion protein abnormalities in myelodysplastic mesenchymal stromal cells. Exp Cell Res 317:2616–2629
Loeffler-Ragg J, Steurer M, Ulmer H et al (2006) Elevated levels of serum CD44 and E-cadherin predict an unfavourable outcome in myelodysplastic syndromes. Leukemia 20:2064–2067
Bhatia S (2013) Therapy-related myelodysplasia and acute myeloid leukemia. Semin Oncol 40(6):666–675
Beurlet S, Omidvar N, Gorombei P, Krief P, Le Pogam C, Setterblad N et al (2013) BCL-2 inhibition with ABT-737 prolongs survival in an NRAS/BCL-2 mouse model of AML by targeting primitive LSK and progenitor cells. Blood 122(16):2864
Watanabe-Okochi N, Kitaura J, Ono R et al (2008) AML1 mutations induced MDS and MDS/AML in a mouse BMT model. Blood 111:4297
Li L, Piloto O, Nguyen HB, Greenberg K, Takamiya K, Racke F et al (2008) Knock in of an internal tandem duplication mutation into murine FLT3 confers myeloproliferative disease in a mouse model. Blood 111(7):3849
Moody JL, Xu L, Helgason CD et al (2004) Anemia, thrombocytopenia, leukocytosis, extramedullary hematopoiesis, and impaired progenitor function in Ptenþ/_SHIP_/_mice: a novel model of myelodysplasia. Blood 103:4503
Pineault N, Buske C, Feuring-Buske M et al (2003) Induction of acute myeloid leukemia in mice by the human leukemia-specific fusion gene NUP98-HOXD13 in concert with Meis1. Blood 101:4529
Daw S, Law A, Law S (2019) Myelodysplastic syndrome related alterations of MAPK signaling in the bone marrow of experimental mice including stem/progenitor compartment. Acta Histochem 121(3):330–343
Chatterjee R, Gupta S, Law S (2017) Hematopathological alterations of major tumor suppressor cascade, vital cell cycle inhibitors and hematopoietic niche components in experimental myelodysplasia. Chem Biol Interact 273:1–10
Daw S, Chatterjee R, Law A, Law S (2016) Analysis of hematopathology and alteration of JAK1/STAT3/STAT5 signaling axis in experimental myelodysplastic syndrome. Chem Biol Interact 260:176–185
Chatterjee R, Chattopadhyay S, Sanyal S, Daw S, Law S (2015) Pathophysiological scenario of hematopoietic disorders: a comparative study of aplastic anemia, myelodysplastic syndrome and leukemia in experimental animals. Proc Zool Soc 69(1):114–124
Das M, Chaudhuri S, Law S (2013) Unveiling the paradoxical nature of myelodysplastic syndromes (MDS): why hypercellular marrow strongly favors accelerated apoptosis. Biochem Cell Biol 91(5):303–308
Das M, Chatterjee S, Basak P, Das P, Pereira JA, Dutta RK, Chaklader M, Chaudhuri S, Law S (2009) Sca-1/c-kit receptor expression and apoptosis pattern in ENU induced MDS mice. J Stem Cells 4(4):229–241
Wrotnowski U, Innes DJ, Hobson AS (1987) Nonspecific esterase staining patterns in acute monocytic leukemia. Am J Clin Pathol 87:515–518
Chatterjee R, Chattopadhyay S, Law S (2016) Deregulation of vital mitotic kinase phosphatase signaling in hematopoietic stem/progenitor compartment leads to cellular catastrophe in experimental aplastic anemia. Mol Cell Biochem 422:121–134
Chatterjee R, Chattopadhyay S, Law S (2016) Alteration of classical and hematopoiesis specific p53 pathway in the bone marrow hematopoietic stem/progenitor compartment facilitates leukemia progression in experimental mice. Leukemia Res 47:70–77
Gajkowska A, Oldak T, Jastrzewska M, Machaj EK, Walewski J, Kraszewska E, Pojda Z (2006) Flow cytometric enumeration of CD34þ hematopoietic stem and progenitor cells in leukapheresis product and bone marrow for clinical transplantation: a comparison of three methods. Folia Histochem Cytobiol 44:53–60
Papadaki HA, Tsagournisakis M, Mastorodemos V, Pontikoglou C, Damianaki A, Pyrovolaki A et al (2005) Normal bone marrow hematopoietic stem cell reserves and normal stromal cell function support the use of autologous stem cell transplantation in patients with multiple sclerosis, Bone marrow. Transplant 36:1053–1063
Chitteti BR, Cheng YH, Rodriguez-Rodriguez S, Carlesso N, Kacena M, Srour E (2010) Hierarchical organization of osteoblasts and their impact on hematopoietic stem cell maintenance and function. Blood 116(21):1611
Galán-Díez M, Kousteni S (2017) The osteoblastic niche in hematopoiesis and hematological myeloid malignancies. Curr Mol Biol Rep 3(2):53–62
Park JH, Lee NK, Lee SY (2017) Current understanding of RANK signaling in osteoclast differentiation and maturation. Mol Cells 40(10):706–713
Chen X, Zhi X, Wang J et al (2018) RANKL signaling in bone marrow mesenchymal stem cells negatively regulates osteoblastic bone formation. Bone Res 6:34
Leibbrandt A, Penninger JM (2008) RANK/RANKL: regulators of immune responses and bone physiology. Ann N Y Acad Sci 1143:123–150
Frisch BJ, Ashton JM, Xing L, Becker MW, Jordan CT, Calvi LM (2012) Functional inhibition of osteoblastic cells in an in vivo mouse model of myeloid leukemia. Blood 119(2):540–550
Lévesque JP, Helwani FM, Winkler IG (2010) The endosteal 'osteoblastic' niche and its role in hematopoietic stem cell homing and mobilization. Leukemia 24(12):1979–1992
Hoggatt J, Pelus LM (2011) Mobilization of hematopoietic stem cells from the bone marrow niche to the blood compartment. Stem Cell Res Ther 2:13
Ling KW, Ottersbach K, van Hamburg JP, Oziemlak A, Tsai FY, Orkin SH, Ploemacher R, Hendriks RW, Dzierzak E (2004) GATA-2 plays two functionally distinct roles during the ontogeny of hematopoietic stem cells. J Exp Med 200:871–882
Avellino R, Delwel R (2017) Expression and regulation of C/EBPα in normal myelopoiesis and in malignant transformation. Blood 129(15):2083–2091
Lévesque J-P, Winkler IG, Larsen SR, Rasko JEJ (2007) Bone marrow-derived progenitors. Springer, Berlin, pp 3–37
Hosokawa K, Arai F, Yoshihara H, Iwasaki H, Nakamura Y, Gomei Y et al (2010) Knockdown of N-cadherin suppresses the long-term engraftment of hematopoietic stem cells. Blood 116:554–563
Acknowledgements
We are thankful to the Department of Biotechnology, Government of West Bengal for the financial assistance {Sanction No. 124 (A)-BT (Estt)/RD-3/12 dt.27.2.13} and Department of Science and Technology, Government of India, [No. DST/INSPIRE Fellowship/2015/IF150411] for their sponsorship. We are grateful to the Director of the Calcutta School of Tropical Medicine (Kolkata) for his encouragement and support for the successful completion of this work. Authors also acknowledge the Head of the Department of Biological Sciences, Presidency University for fluorescence microscopy facility, CRNN(Centre for Research in Nanoscience And Nanotechnology) for their electron microscopy facility and IIT Kharagpur, Central Research Facility for the Micro CT facility.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors unanimously declared no potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Daw, S., Law, S. The functional interplay of transcription factors and cell adhesion molecules in experimental myelodysplasia including hematopoietic stem progenitor compartment. Mol Cell Biochem 476, 535–551 (2021). https://doi.org/10.1007/s11010-020-03920-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-020-03920-6