Abstract
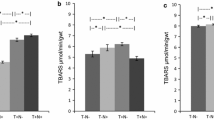
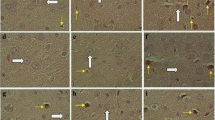
Nandrolone decanoate (ND), an anabolic–androgenic steroid prohibited in collegiate and professional sports, is associated with detrimental cardiovascular effects through redox-dependent mechanisms. We previously observed that high-dose short-term ND administration (15 mg/kg for 2 weeks) did not induce left heart ventricular hypertrophy and, paradoxically, improved postischemic response, whereas chronic ND treatment (5 mg/kg twice a week for 10 weeks) significantly reduced the cardioprotective effect of postconditioning, with an increase in infarct size and a decrease in cardiac performance. We wanted to determine whether short-term ND administration could affect the oxidative redox status in animals exposed to acute restraint stress. Our hypothesis was that, depending on treatment schedule, ND may have a double-edged sword effect. Measurement of malondialdehyde and 4-hydroxynonenal, two oxidative stress markers, in rat plasma and left heart ventricular tissue, revealed that the levels of both markers were increased in animals exposed to restraint stress, whereas no increase in marker levels was noted in animals pretreated with ND, indicating a possible protective action of ND against stress-induced oxidative damage. Furthermore, isolation and identification of proteins extracted from the left heart ventricular tissue samples of rats pretreated or not with ND and exposed to acute stress showed a prevalent expression of enzymes involved in amino acid synthesis and energy metabolism. Among other proteins, peroxiredoxin 6 and alpha B-crystallin, both involved in the oxidative stress response, were predominantly expressed in the left heart ventricular tissues of the ND-pretreated rats. In conclusion, ND seems to reduce oxidative stress by inducing the expression of antioxidant proteins in the hearts of restraint-stressed animals, thus contributing to amelioration of postischemic heart performance.






Similar content being viewed by others
References
Kicman AT (2008) Pharmacology of anabolic steroids. Br J Pharmacol 154:502–521. doi:10.1038/bjp.2008.165
Nieschlag E, Vorona E (2015) Mechanisms in endocrinology: medical consequences of doping with anabolic androgenic steroids: effects on reproductive functions. Eur J Endocrinol 173:R47–R58. doi:10.1530/EJE-15-0080
Nieschlag E, Vorona E (2015) Doping with anabolic androgenic steroids (AAS): adverse effects on non-reproductive organs and functions. Rev Endocr Metab Disord 16:199–211. doi:10.1007/s11154-015-9320-5
Hartgens F, Kuipers H (2004) Effects of androgenic-anabolic steroids in athletes. Sports Med 34:513–554
Turillazzi E, Perilli G, Di Paolo M, Neri M, Riezzo I, Fineschi V (2011) Side effects of AAS abuse: an overview. Mini Rev Med Chem 11:374–389
Bird SR, Goebel C, Burke LM, Greaves RF (2016) Doping in sport and exercise: anabolic, ergogenic, health and clinical issues. Ann Clin Biochem 53:196–221
Achar S, Rostamian A, Narayan SM (2010) Cardiac and metabolic effects of anabolic-androgenic steroid abuse on lipids, blood pressure, left ventricular dimensions, and rhythm. Am J Cardiol 106(6):893–901. doi:10.1016/j.amjcard.2010.05.013
Vanberg P, Atar D (2010) Androgenic anabolic steroid abuse and the cardiovascular system. Handb Exp Pharmacol 195:411–457. doi:10.1007/978-3-540-79088-4_18
Riezzo I, De Carlo D, Neri M, Nieddu A, Turillazzi E, Fineschi V (2011) Heart disease induced by AAS abuse, using experimental mice/rats models and the role of exercise-induced cardiotoxicity. Mini Rev Med Chem 11:409–424. doi:10.2174/138955711795445862
Vasilaki F, Tsitsimpikou C, Tsarouhas K, Germanakis I, Tzardi M, Kavvalakis M, Ozcagli E, Kouretas D, Tsatsakis AM (2016) Cardiotoxicity in rabbits after long-term nandrolone decanoate administration. Toxicol Lett 241:143–151
Nikolic TR, Zivkovic VI, Srejovic IM, Radovanovic DS, Jeremic NS, Jevdjevic MD, Djuric DM, Jakovljevic VL (2016) Acute effects of nandrolone decanoate on cardiodynamic parameters in isolated rat heart. Can J Physiol Pharmacol 94:1048–1057
Langfort J, Jagsz S, Dobrzyn P, Brzezinska Z, Klapcinska B, Galbo H (2010) Testosterone affects hormone-sensitive lipase (HSL) activity and lipid metabolism in the left ventricle. Biochem Biophys Res Commun 399:670–676. doi:10.1016/j.bbrc.2010.07.140
Liu J, Tsang S, Wong TM (2006) Testosterone is required for delayed cardioprotection and enhanced heat shock protein 70 expression induced by preconditioning. Endocrinology 147:4569–4577. doi:10.1210/en.2006-0297
Borst SE, Quinbry JC, Yarrow JF, Conover CF, Powers SK (2010) Testosterone administration induces protection against global myocardial ischemia. Horm Metab Res 42:122–129. doi:10.1055/s-0029-1241843
Powers SK, Demirel HA, Vincent HK, Coombes JS, Naito H, Hamilton KL, Shanely RA, Jessup J (1998) Exercise training improves myocardial tolerance to in vivo ischemia-reperfusion in the rat. Integr Comp Physiol 275:R1468–R1477
Hamilton KL, Powers SK, Sugiura T, Kim S, Lennon S, Tumer N, Mehta JL (2001) Short-term exercise training can improve myocardial tolerance to I/R without elevation in heat shock proteins. Physiology 281:H1346–H1352
Chaves E, Pereira PPJ, Fortunato RS, Masuda MO, de Carvalho AC, de Carvalho DP, Oliveira MF, Nascimento JH (2006) Nandrolone decanoate impairs exercise-induced cardioprotection: role of antioxidant enzymes. J Steroid Biochem Mol Biol 99:223–230. doi:10.1016/j.jsbmb.2006.01.004
Frankenfeld SP, Oliveira LP, Ortenzi VH, Rego-Monteiro IC, Chaves EA, Ferreira AC, Leitão AC, Carvalho DP, Fortunato RS (2014) The anabolic androgenic steroid nandrolone decanoate disrupts redox homeostasis in liver, heart and kidney of male Wistar rats. PLoS One 9:9
Tanno AP, das Neves VJ, Rosa KT, Cunha TS, Giordano FC, Calil CM, Guzzoni V, Fernandes T, de Oliveira EM, Novaes PD, Irigoyen MC, Moura MJ, Marcondes FK (2011) Nandrolone and resistance training induce heart remodeling: role of fetal genes and implications for cardiac pathophysiology. Life Sci 89:631–637
Franquni JV, do Nascimento AM, de Lima EM, Brasil GA, Heringer OA, Cassaro KO, da Cunha TV, Musso C, Santos MCS, Kalil IC, Endringer DC, Boëchat GA, Bissoli NS, de Andrade TU (2013) Nandrolone decanoate determines cardiac remodelling and injury by an imbalance in cardiac inflammatory cytokines and ACE activity, blunting of the Bezold-Jarisch reflex, resulting in the development of hypertension. Steroids 78:379–385
Frati P, Busardò FP, Cipolloni L, Dominicis ED, Fineschi V (2015) Anabolic androgenic steroid (AAS) related deaths: autoptic, histopathological and toxicological findings. Curr Neuropharmacol 13:146–159
Chaves EA, Fortunato RS, Carvalho DP, Hamilton KL, Nascimento JH, Oliveira MF (2013) Exercise-induced cardioprotection is impaired by anabolic steroid treatment through a redox-dependent mechanism. J Steroid Biochem Mol Biol 138:267–272. doi:10.1016/j.jsbmb.2013.06.006
Du Toit EF, Rossouw E, Van Rooyen J, Lochner A (2005) Proposed mechanisms for the anabolic steroid-induced increase in myocardial susceptibility to ischaemia/reperfusion injury. Cardiovasc J S Afr 16:21–28
Rocha FL, Carmo EC, Roque FR, Hashimoto NY, Rossoni LV, Frimm C, Aneas I, Negrão CE, Krieger JE, Oliveira EM (2007) Anabolic steroids induce cardiac renin-angiotensin system and impair the beneficial effects of aerobic training in rats. Am J Physiol Heart Circ Physiol 293:H3575–H3583. doi:10.1152/ajpheart.01251.2006
Medei E, Marocolo M, Rodrigues DC, Arantes PC, Takiya CM, Silvia J, Rondinelli E, Goldenberg RC, De Carvalho AC, Nascimento JH (2010) Chronic treatment with anabolic steroids induces ventricular repolarization disturbances: cellular, ionic and molecular mechanism. J Mol Cell Cardiol 49:165–175. doi:10.1016/j.yjmcc.2010.04.014
Penna C, Abbadessa G, Mancardi D, Tullio F, Piccione F, Spaccamiglio A, Racca S, Pagliaro P (2008) Synergistic effects against post-ischemic cardiac dysfunction by sub-chronic nandrolone pretreatment and postconditioning: role of beta2-adrenoceptor. J Physiol Pharmacol 59(4):645–659
Penna C, Tullio F, Perrelli MG, Moro F, Abbadessa G, Piccione F, Carriero V, Racca S, Pagliaro P (2011) Ischemia/reperfusion injury is increased and cardioprotection by a postconditioning protocol is lost as cardiac hypertrophy develops in nandrolone treated rats. Basic Res Cardiol 106:409–420. doi:10.1007/s00395-010-0143-y
Şahin E, Gümüşlü S (2007) Immobilization stress in rat tissues: alterations in protein oxidation, lipid peroxidation and antioxidant defense system. Comp Biochem Physiol Toxicol Pharmacol 144:342–347. doi:10.1016/j.cbpc.2006.10.009
Atif F, Yousuf S, Agarwal SK (2008) Restraint stress-induced oxidative damage and its amelioration with selenium. Eur J Pharmacol 600:59–63. doi:10.1016/j.ejphar.2008.09.029
Penna C, Abbadessa G, Mancardi D, Spaccamiglio A, Racca S, Pagliaro S (2007) Nandrolone-pretreatment enhances cardiac beta(2)-adrenoceptor expression and reverses heart contractile down-regulation in the post-stress period of acute stressed rats. J Steroid Biochem Mol Biol 107:106–113. doi:10.1016/j.jsbmb.2007.05.005
Pope HG Jr, Katz DL (1994) Psychiatric and medical effects of anabolic-androgenic steroid use. A controlled study of 160 athletes. Arch Gen Psychiatry 51:375–382. doi:10.1001/archpsyc.1994.03950050035004
Sweerts BW, Jarrott B, Lawrence AJ (1999) Expression of preprogalanin mRNA following acute and chronic restraint stress in brains of normotensive and hypertensive rats. Mol Brain Res 69:113–123. doi:10.1016/S0169-328X(99)00095-9
Tsuchida M, Miura T, Mizutani K, Aibara K (1985) Fluorescent substances in mouse and human sera as a parameter of in vivo lipid peroxidation. Biochim Biophys Acta 834:196–204
Bernheim F, Bernheim ML, Wilbur KM (1948) The reaction between thiobarbituric acid and the oxidative products of certain lipid. J Biol Chem 174:257–264
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ (1951) Protein measurement with Folin phenol reagent. J Biol Chem 193:265–275
Liu G, Feinstein SI, Wang Y, Dodia C, Fisher D, Yu K, Ho YS, Fisher AB (2010) Comparison of glutathione peroxidase 1 and peroxiredoxin 6 in protection against oxidative stress in the mouse lung. Free Radic Biol Med 49(7):1172–1181. doi:10.1016/j.freeradbiomed.2010.07.002
Xu F, Yu H, Liu J, Cheng L (2013) αB-crystallin regulates oxidative stress-induced apoptosis in cardiac H9c2 cells via the PI3K/AKT pathway. Mol Biol Rep 40:2517–2526
Madrigal JL, Olivenza R, Moro MA, Lizasoain I, Lorenzo P, Rodrigo J, Leza JC (2001) Glutathione depletion, lipid peroxidation and mitochondrial dysfunction are induced by chronic stress in rat brain. Neuropsychopharmacology 24:420–429. doi:10.1016/S0893-133X(00)00208-6
Zafir A, Banu N (2009) Modulation of in vivo oxidative status by exogenous corticosterone and restraint stress in rats. Stress 12(2):167–177. doi:10.1080/10253890802234168
Marques-Neto S, Ferraz E, Rodrigues D, Njaine B, Rondinelli E, Campos de Carvalho A, Nascimento J (2014) AT1 and aldosterone receptors blockade prevents the chronic effect of nandrolone on the exercise-induced cardioprotection in perfused rat heart subjected to ischemia and reperfusion. Cardiovasc Drugs Ther 28(2):125–135. doi:10.1007/s10557-013-6503-8
Acharjee BK, Mahanta R, Borkotoky A (2010) Nandrolone decanoate enhances the activities of cholanthrene induced glutathione-s-transferase in liver tissue of albino mice. Drug Metab Lett 4:1–6
Racca S, Piccione F, Spaccamiglio A, Carriero VM, De Francia S, Cangemi L, Esculapio P, Papotti M, Migliaretti G, Portaleone P, Di Carlo F, Abbadessa G (2012) Effects of sub-chronic nandrolone administration on hormonal adaptive response to acute stress in rats. Psychoneuroendocrinology 37:1234–1247. doi:10.1016/j.psyneuen.2011.12.017
Iuchi T, Akaike M, Mitsui T, Ohshima Y, Shintani Y, Azuma H, Matsumoto T (2003) Glucocorticoid excess induces superoxide production in vascular endothelial cells and elicits vascular endothelial dysfunction. Circ Res 92:81–87. doi:10.1161/01.RES.0000050588.35034.3c
Sato H, Takahashi T, Sumitani K, Takatsu H, Urano S (2010) Glucocorticoid generates ROS to induce oxidative injury in the hippocampus, leading to impairment of cognitive function of rats. J Clin Biochem Nutr 47:224–232. doi:10.3164/jcbn.10-58
Forman HJ, Maiorino M, Ursini F (2010) Signaling functions of reactive oxygen species. Biochemistry 49:835–842. doi:10.1021/bi9020378
Nagy N, Malik G, Fisher AB, Das DK (2006) Targeted disruption of peroxiredoxin 6 gene renders the heart vulnerable to ischemia-reperfusion injury. Am J Physiol Heart Circ Physiol 291(6):H2636–H2640. doi:10.1152/ajpheart.00399.2006
Rhee SG, Chae HZ, Kim K (2005) Peroxiredoxins: a historical overview and speculative preview of novel mechanisms and emerging concepts in cell signalling. Free Radic Biol Med 38:1543–1552. doi:10.1016/j.freeradbiomed.2005.02.026
Aggeli IK, Beis I, Gaitanaki C (2008) Oxidative stress and calpain inhibition induce alpha B-crystallin phosphorylation via p38-MAPK and calcium signalling pathways in H9c2 cells. Cell Signal 20(7):1292–1302. doi:10.1016/j.cellsig.2008.02.019
Liu S, Li J, Tao Y, Xiao X (2007) Small heat shock protein alpha B-crystallin binds to p53 to sequester its translocation to mitochondria during hydrogen peroxide-induced apoptosis. Biochem Biophys Res Commun 354:109–114. doi:10.1016/j.bbrc.2006.12.152
Shin JH, Kim SW, Lim CM, Jeong JY, Piao CS, Lee JK (2009) AlphaB-crystallin suppresses oxidative stress-induced astrocyte apoptosis by inhibiting caspase-3 activation. Neurosci Res 64:355–361. doi:10.1016/j.neures.2009.04.006
Ray PS, Martin JL, Swanson EA, Otani H, Dillmann WH, Das DK (2001) Transgene overexpression of alphaB crystallin confers simultaneous protection against cardiomyocyte apoptosis and necrosis during myocardial ischemia and reperfusion. FASEB J 15:393–402. doi:10.1096/fj.00-0199com
Morrison LE, Whittaker RJ, Klepper RE, Wawrousek EF, Glembotski CC (2004) Roles for alphaB-crystallin and HSPB2 in protecting the myocardium from ischemia-reperfusion-induced damage in a KO mouse model. Am J Physiol Heart Circ Physiol 286:H847–H855. doi:10.1152/ajpheart.00715.2003
Golenhofen N, Redel A, Wawrousek EF, Drenckhahn D (2006) Ischemia-induced increase of stiffness of alpha B-crystallin/HSPB2-deficient myocardium. Pflug Arch 451:518–525. doi:10.1007/s00424-005-1488-1
Mak S, Newton GE (2001) Vitamin C augments the inotropic response to dobutamine in humans with normal left ventricular function. Circulation 103:826–830. doi:10.1161/01.CIR.103.6.826
Kubin AM, Skouma R, Tavi P, Kόnyi A, Perjés A, Leskinen H, Ruskoaho H, Szokodi I (2011) Role of reactive oxygen species in the regulation of cardiac contractility. J Mol Cell Cardiol 50:884–893. doi:10.1016/j.yjmcc.2011.02.005
Acknowledgements
The work was supported by the research grants from the University of Torino, Ministero dell’Istruzione, dell’ Università e della Ricerca (local University funds, 2012-2014) to S. R. and B. P. We thank F. Biasi for helpful discussions during the course of this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Pergolizzi, B., Carriero, V., Abbadessa, G. et al. Subchronic nandrolone administration reduces cardiac oxidative markers during restraint stress by modulating protein expression patterns. Mol Cell Biochem 434, 51–60 (2017). https://doi.org/10.1007/s11010-017-3036-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-017-3036-7