Abstract
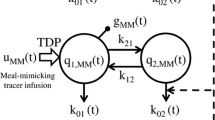
GLP-1 is an insulinotropic hormone that synergistically with glucose gives rise to an increased insulin response. Its secretion is increased following a meal and it is thus of interest to describe the secretion of this hormone following an oral glucose tolerance test (OGTT). The aim of this study was to build a mechanism-based population model that describes the time course of total GLP-1 and provides indices for capability of secretion in each subject. The goal was thus to model the secretion of GLP-1, and not its effect on insulin production. Single 75 g doses of glucose were administered orally to a mixed group of subjects ranging from healthy volunteers to patients with type 2 diabetes (T2D). Glucose, insulin, and total GLP-1 concentrations were measured. Prior population data analysis on measurements of glucose and insulin were performed in order to estimate the glucose absorption rate. The individual estimates of absorption rate constants were used in the model for GLP-1 secretion. Estimation of parameters was performed using the FOCE method with interaction implemented in NONMEM VI. The final transit/indirect-response model obtained for GLP-1 production following an OGTT included two stimulation components (fast, slow) for the zero-order production rate. The fast stimulation was estimated to be faster than the glucose absorption rate, supporting the presence of a proximal–distal loop for fast secretion from l-cells. The fast component (st 3 = 8.64·10−5 [mg−1]) was estimated to peak around 25 min after glucose ingestion, whereas the slower component (st 4 = 26.2·10−5 [mg−1]) was estimated to peak around 100 min. Elimination of total GLP-1 was characterised by a first-order loss. The individual values of the early phase GLP-1 secretion parameter (st 3 ) were correlated (r = 0.52) with the AUC(0–60 min.) for GLP-1. A mechanistic population model was successfully developed to describe total GLP-1 concentrations over time observed after an OGTT. The model provides indices related to different mechanisms of subject abilities to secrete GLP-1. The model provides a good basis to study influence of different demographic factors on these components, presented mainly by indices of the fast- and slow phases of GLP-1 response.







Similar content being viewed by others
References
Vilsboll T, Agerso H, Krarup T, Holst JJ (2003) Similar elimination rates of glucagon-like peptide-1 in obese type 2 diabetic patients and healthy subjects. J Clin Endocrinol Metab 88(1):220–224
Brandt A, Katschinski M, Arnold R, Polonsky KS, Goke B, Byrne MM (2001) GLP-1-induced alterations in the glucose-stimulated insulin secretory dose-response curve. Am J Physiol Endocrinol Metab 281(2):E242–E247
Lim GE, Brubaker PL (2006) Glucagon-like peptide 1 secretion by the L-cell. Diabetes 55(Suppl 2):S70–S77
Meier JJ, Nauck MA, Kranz D, Holst JJ, Deacon CF, Gaeckler D, Schmidt WE, Gallwitz B (2004) Secretion, degradation, and elimination of glucagon-like peptide 1 and gastric inhibitory polypeptide in patients with chronic renal insufficiency and healthy control subjects. Diabetes 53(3):654–662
Rask E, Olsson T, Söderberg S, Holst JJ, Tura A, Pacini G, Ahrén B (2004) Insulin secretion and incretin hormones after oral glucose in non-obese subjects with impaired glucose tolerance. Metabolism 53(5):624–631
Knop FK, Vilsbøll T, Højberg PV, Larsen S, Madsbad S, Vølund A, Holst JJ, Krarup T (2007) Reduced incretin effect in type 2 diabetes. Diabetes 56(8):1951–1959
Dayneka NL, Garg V, Jusko WJ (1993) Comparison of four basic models of indirect pharmacodynamic responses. J Pharmacokinet Pharmacodyn 21(4):457–478
Toft-Nielsen MB, Damholt MB, Madsbad S, Hilsted LM, Hughes TE, Michelsen BK, Holst JJ (2001) Determinants of the impaired secretion of glucagon-like peptide-1 in type 2 diabetic patients. J Clin Endocrinol Metab 86(8):3717–3723
Hansen T, Drivsholm T, Urhammer SA, Palacios RT, Vølund A, Borch-Johnsen K, Pedersen O (2007) The BIGTT test. Diabetes Care 30(2):257–262
American Diabetes Association (2004) Diagnosis and classification of diabetes mellitus. Diabetes Care 30(suppl 1):S5–S10
Andersen L, Dinesen B, Jorgensen P, Poulsen F, Roder M (1993) Enzyme immunoassay for intact human insulin in serum or plasma. Clin Chem 39(4):578–582
Orskov C, Rabenhøj L, Wettergren A, Kofod H, Holst JJ (1994) Tissue and plasma concentrations of amidated and glycine-extended glucagon-like peptide I in humans. Diabetes 43(4):535–539
Deacon CF, Pridal L, Klarskov L, Olesen M, Holst JJ (1996) Glucagon-like peptide 1 undergoes differential tissue-specific metabolism in the anesthetized pig. Am J Physiol Endocrinol Metab 271(3):E458–E464
Lima JJ, Matsushima N, Kissoon N, Wang J, Sylvester JE, Jusko WJ (2004) Modeling the metabolic effects of terbutaline in [beta]2-adrenergic receptor diplotypes[ast]. Clin Pharmacol Ther 76(1):27–37
Woo S, Pawaskar D, Jusko W (2009) Methods of utilizing baseline values for indirect response models. J Pharmacokinet Pharmacodyn 36(5):381–405
Holst JJ (2007) The physiology of glucagon-like peptide 1. Physiol Rev 87(4):1409–1439
Savic R, Jonker D, Kerbusch T, Karlsson M (2007) Implementation of a transit compartment model for describing drug absorption in pharmacokinetic studies. J Pharmacokinet Pharmacodyn 34(5):711–726
Silber HE, Frey N, Karlsson MO (2010) An integrated glucose-insulin model to describe oral glucose tolerance test data in healthy volunteers. J Clin Pharmacol 50(3):246–256
Møller J, Overgaard R, Madsen H, Hansen T, Pedersen O, Ingwersen S (2010) Predictive performance for population models using stochastic differential equations applied on data from an oral glucose tolerance test. J Pharmacokinet Pharmacodyn 37(1):85–98
Savic R, Karlsson M (2009) Importance of shrinkage in empirical Bayes estimates for diagnostics: problems and solutions. AAPS J 11(3):558–569
Rask E, Olsson T, Søderberg S, Johnson O, Seckl J, Holst JJ, Ahrén B (2001) Impaired incretin response after a mixed meal is associated with insulin resistance in nondiabetic men. Diabetes Care 24(9):1640–1645
Dalla Man C, Caumo A, Basu R, Rizza R, Toffolo G, Cobelli C (2004) Minimal model estimation of glucose absorption and insulin sensitivity from oral test: validation with a tracer method. Am J Physiol Endocrinol Metab 287(4):E637–E643
Thomaseth K, Pavan A, Berria R, Glass L, DeFronzo R, Gastaldelli A (2008) Model-based assessment of insulin sensitivity of glucose disposal and endogenous glucose production from double-tracer oral glucose tolerance test. Comput Methods Prog Biomed 89(2):132–140
Orskov C, Wettergren A, Holst JJ (1993) Biological effects and metabolic rates of glucagonlike peptide-1 7–36 amide and glucagonlike peptide-1 7–37 in healthy subjects are indistinguishable. Diabetes 42(5):658–661
Kreymann B, Ghatei MA, Williams G, Bloom SR (1987) Glucagon-like peptide-1 7–36: a physiological incretin in man. Lancet 330(8571):1300–1304
Acknowledgments
This study was partly supported by NIH Grant GM 57980 for WJJ and WG.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Møller, J.B., Jusko, W.J., Gao, W. et al. Mechanism-based population modelling for assessment of L-cell function based on total GLP-1 response following an oral glucose tolerance test. J Pharmacokinet Pharmacodyn 38, 713–725 (2011). https://doi.org/10.1007/s10928-011-9216-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10928-011-9216-2