Abstract
In recent years, telehealth visits have surged in response to the COVID-19 pandemic. However, existing structural inequities impact the access and use of information technology based on social and geographical characteristics, which is referred to as the digital divide. This has created disparities between patients with access to video visits vs. telephone visits. Previous telehealth research has focused on the completion of video visits. However, further research is needed to understand patients who decline video visits and rely on phone visits. We conducted semi-structured interviews (n = 13) of older patients (n = 9) and clinical support staff (n = 4) to understand the barriers in accessing virtual care. Most patients reported feeling left behind with telehealth, despite having access to a computer or smartphone. Clinical staff identified access to reliable technology and the ability for patients to navigate the technology as primary barriers to accessing virtual care. Many patients indicated an interest in video visits, but wanted low tech solutions and at-the-elbow support to build confidence with the technology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In response to the COVID-19 pandemic, ambulatory care nationwide expanded telehealth visits, including video visits (VV) and telephone visits (TV). At Oregon Health & Science University, telehealth appointments jumped from 2.5% of all ambulatory visits in 2019 to 51% in 2020 [1]. However, multiple studies have found inequities in this expansion, with reduced proportions of VV to TV in certain racial groups, non-English speakers, seniors and Medicaid beneficiaries [1, 2]. These inequities may reflect the impact of the digital divide: the unequal access and use of information technology based on social and geographical characteristics. VV require access to video capable technologies, reliable internet access, and digital literacy. While TV have fewer barriers, VV may be superior by allowing physical examination, building rapport, and improving provider decision-making and diagnostic accuracy [3, 4]. In order to address these developing disparities, this study aimed to uncover the barriers to VV use for patients who rely on TV for ambulatory care.
Methods
To understand both barriers and opportunities for older patients in utilization of VV, our study explored one primary research question: What barriers in accessing virtual care are there for patients who rely on phone visits? To answer this question, patients were randomly selected from a list of those who completed a TV at two ambulatory clinics in Portland, OR between 4/18/2021 and 5/18/2021 and matched target demographics of patients 65 or older, used Medicare or Medicaid, and/or identified as Black and/or Native American, and/or lived in a rural community. Clinical support staff were selected based on roles and familiarity with telehealth at the two clinics. We conducted semi-structured interviews (n = 13) of patients (n = 9) via 30-minute telephone calls and clinical support staff (n = 4) via 30-minute video conferences. Given semi-structured interviews, not all patients were asked all questions. Denominators reflect number of participants asked each question. Participants provided verbal informed consent. This study was IRB exempt. Patient and staff interview schedule (Table S1), patient interviews coding schema (Table S2) and staff interviews coding schema (Table S3) are available in Online Resource 1. The average age of the randomly sampled patient participants was 68, and a majority (n = 5, 56%) were 70 or older. A majority were Black, Indigenous, and People of Color (BIPOC) (n = 6, 67%), and a majority had Medicaid or Medicare (n = 7, 78%). Staff participants included a Care Coordinator (n = 1, 25%), a Medical Assistant Supervisor (n = 1, 25%), a Patient Access Specialist (n = 1, 25%), and a Behavioral Health Resource Specialist (n = 1, 25%). Interview data were analyzed using an inductive coding approach and three data sweeps for each data set (patients and staff). After developing a preliminary list of named codes based on the transcripts, three investigators coded the data. Four investigators then synthesized the data using affinity diagramming, a visual mapping technique common in human-centered design.
Results
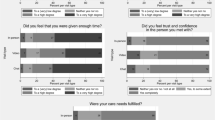
Several themes emerged from the data, including VV utility, technology confidence, and desire for assistance. Patients generally had technology access (n = 8/9, 89%), reported getting online regularly to pay bills, email, or shop (n = 6/9, 67%), and had accounts for the health system’s patient portal (n = 6/9, 67%). They reported a preference for in-person visits (n = 7/9, 78%), but also a strong interest in participating in VV (n = 6/9, 67%). Patients looked to providers for guidance about why they might consider a VV over a TV.
One patient reported, “I’m scared of video visits - don’t how they work, don’t know how to do it. Not sure if more effective than a phone visit. What’s the advantage of a video visit? I don’t know. No one has ever explained the difference and value to me.”
The most common barrier cited by patients was lack of confidence and skills with VV technology (n = 6/9, 67%). Other patient concerns included invasion of privacy and personal presentation from home (n = 2/9, 22%). Finally, patients reported a desire to have in-person help with technology and sought to avoid technical challenges in this setting (n = 5/6, 83%). For these patients, the stakes are perceived as high for a VV.
As one patient described, “I want to know and interested in how to do stuff online. I have a laptop but don’t know how to do these things.”
A majority of patient interviewees liked the idea of in-person support “with my own technology” (n = 5/6, 83%). All patients asked felt a mailed pamphlet with resources and instructions would be useful (n = 5/5, 100%). Some felt practice video calls with a help center would be useful (n = 5/7, 71%).
One patient remarked, “Having people come to my house and help me set up the technology would be great. Help during in-person appointment, I’ve had that before, it’ll be nice if the lady at the front desk helps me again.”
Interviews from the staff aligned with patient perspectives. The majority of staff reported that VV were switched to TV due to patient technology challenges (n = 3/4, 75%). These included both access to reliable technology and digital literacy.
One staff member shared, “So it’s not uncommon that if a virtual visit is suggested and can’t be done for a particular issue…typically those will get converted to a phone because they…typically can’t do the virtual visit.”
Examples of patients’ technology struggles that staff shared included remembering the login password (n = 1/4, 25%), difficulty with pre-check in requirements prior to starting a VV (n = 3/4, 75%), turning off pop-up blockers (n = 1/4, 25%), keeping up with new updates made to the electronic patient portal (n = 2/4, 50%) and lack of equipment or access to reliable internet (n = 2/4, 50%). All staff thought that in-person help in the clinic would be helpful (n = 4/4, 100%), while other ideas that were less popular included providing patients with a resource brochure (n = 2/4, 50%), a phone call a day before a VV (n = 2/4, 50%), a practice VV (n = 1/4, 25%), and a home visit for technology assistance (n = 1/4, 25%).
Discussion
While patient participants expressed a preference for in-person visits, they clearly described the potential benefits of a VV. These included avoiding unreliable medical transportation and reduced time to complete an appointment. Some reported needing information from providers about why VV are better than TV. Though many have access to technology and use it for tasks such as email, they want in-person help specific to their personal technology to build confidence in VV use. Even those who do not own internet-capable technology are interested in getting assistance to obtain and use it. Staff identified access to reliable technology and the ability for patients to navigate the technology as primary barriers to VV. They agreed with patients that in-person help would be best.
A limitation of our study is that respondents were from two academic clinical practices and therefore may reflect different perspectives than other communities.
Our findings are consistent with the literature on older adults’ use of health information technology as a whole, which includes lack of familiarity and confidence [5]. However, our findings call into question the belief that older adults are not interested in virtual care [5]. Many have stated that they are interested, but need assistance with building confidence.
Recent research on the digital divide shows that decreased access and ability to utilize technology exacerbates inequality and calls for health care organizations to join in the solution [6]. Our work answers this call. Next steps include interventions to improve the VV experience. This data demonstrates how those not using the technology may feel left behind. Future steps should actively include historically marginalized patients when prototyping solutions to ensure we target our solutions to those who would benefit most.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Sachs JW, Graven P, Gold JA, Kassakian SZ. Disparities in telephone and video telehealth engagement during the COVID-19 pandemic. JAMIA Open 2021;4(3) doi: https://doi.org/10.1093/jamiaopen/ooab056[published Online First: Epub Date]|.
Rodriguez JA, Betancourt JR, Sequist TD, Ganguli I. Differences in the use of telephone and video telemedicine visits during the COVID-19 pandemic. Am J Manag Care 2021;27(1):21–26 doi: https://doi.org/10.37765/ajmc.2021.88573[published Online First: Epub Date]|.
Rush KL, Howlett L, Munro A, Burton L. Videoconference compared to telephone in healthcare delivery: A systematic review. Int J Med Inform 2018;118:44–53 doi: https://doi.org/10.1016/j.ijmedinf.2018.07.007[published Online First: Epub Date]|.
Donaghy E, Atherton H, Hammersley V, et al. Acceptability, benefits, and challenges of video consulting: a qualitative study in primary care. Br J Gen Pract 2019;69(686):e586-e94 doi: https://doi.org/10.3399/bjgp19X704141[published Online First: Epub Date]|.
Fischer SH, David D, Crotty BH, Dierks M, Safran C. Acceptance and use of health information technology by community-dwelling elders. International journal of medical informatics 2014;83(9):624–35 doi: https://doi.org/10.1016/j.ijmedinf.2014.06.005[published Online First: Epub Date]|.
Alkureishi MA, Choo Z-Y, Rahman A, et al. Digitally Disconnected: Qualitative Study of Patient Perspectives on the Digital Divide and Potential Solutions. JMIR Hum Factors 2021;8(4):e33364 doi: 10.2196/33364[published Online First: Epub Date]|.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Hetal Choxi, Hans VanDerSchaaf, Yihan Li, Emily Morgan. The first draft of the manuscript was written by Hetal Choxi and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was reviewed by OHSU IRB and determined to be IRB exempt.
Informed consent
Verbal informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Patient Facing Systems
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Choxi, H., VanDerSchaaf, H., Li, Y. et al. Telehealth and the Digital Divide: Identifying Potential Care Gaps in Video Visit Use. J Med Syst 46, 58 (2022). https://doi.org/10.1007/s10916-022-01843-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-022-01843-x