Abstract
While data have shown that Black populations are disproportionately affected by COVID-19, few studies have evaluated birth outcomes in these understudied populations. This study hypothesized that SARS-CoV-2 infection would confer worse maternal and neonatal outcomes in a predominantly Black and underserved population in Brooklyn, New York City. In particular, SARS-CoV-2 is associated with higher rates of preterm birth, cesarean delivery, postpartum hemorrhage, lower APGAR scores, and neonatal resuscitation. Demographic factors and comorbidities were compared between the SARS-CoV-2 positive and negative groups. A retrospective cohort study was conducted in hospitalized patients who gave birth at Kings County Hospital from April 10 through June 10, 2020. Demographic and clinical data were obtained from the electronic medical record. Patients were categorized based on SARS-CoV-2 infection status and peripartum outcomes were analyzed. We used the Fisher exact test for categorical variables and the Wilcoxon rank-sum test for continuous variables. P < 0.05 was considered significant. There were no differences in obstetric or neonatal outcomes between the SARS-CoV-2 positive and negative cohorts. Most SARS-CoV-2 positive patients were asymptomatic on admission. The rates of maternal comorbidities were similar in the SARS-CoV-2 positive and negative groups. In this predominantly Black population in Brooklyn, SARS-CoV-2 infection did not confer increased risk of adverse obstetric or neonatal outcomes, despite the prevalence of comorbidities. The impact of SARS-CoV-2 infection on pregnancy outcomes is complex and may differ on a community level. Determining how COVID-19 is associated with perinatal outcomes in this minoritized patient population will augment our understanding of health disparities in order to improve care.
Similar content being viewed by others
Introduction
Knowledge about Coronavirus 19 (COVID-19) in pregnancy has evolved over the past year. Preliminary data suggested that pregnancy does not increase the risk for acquiring severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, nor does it significantly worsen the clinical course of COVID-19 compared with that of non-pregnant individuals of the same age [1,2,3]. Early studies from Wuhan, China showed that pregnant women were not at an increased risk of severe disease compared to nonpregnant patients. In fact, studies have reported that most pregnant women who are symptomatic tend to have mild disease [4, 5]. However, more recent reports from the Centers for Disease Control and Prevention (CDC) showed that pregnant women may be at increased risk for intensive care unit (ICU) admission and mechanical ventilation [6].
In non-pregnant populations, chronic underlying conditions such as hypertension, obesity, cardiovascular disease, diabetes, chronic kidney disease and chronic obstructive pulmonary disease can predispose patients to COVID-19. These underlying conditions can severely worsen disease progression and cause higher mortality rates [7, 8]. A study in the United Kingdom showed that pregnant women hospitalized for COVID-19 were more likely to be Black or minoritized, older (35 years old or over), obese, and have pre-existing comorbidities [9]. This effect persisted even after adjusting for age, body mass index (BMI), and comorbidities. While studies have shown that Black populations are disproportionately affected by COVID-19, there is a paucity of information on intrapartum outcomes in this population. The American College of Obstetricians and Gynecologists (ACOG) released a COVID-19 practice advisory that highlighted the need for additional research on racial and ethnic minoritized groups [10].
To date, comorbidities and the peripartum course of Black populations in Brooklyn as they relate to the COVID-19 pandemic remain understudied. This study hypothesized that SARS-CoV-2 infection would confer worse maternal and neonatal outcomes in a predominantly Black and underserved population in Brooklyn, New York City (NYC). In particular, SARS-CoV-2 would be associated with higher rates of preterm birth, cesarean delivery, postpartum hemorrhage, lower APGAR scores, and neonatal resuscitation. Patient demographic factors, comorbidities, birth outcomes, and SARS-CoV-2 infection were evaluated at Kings County Hospital Center (KCHC). Located in Brooklyn, KCHC belongs to the New York City Health + Hospitals (NYC H + H), the public hospitals and clinics in NYC. KCHC is a 627-bed, Level I Trauma Center serving Central Brooklyn and East Flatbush, which has the densest West Indian population in the United States [11]. This community experiences high rates of poverty, unemployment, lack of insurance, and health illiteracy [11]. The top primary languages spoken in the community include Haitian Creole, Spanish, Arabic, Bengali, Russian, French, and French Creole. The patient population is 84% Black, 6% Hispanic, 3% White, 6% Other, and 1% Asian. There are approximately 2,100 neonates delivered per year [11].
Methods
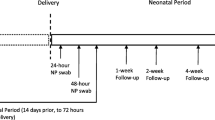
This study was approved by KCHC and NYC H + H Institutional Review Boards prior to initiation (#20–12-216–202). A retrospective observational study was conducted in hospitalized patients who gave birth at KCHC from April 10 through June 10, 2020. This time period was during the first wave of the COVID-19 pandemic and included the peak infection rate in New York City. Beginning on April 10, 2020, all patients admitted for labor were tested for SARS-CoV-2 infection by reverse transcription polymerase chain reaction (RT-PCR) nasopharyngeal swab collection.
Demographic and clinical data were abstracted from the electronic medical record, including age, race, ethnicity, parity, gestational age at delivery, prior uterine surgery, maternal symptoms on admission, and comorbidities (Table 1). Self-reported race and ethnicity were recorded with prespecified categories. Race was classified as White, Black, Asian/Indian, Native American/Pacific Islander, Other, or Unknown; ethnicity was classified as Hispanic, non-Hispanic, or Unknown. Maternal comorbidities assessed included chronic hypertension, gestational hypertension or preeclampsia, pregestational diabetes, gestational diabetes, asthma, obesity, human immunodeficiency virus (HIV), autoimmune disorders, and history of smoking. The following intrapartum outcomes were analyzed: preterm birth, mode of delivery, indication for cesarean section, postpartum hemorrhage, neonatal birthweight, APGARs at 1 and 5 min, rupture of membranes to delivery time, and the need for neonatal resuscitation. Preterm birth was defined as any vaginal or cesarean delivery at 34 to 36 + 6 weeks gestational age. Early preterm delivery was defined as any vaginal or cesarean delivery before 34 weeks gestational age. Indications for cesarean section included elective and repeat, failed labor, failed induction of labor, and emergency reasons. Failed labor refers to arrest of labor, failure to descend, and failure to progress, as defined by ACOG [12]. Postpartum hemorrhage was defined as greater than or equal to 1,000 ml (mL) of blood loss [13].
We also assessed maternal outcomes between SARS-CoV-2 positive versus negative women. Women had SARS-CoV-2 infection if the PCR test was positive, including both asymptomatic and symptomatic. Women were infectious with COVID-19 if their PCR test was positive and they had symptoms. Throughout the delivery hospitalization, symptomatic women were classified as mild, moderate, or severe disease based on the World Health Organization criteria [14, 15]. Mild COVID-19 was defined as symptoms requiring no additional oxygen supplementation (beyond standard labor and delivery care). Severe COVID-19 was defined as dyspnea (patient reported), respiratory rate 30 breaths per minute or higher, oxygen saturation 93% or less on room air, or findings consistent with pneumonia on chest X-ray, or a combination of these. Critical COVID-19 was defined as any or all of the following: respiratory failure (need for intubation and invasive ventilation), septic shock, and multiple organ dysfunction or failure.
All categorical predictors and covariates were summarized using frequency and percentage, and compared across COVID-19 status using the Fisher exact test. For multi-level categorical variables, the p-value represents the comparison of the variable’s overall distribution between the groups, not any specific level. Continuous predictor variables and covariates were summarized using median and 25th-75th percentile, or means and standard deviations where noted. Where medians were reported, a Wilcoxon rank sum test was used. Where means were reported, a t-test was performed. Statistical significance was set at 0.05, and all analyses were conducted using SAS version 9.4 (Cary, NC).
Results
We included 335 women who were admitted to KCHC for labor from April 10, 2020, to June 10, 2020. Of the 335 total women, 56 (16.7%) women were confirmed SARS-CoV-2 positive by nasopharyngeal swab testing. There were no differences in baseline characteristics between positive and negative SARS-CoV-2 groups (Table 1).
The median age overall was 30 years old. Median gravidity was three, and median parity was one. The patient population was 89.8% Black, 1.8% White, 0.6% Asian/ Indian, 6.3% Other, and 1.5% Unknown. There were 326 live births, six twin deliveries, and six stillbirths. The most common comorbidities were obesity (62.6%), gestational diabetes (14%), asthma (12.8%), gestational hypertension or preeclampsia (12.5%), and chronic hypertension (9.3%). Of the 335 patients studied, 17.4% of women had class II obesity (BMI 35 to 39.9) and 14.3% had class III obesity (BMI 40 or greater). Black women accounted for 92.9% of women in the SARS-CoV-2 positive group (52/56) and 89.1% of women in the SARS-CoV-2 negative group (246/279), which was not statistically significant (p = 0.899). Maternal COVID-19 illness severity on initial presentation was primarily asymptomatic (320/335).
Within the group of SARS-CoV-2 positive patients, the median age was 29 years old. There were no stillbirths in the SARS-CoV-2 positive group. Of those who tested positive for SARS-CoV-2, 10.7% had chronic hypertension, 14.3% had gestational hypertension or preeclampsia, 3.6% had pregestational diabetes mellitus, 10.7% had gestational diabetes mellitus and 5.4% had asthma (Table 1). None of the comorbidities examined were statistically different between the SARS-CoV-2 positive and negative groups (Table 1).
On admission, most SARS-CoV-2 positive patients (85.7%, 48/56) were asymptomatic and remained asymptomatic throughout their hospitalization. Only 14.3% (8/56) of women who tested positive for SARS-CoV-2 were symptomatic. Of the eight symptomatic patients, 50% (4/8) reported cough, 75% (6/8) were febrile, one reported dyspnea, gastrointestinal symptoms, and fatigue (12.5%). Fifty percent of patients (4/8) reported other nonspecific symptoms including myalgias and rhinorrhea. Twenty-five percent of patients (2/8) had chest x-ray findings suggestive of multifocal pneumonia due to COVID-19. Of the eight symptomatic patients, six had mild COVID-19 symptoms and two had severe COVID-19 symptoms. None of the patients included in this cohort had critical COVID-19 symptoms. However, one woman with severe COVID-19 required ICU admission and noninvasive ventilation.
There were no statistical differences in obstetrical or neonatal outcomes between SARS-CoV-2 positive and negative patients (Tables 2 and 3). The rates of preterm birth, cesarean delivery, vaginal delivery, and vaginal birth after cesarean (VBAC) were similar between the two groups. The rates of preterm birth were 14.3% (8/56) and 15% (41/279) in the SARS-CoV-2 positive and negative populations, respectively (p = 1.00). Among women who tested positive, 28.6% had cesarean deliveries and 5.4% had VBACs. In comparison, 34.8% had cesarean deliveries and 1.8% had VBACs in the negative group (p = 0.186). The indication for cesarean delivery and incidence of postpartum hemorrhage were not different between the two groups (Table 2). Birthweight, APGAR scores, and percentage of neonates requiring resuscitation were all similar between the two groups (Table 3).
Discussion
In this study comparing pregnancy outcomes in a predominantly Black patient population of Brooklyn, there were no significant differences between SARS-CoV-2 positive and negative women. Most SARS-CoV-2 positive patients were asymptomatic. The frequency of comorbidities was similar between the SARS-CoV-2 positive and SARS-CoV-2 negative groups.
In previous single-institution studies during the first wave, SARS-CoV-2 infection in pregnancy was not associated with adverse pregnancy outcomes, and the majority of patients who tested positive were asymptomatic. At Parkland Hospital in Texas, delivered women (from March 18, 2020 to August 22, 2020) with SARS-CoV-2 infection did not have a higher frequency of preterm birth, preeclampsia with severe features, or cesarean delivery for abnormal fetal heart rate [16]. There were no significant differences in other adverse pregnancy outcomes in this study by Adhikari et. al. On initial presentation, 239 women were asymptomatic or had mild disease (95%), and six of those women (3%) subsequently developed severe or critical COVID-19 [16]. At Elmhurst Hospital in Queens, NY, 72% of SARS-CoV-2 positive patients had no symptoms (from March 29, 2020 to April 22, 2020) [17]. There were no differences in preterm deliveries and mode of deliveries between the SARS-CoV-2 positive and negative groups [17]. While a study at Maimonides Medical Center in Brooklyn (from March 15, 2020 to April 15, 2020) suggested that women with COVID-19 had a greater rate of preterm birth (< 37 weeks), the sample size was small (33 symptomatic patients and 22 asymptomatic patients) [18]. Nonetheless, the rates of cesarean delivery, postpartum hemorrhage (1,000 mL or greater), preeclampsia, and length of stay were similar between symptomatic and asymptomatic patients [18].
Our data suggest a similar pattern for SARS-CoV-2 infection. Most notably, we found similar rates of preterm birth < 37 weeks (14.3% vs 15%, p = 1.00), cesarean delivery (28.6% vs 34.8%, p = 0.186), vaginal delivery (66.1% vs 63.4%, p = 0.186), and postpartum hemorrhage (13.7% vs 14.5%, p = 1.00) in the SARS-CoV-2 positive and negative cohorts. The indication for cesarean delivery, which was categorized into elective or repeat cesarean, failed labor, failed induction of labor, and emergency cesarean delivery did not differ between the two cohorts (Table 2). These findings suggest that in this unique patient population, pregnant women admitted to the hospital with positive SARS-CoV-2 infection did not have worse birth outcomes, such as higher rates of cesarean delivery, preterm birth, and maternal death.
However, multi-institutional and national studies from the first wave have demonstrated different findings. A meta-analysis showed “pre-existing comorbidities, advanced maternal age, and high body mass index seem to be risk factors for severe COVID-19 [19].” Preterm birth rates were higher in pregnant women with COVID-19 than in pregnant women without the disease [19]. A CDC report across multiple states demonstrated that only 55% of hospitalized pregnant women with COVID-19 were asymptomatic [20]. The authors Delahoy et. al. noted that the prevalence of preterm delivery in pregnant women with COVID-19 (12.6%) from March 1, 2020 to August 22, 2020 was higher than the baseline prevalence of preterm delivery in the general U.S. population in 2018 (10.0%) [20]. A study in Washington State (from March 1, 2020 to June 30, 2020) indicated that “pregnant patients with severe or critical disease were at increased risk for preterm birth when compared to women who recovered from COVID-19 (45.4% severe or critical COVID-19 vs 5.2% mild COVID-19 vs 9.0% recovered; P < 0.001) [21].” A recent publication including delivered women from 33 U.S. hospitals (from March 1, 2020 to July 1, 2020) demonstrated that “severe-critical COVID-19 was associated with increased risk of cesarean birth, hypertensive disorders of pregnancy, and preterm birth compared with asymptomatic patients [22].” The discrepancy between this data and local, community-level studies shows that state or nationwide findings may not be extrapolated to all communities.
Based on our results, the SARS-CoV-2 positive group did not have a higher incidence of comorbidities (chronic hypertension, gestational hypertension, preeclampsia, pregestational diabetes, gestational diabetes, asthma, BMI, HIV, autoimmune disorders, and smoking) compared to the SARS-CoV-2 negative group. In contrast, several studies in pregnancy illustrate a relationship between comorbidities and greater susceptibility to acquiring COVID-19. One study found asthma to be more prevalent among COVID-19 patients [1]. The CDC showed that the percentage of gestational diabetes was higher among women hospitalized for COVID-19 (25.6%) than among those hospitalized for obstetric reasons (8.1%) [23]. The authors Panagiotakopoulos et. al. found that pregnant women hospitalized for COVID-19 had higher rates of pre-pregnancy obesity (44%) than asymptomatic women hospitalized for obstetric reasons (31%) [23]. While our study suggests no increase in susceptibility of acquiring or carrying SARS-CoV-2 among patients with comorbidities, we cannot support this association with COVID-19 given the small sample size.
An ongoing challenge lies in the prediction of patients admitted with SARS-CoV-2 infection who will develop clinically significant COVID-19 that may affect birth outcomes. We found that rates of cough, fever, and other symptoms on admission were higher in SARS-CoV-2 positive patients (p = 0.0009), but 85.7% of SARS-CoV-2 positive patients remained asymptomatic. One study in NYC demonstrated that pregnant women who initially presented with symptoms were more likely to need respiratory support [18]. Despite these findings, symptoms on admission may not be reliable due to high rates of asymptomatic viremia in pregnancy [24,25,26]. A study including five NYC hospitals demonstrated that 61.4% of pregnant patients were asymptomatic on admission [27]. Washington University of St. Louis Barnes-Jewish Hospital discovered that “the pre-procedural asymptomatic infection rate was 15.7 times higher in the obstetrical population versus the general surgical population on admission [26].” These studies indicate a possible haphazard association between initial symptomatology and disease progression; therefore, relying on symptoms to predict outcomes is difficult.
The limitations of this study include its retrospective and observational design, small sample size, and minimal patients with symptomatic SARS-CoV-2 infection (COVID-19). COVID-19 sub-group analysis was not conducted due to an inadequate sample size. Up to 25% of patients did not have their ethnicity noted in the electronic medical record. Test results could be false negatives (17%) or contain an inadequate sample [28]. If collected too early in the onset of illness, the virus may be undetectable. This study did not assess for social determinants of health such as insurance status, type of housing, income, and the number of cohabitants in the household, which could augment our understanding of health disparities. Key strengths are the adoption of universal testing and 98.5% complete racial data. This data set analyzed outcomes on a community level in a predominantly Black patient population. The study occurred during the first wave, which encompassed the peak rates of COVID-19 in our community. We believe that this study accurately captured pregnant women with COVID-19 infection and did not miss a subset of sicker women. In our hospital, 16.7% of women were SARS-CoV-2 positive, which is comparable to the New York City infectivity rate of approximately 15% during this time [29].
In summary, our results showed no significant differences in perinatal outcomes between SARS-CoV-2 positive and negative women. This study highlights that the impact of SARS-CoV-2 infection on perinatal outcomes differ greatly based on region and scale. Additionally, using initial symptomatology and preexisting comorbidities as prognostic factors in COVID-19 is difficult. Most SARS-CoV-2 positive patients were asymptomatic on admission; only 16.7% of patients tested positive for SARS-CoV-2 and 2.4% developed COVID-19. Maternal comorbidities did not confer an increased risk of acquiring SARS-CoV-2 infection.
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Andrikopoulou, M., Madden, N., Wen, T., Aubey, J. J., Aziz, A., Baptiste, C. D., et al. (2020). Symptoms and Critical Illness Among Obstetric Patients With Coronavirus Disease 2019 (COVID-19) Infection. Obstetrics and Gynecology, 136(2), 291–299.
Breslin, N., Baptiste, C., Gyamfi-Bannerman, C., Miller, R., Martinez, R., Bernstein, K., et al. (2020). COVID-19 infection among asymptomatic and symptomatic pregnant women: Two weeks of confirmed presentations to an affiliated pair of New York City hospitals. Am J Obstet Gynecol MFM. https://doi.org/10.1016/j.ajogmf.2020.100118.
Yang, Z., Wang, M., Zhu, Z., Liu, Y., & Coronavirus disease, . (2019). (COVID-19) and pregnancy: a systematic review. The Journal of Maternal-Fetal & Neonatal Medicine, 2020, 1–4.
Chen, H., Guo, J., Wang, C., Luo, F., Yu, X., Zhang, W., et al. (2020). Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet, 395(10226), 809–815.
Chen, L., Li, Q., Zheng, D., Jiang, H., Wei, Y., Zou, L., et al. (2020). Clinical Characteristics of Pregnant Women with Covid-19 in Wuhan, China. N Engl J Med. https://doi.org/10.1056/NEJMc2009226.
Ellington, S., Strid, P., Tong, V. T., Woodworth, K., Galang, R. R., Zambrano, L. D., et al. (2020). Characteristics of Women of Reproductive Age with Laboratory-Confirmed SARS-CoV-2 Infection by Pregnancy Status - United States, January 22-June 7, 2020. MMWR. Morbidity and Mortality Weekly Report, 69(25), 769–775.
Chen, T., Wu, D., Chen, H., Yan, W., Yang, D., Chen, G., et al. (2020). Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ, 368, m1091.
Emami, A., Javanmardi, F., Pirbonyeh, N., & Akbari, A. (2020). Prevalence of Underlying Diseases in Hospitalized Patients with COVID-19: a Systematic Review and Meta-Analysis. Arch Acad Emerg Med., 8(1), e35.
Knight, M., Bunch, K., Vousden, N., Morris, E., Simpson, N., Gale, C., et al. (2020). Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: national population based cohort study. BMJ, 369, m2107.
Gynecologists TACoOa. Novel Coronavirus 2019 (COVID-19) Practice Advisory. 2020.
Kings County Hospital Community Health Needs Assessment (CHNA) and Implementation Strategy Plan: NYC Health and Hospitals Kings County Hospital; 2019 [cited 2019 06/30]. Available from: https://www.nychealthandhospitals.org/kingscounty/community-health-needs-assessment-report/.
Safe prevention of the primary cesarean delivery. (2014). Obstetric Care Consensus No. 1. American College of Obstetricians and Gynecologists. Obstet Gynecol., 123, 693–711.
Postpartum hemorrhage. (2017). Practice Bulletin No. 183. American College of Obstetricians and Gynecologists. Obstet Gynecol., 130, e168-86.
Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19). World Health Organization.
Wu, J. T., Leung, K., Bushman, M., Kishore, N., Niehus, R., de Salazar, P. M., et al. (2020). Estimating clinical severity of COVID-19 from the transmission dynamics in Wuhan. China. Nat Med., 26(4), 506–510.
Adhikari, E. H., Moreno, W., Zofkie, A. C., MacDonald, L., McIntire, D. D., Collins, R. R. J., et al. (2020). Pregnancy Outcomes Among Women With and Without Severe Acute Respiratory Syndrome Coronavirus 2 Infection. JAMA Network Open, 3(11), e2029256.
Maru, S., Patil, U., Carroll-Bennett, R., Baum, A., Bohn-Hemmerdinger, T., Ditchik, A., et al. (2020). Universal screening for SARS-CoV-2 infection among pregnant women at Elmhurst Hospital Center, Queens, New York. PLoS ONE, 15(12), e0238409.
London, V., McLaren, R., Jr., Atallah, F., Cepeda, C., McCalla, S., Fisher, N., et al. (2020). The Relationship between Status at Presentation and Outcomes among Pregnant Women with COVID-19. American Journal of Perinatology, 37(10), 991–994.
Allotey, J., Stallings, E., Bonet, M., Yap, M., Chatterjee, S., Kew, T., et al. (2020). Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ, 370, m3320.
Delahoy, M. J. W. M., O’Halloran, A., et al. (2020). Characteristics and Maternal and Birth Outcomes of Hospitalized Pregnant Women with Laboratory-Confirmed COVID-19—COVID-NET, 13 States, March 1–August 22, 2020. MMWR. Morbidity and Mortality Weekly Report, 69, 1347–1354.
Lokken, E. M., Huebner, E. M., Taylor, G. G., Hendrickson, S., Vanderhoeven, J., Kachikis, A., et al. (2021). Disease severity, pregnancy outcomes, and maternal deaths among pregnant patients with severe acute respiratory syndrome coronavirus 2 infection in Washington State. Am J Obstet Gynecol. https://doi.org/10.1016/j.ajog.2020.12.1221.
Metz, T. D., Clifton, R. G., Hughes, B. L., Sandoval, G., Saade, G. R., Grobman, W. A., et al. (2021). Disease Severity and Perinatal Outcomes of Pregnant Patients With Coronavirus Disease 2019 (COVID-19). Obstetrics and Gynecology, 137(4), 571–580.
Panagiotakopoulos, L. M. T., Gee, J., et al. (2020). SARS-CoV-2 Infection Among Hospitalized Pregnant Women: Reasons for Admission and Pregnancy Characteristics—Eight U.S. Health Care Centers, March 1–May 30, 2020. MMWR Morb Mortal Wkly Rep. https://doi.org/10.15585/mmwr.mm6938e2.
Miller, E. S., Grobman, W. A., Sakowicz, A., Rosati, J., & Peaceman, A. M. (2020). Clinical Implications of Universal Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Testing in Pregnancy. Obstetrics and Gynecology, 136(2), 232–234.
Fox, N. S., & Melka, S. (2020). COVID-19 in Pregnant Women: Case Series from One Large New York City Obstetrical Practice. American Journal of Perinatology, 37(10), 1002–1004.
Kelly, J. C. R. N., Palanisamy, A., Stout, M. J., & Carter, E. B. (2020). Pre-procedural asymptomatic COVID-19 in obstetric and surgical units. American Journal of Obstetrics and Gynecology. https://doi.org/10.1016/j.ajog.2020.09.023.
Khoury, R., Bernstein, P. S., Debolt, C., Stone, J., Sutton, D. M., Simpson, L. L., et al. (2020). Characteristics and Outcomes of 241 Births to Women With Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection at Five New York City Medical Centers. Obstetrics and Gynecology, 136(2), 273–282.
Kanji, J. N., Zelyas, N., MacDonald, C., Pabbaraju, K., Khan, M. N., Prasad, A., et al. (2021). False negative rate of COVID-19 PCR testing: a discordant testing analysis. Virol J., 18(1), 13.
Sutton, D., Fuchs, K., D’Alton, M., & Goffman, D. (2020). Universal Screening for SARS-CoV-2 in Women Admitted for Delivery. N Engl J Med. https://doi.org/10.1056/NEJMc2009316.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Not applicable.
Corresponding author
Ethics declarations
Conflict of interest
Not applicable.
Ethical Approval
Not applicable.
Consent to Participate
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, C., Andrusier, M., Silver, M. et al. Effect of SARS-CoV-2 Infection on Pregnancy Outcomes in an Inner-City Black Patient Population. J Community Health 46, 1029–1035 (2021). https://doi.org/10.1007/s10900-021-00988-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-021-00988-z