Abstract
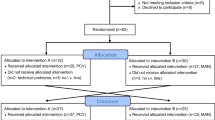
Paratracheal pressure has been recently suggested to compress and occlude the upper esophagus at the lower left paratracheal region to prevent gastric regurgitation alternative to cricoid pressure. It also prevents gastric insufflation. The aim of this randomized cross-over study was to investigate the effectiveness of paratracheal pressure on mask ventilation in obese anesthetized paralyzed patients. After the induction of anesthesia, two-handed mask ventilation was initiated in a volume-controlled mode with a tidal volume of 8 mL kg‒1 based on ideal body weight (IBW), a respiratory rate of 12 breaths min− 1, and positive end-expiratory pressure of 10 cmH2O. Expiratory tidal volume and peak inspiratory pressure were recorded alternately with or without the application of 30 Newtons (approximately 3.06 kg) paratracheal pressure during a total of 16 successive breaths over 80 s. Association of patient characteristics with the effectiveness of paratracheal pressure on mask ventilation, defined as the difference in expiratory tidal volume between the presence or absence of paratracheal pressure were evaluated. In 48 obese anesthetized paralyzed patients, expiratory tidal volume was significantly higher with the application of paratracheal pressure than without paratracheal pressure [496.8 (74.1) mL kg− 1 of IBW vs. 403.8 (58.4) mL kg− 1 of IBW, respectively; P < 0.001]. Peak inspiratory pressure was also significantly higher with the application of paratracheal pressure compared to that with no paratracheal pressure [21.4 (1.2) cmH2O vs. 18.9 (1.6) cmH2O, respectively; P < 0.001]. No significant association was observed between patient characteristics and the effectiveness of paratracheal pressure on mask ventilation. Hypoxemia did not occur in any of the patients during mask ventilation with or without paratracheal pressure. The application of paratracheal pressure significantly increased both the expiratory tidal volume and peak inspiratory pressure during face-mask ventilation with a volume-controlled mode in obese anesthetized paralyzed patients. Gastric insufflation was not evaluated in this study during mask ventilation with or without paratracheal pressure.


Similar content being viewed by others
References
Bouvet L, Albert ML, Augris C, Boselli E, Ecochard R, Rabilloud M, et al. Real-time detection of gastric insufflation related to facemask pressure-controlled ventilation using ultrasonography of the antrum and epigastric auscultation in nonparalyzed patients: a prospective, randomized, double-blind study. Anesthesiology. 2014;120:326–34.
Kheterpal S, Han R, Tremper KK, Shanks A, Tait AR, O’Reilly M, et al. Incidence and predictors of difficult and impossible mask ventilation. Anesthesiology. 2006;105:885–91.
Domi R, Laho H. Anesthetic challenges in the obese patient. J Anesth. 2012;26:758–65.
Strandberg A, Tokics L, Brismar B, Lundquist H, Hedenstierna G. Constitutional factors promoting development of atelectasis during anaesthesia. Acta Anaesthesiol Scand. 1987;31:21–4.
Eichenberger A, Proietti S, Wicky S, Frascarolo P, Suter M, Spahn DR, et al. Morbid obesity and postoperative pulmonary atelectasis: an underestimated problem. Anesth Analg. 2002;95:1788–92. table of contents.
Coussa M, Proietti S, Schnyder P, Frascarolo P, Suter M, Spahn DR, et al. Prevention of atelectasis formation during the induction of general anesthesia in morbidly obese patients. Anesth Analg. 2004;98:1491–5. table of contents.
Gander S, Frascarolo P, Suter M, Spahn DR, Magnusson L. Positive end-expiratory pressure during induction of general anesthesia increases duration of nonhypoxic apnea in morbidly obese patients. Anesth Analg. 2005;100:580–4.
Cajander P, Edmark L, Ahlstrand R, Magnuson A, de Leon A. Effect of positive end-expiratory pressure on gastric insufflation during induction of anaesthesia when using pressure-controlled ventilation via a face mask: a randomised controlled trial. Eur J Anaesthesiol. 2019;36:625–32.
Zeng J, Jia ZJ, Peng L, Wei W. Detection of gastric inflation using transesophageal echocardiography after different level of pressure-controlled mask ventilation: a prospective randomized trial. J Clin Monit Comput. 2020;34:535–40.
Gautier N, Danklou J, Brichant JF, Lopez AM, Vandepitte C, Kuroda MM, et al. The effect of force applied to the left paratracheal oesophagus on air entry into the gastric antrum during positive-pressure ventilation using a facemask. Anaesthesia. 2019;74:22–8.
de Leon A, Thorn SE, Wattwil M. High-resolution solid-state manometry of the upper and lower esophageal sphincters during anesthesia induction: a comparison between obese and non-obese patients. Anesth Analg. 2010;111:149–53.
Langeron O, Masso E, Huraux C, Guggiari M, Bianchi A, Coriat P, et al. Prediction of difficult mask ventilation. Anesthesiology. 2000;92:1229–36.
Riad W, Vaez MN, Raveendran R, Tam AD, Quereshy FA, Chung F, et al. Neck circumference as a predictor of difficult intubation and difficult mask ventilation in morbidly obese patients: a prospective observational study. Eur J Anaesthesiol. 2016;33:244–9.
Won D, Kim H, Chang JE, Lee JM, Min SW, Ma S, et al. Effect of Paratracheal pressure on the Glottic View during Direct Laryngoscopy: a Randomized Double-Blind, Noninferiority Trial. Anesth Analg. 2021;133:491–9.
Cadi P, Guenoun T, Journois D, Chevallier JM, Diehl JL, Safran D. Pressure-controlled ventilation improves oxygenation during laparoscopic obesity surgery compared with volume-controlled ventilation. Br J Anaesth. 2008;100:709–16.
De Baerdemaeker LE, Van der Herten C, Gillardin JM, Pattyn P, Mortier EP, Szegedi LL. Comparison of volume-controlled and pressure-controlled ventilation during laparoscopic gastric banding in morbidly obese patients. Obes Surg. 2008;18:680–5.
Hans GA, Pregaldien AA, Kaba A, Sottiaux TM, DeRoover A, Lamy ML, et al. Pressure-controlled ventilation does not improve gas exchange in morbidly obese patients undergoing abdominal surgery. Obes Surg. 2008;18:71–6.
Pournajafian A, Sakhaeyan E, Rokhtabnak F, Alimian M, Ghodrati A, Jolousi M, et al. Comparison of pressure and volume-controlled mechanical ventilation in laparoscopic bariatric surgery: a randomized crossover trial. Anesth Pain Med. 2022;12:e123270.
Aldenkortt M, Lysakowski C, Elia N, Brochard L, Tramer MR. Ventilation strategies in obese patients undergoing surgery: a quantitative systematic review and meta-analysis. Br J Anaesth. 2012;109:493–502.
Warters RD, Szabo TA, Spinale FG, DeSantis SM, Reves JG. The effect of neuromuscular blockade on mask ventilation. Anaesthesia. 2011;66:163–7.
Goodwin MW, Pandit JJ, Hames K, Popat M, Yentis SM. The effect of neuromuscular blockade on the efficiency of mask ventilation of the lungs. Anaesthesia. 2003;58:60–3.
Herman NL, Carter B, Van Decar TK. Cricoid pressure: teaching the recommended level. Anesth Analg. 1996;83:859–63.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Taikyung Seol, Hyerim Kim, Jee-Eun Chang, Yeonsoo Kang, and Jin-Young Hwang. The first draft of the manuscript was written by Taikyung Seol, and Jin-Young Hwang, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Seol, T., Kim, H., Chang, JE. et al. Effect of paratracheal pressure on the effectiveness of mask ventilation in obese anesthetized patients: a randomized, cross-over study. J Clin Monit Comput 38, 31–36 (2024). https://doi.org/10.1007/s10877-023-01048-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-023-01048-8