Abstract
Purpose
Laryngeal Mask Airway (LMA) insertion may not always be smooth without complications. Controversial results of several studies evaluating ideal insertion conditions have been published. This study compared the oropharyngeal leak pressure values and fiberoptic grading scores between blind and video-laryngoscope-guided LMA insertion.
Methods
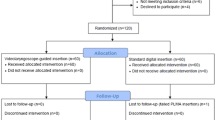
Patients were randomly assigned into blind insertion (n = 50) and video-laryngoscope guided insertion (n = 50) groups. The oropharyngeal leak pressure, peak airway pressure, fiberoptic grading score, first attempt success rate, hemodynamic parameters, and complications were recorded.
Results
All laryngeal mask airways were successfully inserted in both groups at the first attempt. The fiberoptic staging scores were: grade 1 in 8.2% of patients, grade 2 in 24.4% of patients, grade 3 in 44.8% of patients, grade 4 in 22.4% of patients in the control group. On the other hand, grade 1 in 2.2% of patients, grade 2 in 28.6% of patients, grade 3 in 51% of patients, grade 4 in 8.2% of patients in the VL group (p = 0.260). The peak airway pressure and LMA insertion time were similar between groups. However, the oropharyngeal leak pressure before extubation was significantly higher in the video-laryngoscope-guided insertion than blind insertion (36.29 ± 7.09 vs. 33.79 ± 8.84 cmH2O respectively, p = 0.04).
Conclusions
The findings of our study suggest that the video-laryngoscope-guided LMA-Classic insertion with a standard blade technique may be a helpful alternative to blind insertion.

Similar content being viewed by others
References
Seet E, Rajeev S, Firoz T, Yousaf F, Wong J, Wong DT, et al. Safety and efficacy of laryngeal mask airway supreme versus laryngeal mask airway ProSeal: a randomized controlled trial. Eur J Anaesthesiol. 2010;27:602–7.
Francksen H, Bein B, Cavus E, Renner J, Scholz J, Steinfath M, et al. Comparison of LMA Unique, Ambu laryngeal mask and soft seal laryngeal mask during routine surgical procedures. Eur J Anaesthesiol. 2007;24:134–40.
Brain AI. The laryngeal mask-a a new concept in airway management. Br J Anaesth. 1983;55:801–5.
Van Zundert AAJ, Gatt SP, Van Zundert TCRV, Kumar CM, Pandit JJ. Features of new vision-incorporated third-generation video laryngeal mask airways. J Clin Mon Comp. 2021. https://doi.org/10.1007/s10877-021-00780-3.
Van Zundert AAJ, Gatt SP, Kumar CM, Van Zundert TCRV, Pandit JJ. ‘Failed supraglottic airway’: an algorithm for suboptimally placed supraglottic airway devices based on videolaryngoscopy. Br J Anaesth. 2017;118:645–9.
Campbell RL, Biddle C, Assudmi N, Campbell JR, Hotchkiss M. Fiberoptic assessment of laryngeal mask airway placement: blind insertion versus direct visual epiglottoscopy. J Oral Maxillofac Surg. 2004;62:1108–13.
Chandan SN, Sharma SM, Raveendra US, Rajendra Prasad B. Fiberoptic assessment of laryngeal mask airway placement: a comparison of blind insertion and insertion with the use of a laryngoscope. J Maxillofac Oral Surg. 2009;8:95–8.
Kim GW, Kim JY, Kim SJ, Moon YR, Park EJ, Park SY. Conditions for laryngeal mask airway placement in terms of oropharyngeal leak pressure: a comparison between blind insertion and laryngoscope-guided insertion. BMC Anesthesiol. 2019;19:4.
Beleña JM, Núñez M, Anta D, Carnero M, Gracia JL, Ayala JL, et al. Comparison of laryngeal mask airway supreme and laryngeal mask airway Proseal with respect to oropharyngeal leak pressure during laparoscopic cholecystectomy: a randomised controlled trial. Eur J Anaesthesiol. 2013;30:119–23.
Kim HJ, Lee K, Bai S, Kim MH, Oh E, Yoo YC. Influence of head and neck position on ventilation using the air-Q® SP airway in anaesthetized paralysed patients: a prospective randomized crossover study. Br J Anaesth. 2017;118:452–7.
Van Zundert AA, Kumar CM, Van Zundert TC. Malpositioning of supraglottic airway devices: preventive and corrective strategies. Br J Anaesth. 2016;116:579–82.
Keller C, Brimacombe J, Pühringer F. A fibreoptic scoring system to assess the position of laryngeal mask airway devices. Interobserver variability and a comparison between the standard, flexible and intubating laryngeal mask airways. Anaesthesiol Intensivmed Notfallmed Schmerzther. 2000;35(11):692–4. doi:https://doi.org/10.1055/s-2000-8164.
Saracoglu KT, Demir A, Pehlivan G, Saracoglu A, Eti Z. Analysing the efficacy of the I-gel supraglottic airway device in the supine and lateral decubitus positions. Anaesthesiol Intensive Ther. 2018;50:259–62.
Saracoglu A, Saracoglu KT, Kafali IH. I have only D-blade: Is it enough? J Clin Anesth. 2016;34:68–9.
LMA. LMA Proseal™ Instruction Manual. 1st ed. San Diego: LMA North America Inc; 2000.
Zhang L, Seet E, Mehta V, Subramanyam R, Ankichetty SP, Wong DT, Chung F. Oropharyngeal leak pressure with the laryngeal mask airway Supreme™ at different intracuff pressures: a randomized controlled trial. Can J Anaesth. 2011 Jul;58:624–9.
Patil PC, Chikkapillappa MA, Pujara VS, Anandswamy TC, Parate LH, Bevinaguddaiah Y. ProSeal Laryngeal Mask Airway Placement: A Comparison of Blind versus Direct Laryngoscopic Insertion Techniques. Anesth Essays Res. 2017 Apr-Jun;11:380–4.
Joshi S, Sciacca RR, Solanki DR, Young WL, Mathru MM. A prospective evaluation of clinical tests for placement of laryngeal mask airways. Anesthesiology. 1998 Nov;89(5):1141 6. doi:https://doi.org/10.1097/00000542-199811000-00014.
Ozgul U, Erdil FA, Erdogan MA, Begec Z, Colak C, Yucel A, Durmus M. Comparison of video-laryngoscope-guided versus standard digital insertion techniques of the ProSeal™ laryngeal mask airway: a prospective randomized study. BMC Anesthesiol. 2019 Dec;30(1):244. 19 ).
Van Zundert AAJ, Kumar CM, Van Zundert TCRV, Gatt SP, Pandit JJ. The case for a 3rd generation supraglottic airway device facilitating direct vision placement. J Clin Monit Comput. 2020 Jun 15:1–8. doi: https://doi.org/10.1007/s10877-020-00537-4).
Kumar C, Van Zundert T, Seet E, Van Zundert A. Time to consider supraglottic airway device oropharyngeal leak pressure measurement more objectively. Acta Anaesthesiol Scand. 2021;65(2):142–5. https://doi.org/10.1111/aas.13727).
Van Esch BF, Stegeman I, Smit AL. Comparison of laryngeal mask airway vs tracheal intubation: a systematic review on airway complications. J Clin Anesth. 2017 Feb;36:142–50.
Frerk C, Mitchell VS, McNarry AF, Mendonca C, Bhagrath R, Patel A, O’Sullivan EP, Woodall NM, Ahmad I. Difficult Airway Society intubation guidelines working group. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015 Dec;115:827–48.
Author information
Authors and Affiliations
Contributions
Ayten Saracoglu: data curation, conceptualization, methodology, writing reviewing & editing. Tahsin Simsek: data curation, writing- original draft preparation, software, validation, investigation. Ozlem Sezen: writing- original draft preparation, conceptualization, methodology. Gul Cakmak: corresponding author, visualization, writing - reviewing & editing. Kemal Tolga Saracoglu: supervision, visualization.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The authors have no conflicts of interest to declare relevant to this article’s content.
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Marmara University Faculty of Medicine (Date 02.02.2018/ No 09.2018.134).
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Simsek, T., Saracoglu, A., Sezen, O. et al. Blind vs. video-laryngoscope-guided laryngeal mask insertion: A prospective randomized comparison of oropharyngeal leak pressure and fiberoptic grading. J Clin Monit Comput 36, 1249–1255 (2022). https://doi.org/10.1007/s10877-022-00841-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-022-00841-1