Abstract
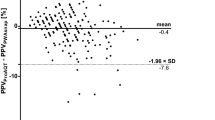
Pulse pressure variation (PPV) and stroke volume variation (SVV) can be used to assess fluid status in the operating room but usually require dedicated advanced hemodynamic monitors. Recently, a smartphone application (Capstesia™), which automatically calculates PPV from a picture of the invasive arterial pressure waveform from any monitor screen (PPVCAP), has been developed. The purpose of this study was to compare PPVCAP with SVV from an uncalibrated pulse wave analysis monitor (SVVPC). In 40 patients undergoing major abdominal surgery, we compared PPVCAP with SVVPC at post-induction, pre-incision, post-incision, end of surgery, and during every hypotensive episode (mean arterial pressure < 65 mmHg). We classified PPVCAP and SVVPC into three categories reflecting the thresholds used for the decision to administer fluids: no fluid administration (PPV and SVV < 9%), gray zone (PPV and SVV 9–13%), and fluid administration (PPV and SVV > 13%). The agreement between SVVPC and PPVCAP for these three categories was measured by the number of concordant paired measurements divided by the total number of paired measurements and Cohen’s kappa coefficient. In the 549 pairs of PPV–SVV data obtained, the overall agreement of PPVCAP with SVVPC was 79%, and the kappa coefficient was moderate (0.55). The highest agreement and kappa coefficient value were observed after the induction of anesthesia before surgical incision. PPVCAP and SVVPC would have resulted in completely opposite clinical decisions regarding fluid administration in 1% of the cases. In this clinical decision making study in patients undergoing major abdominal surgery, we observed a moderate agreement between PPVCAP and SVVPC with regard to categories used to guide fluid administration.
Trial Registration: Clinical Trials.gov (NCT03137901).


Similar content being viewed by others
Notes
Carstensen et al. [22]
References
Michard F, Chemla D, Richard C, et al. Clinical use of respiratory changes in arterial pulse pressure to monitor the hemodynamic effects of PEEP. Am J Respir Crit Care Med. 1999;159:935–9.
Michard F, Boussat S, Chemla D, et al. Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med. 2000;162:134–8.
Marik PE, Cavallazzi R, Vasu T, Hirani A. Dynamic changes in arterial waveform derived variables and fluid responsiveness in mechanically ventilated patients: a systematic review of the literature. Crit Care Med. 2009;37:2642–7.
Monnet X, Marik PE, Teboul JL. Prediction of fluid responsiveness: an update. Ann Intensive Care. 2016;6:111.
Yang X, Du B. Does pulse pressure variation predict fluid responsiveness in critically ill patients? a systematic review and meta-analysis. Crit Care. 2014;18:650.
Joosten A, Tircoveanu R, Arend S, Wauthy P, Gottignies P, Van der Linden P. Impact of balanced tetrastarch raw material on perioperative blood loss: a randomized double blind controlled trial. Br J Anaesth. 2016;117:442–9.
Michard F, Giglio MT, Brienza N. Perioperative goal-directed therapy with uncalibrated pulse contour methods: impact on fluid management and postoperative outcome. Br J Anaesth. 2017;119:22–30.
Ramsingh DS, Sanghvi C, Gamboa J, Cannesson M, Applegate RL. Outcome impact of goal directed fluid therapy during high risk abdominal surgery in low to moderate risk patients: a randomized controlled trial. J Clin Monit Comput. 2013;27:249–57.
Malbouisson LMS, Silva JM Jr, Carmona MJC, et al. A pragmatic multi-center trial of goal-directed fluid management based on pulse pressure variation monitoring during high-risk surgery. BMC Anesthesiol. 2017;17:70.
Cannesson M, Ramsingh D, Rinehart J, et al. Perioperative goal-directed therapy and postoperative outcomes in patients undergoing high-risk abdominal surgery: a historical-prospective, comparative effectiveness study. Crit Care. 2015;19:261.
Rinehart J, Islam T, Boud R, et al. Visual estimation of pulse pressure variation is not reliable: a randomized simulation study. J Clin Monit Comput. 2012;26:191–6.
Barrachina B, Cobos R, Mardones N, Castaneda A, Vinuesa C. Assessment of a smartphone app (Capstesia) for measuring pulse pressure variation: agreement between two methods: a cross-sectional study. Eur J Anaesthesiol. 2017;34:75–80.
Desebbe O, Joosten A, Suehiro K, et al. A novel mobile phone application for pulse pressure variation monitoring based on feature extraction technology: a method comparison study in a simulated environment. Anesth Analg. 2016;123:105–13.
Joosten A, Boudart C, Vincent JL, et al. Ability of a new smartphone pulse pressure variation and cardiac output application to predict fluid responsiveness in patients undergoing cardiac surgery. Anesth Analg. 2018. https://doi.org/10.1213/ANE.0000000000003652 (Epub ahead of print).
Shah SB, Bhargava AK, Hariharan U, Vishvakarma G, Jain CR, Kansal A. Cardiac output monitoring: a comparative prospective observational study of the conventional cardiac output monitor Vigileo and the new smartphone-based application Capstesia. Indian J Anaesth. 2018;62:584–91.
Joosten A, Coeckelenbergh S, Delaporte A, et al. Implementation of closed-loop-assisted intra-operative goal-directed fluid therapy during major abdominal surgery: a case-control study with propensity matching. Eur J Anaesthesiol. 2018;35:650–8.
Joosten A, Delaporte A, Ickx B, et al. Crystalloid versus colloid for intraoperative goal-directed fluid therapy using a closed-loop system: a randomized, double-blinded, controlled trial in major abdominal surgery. Anesthesiology. 2018;128:55–66.
Lima MF, Mondadori LA, Chibana AY, Gilio DB, Giroud Joaquim EH, Michard F. Outcome impact of hemodynamic and depth of anesthesia monitoring during major cancer surgery: a before-after study. J Clin Monit Comput. 2018. https://doi.org/10.1007/s10877-018-0190-8 (Epub ahead of print).
Cannesson M, Le Manach Y, Hofer CK, et al. Assessing the diagnostic accuracy of pulse pressure variations for the prediction of fluid responsiveness: a “gray zone” approach. Anesthesiology. 2011;115:231–41.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Carstensen B. Comparing clinical measurement methods:a practical guide.New Jersey:Wiley;2010.
Carstensen B, Gurrin L, Ekstrom C, Figurski M. MethComp: functions for analysis of agreement in method comparison studies. R package version 1.22.2. https://CRAN.R-project.org/package=MethComp (2015).
Michard F, Chemla D, Teboul JL. Applicability of pulse pressure variation: how many shades of grey? Crit Care. 2015;19:144.
Biais M, Ehrmann S, Mari A, et al. Clinical relevance of pulse pressure variations for predicting fluid responsiveness in mechanically ventilated intensive care unit patients: the grey zone approach. Crit Care. 2014;18:587.
Salzwedel C, Puig J, Carstens A, et al. Perioperative goal-directed hemodynamic therapy based on radial arterial pulse pressure variation and continuous cardiac index trending reduces postoperative complications after major abdominal surgery: a multi-center, prospective, randomized study. Crit Care. 2013;17:R191.
Saugel B, Reuter DA. Perioperative goal-directed therapy using invasive uncalibrated pulse contour analysis. Front Med (Lausanne). 2018;5:12.
Biais M, Stecken L, Martin A, Roullet S, Quinart A, Sztark F. Automated, continuous and non-invasive assessment of pulse pressure variations using CNAP((R)) system. J Clin Monit Comput. 2017;31:685–92.
Monnet X, Dres M, Ferre A, et al. Prediction of fluid responsiveness by a continuous non-invasive assessment of arterial pressure in critically ill patients: comparison with four other dynamic indices. Br J Anaesth. 2012;109:330–8.
Wacharasint P, Lertamornpong A, Wattanathum A, Wongsa A. Predicting fluid responsiveness in septic shock patients by using 3 dynamic indices: is it all equally effective? J Med Assoc Thail. 2012;95(Suppl 5):149-56.
Hong JQ, He HF, Chen ZY, et al. Comparison of stroke volume variation with pulse pressure variation as a diagnostic indicator of fluid responsiveness in mechanically ventilated critically ill patients. Saudi Med J. 2014;35:261–8.
Zhang Z, Lu B, Sheng X, Jin N. Accuracy of stroke volume variation in predicting fluid responsiveness: a systematic review and meta-analysis. J Anesth. 2011;25:904–16.
Acknowledgements
All the Anesthesiology department for their assistance.
Funding
This work was supported by the Department of Anesthesiology, Erasme Hospital, Brussels.
Author information
Authors and Affiliations
Contributions
AJ: Designed the study, analyzed the data and drafted the manuscript. AJ, OD: Designed the study, analyzed the data and edited the manuscript. JLV, SS, JR, LVO: Analyzed the data and edited the manuscript. AH: Analyzed the data (statistical analysis) and edited the manuscript. BS: Analyzed the data and drafted the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Alexandre Joosten: Consultant for Edwards Lifesciences (Irvine, CA, USA). Olivier Desebbe: Collaborates with Medtronic (Dublin, Ireland) as a consultant and received honoraria for giving lectures. Jean-Louis Vincent is Editor-in-Chief of Critical Care. He has no other conflicts related to this article. Joseph Rinehart: Ownership interest in Sironis, a company developing closed-loop medical software, consultant for Edwards Lifesciences (Irvine, CA, USA). Bernd Saugel: Collaborates with Pulsion Medical Systems (Feldkirchen, Germany) as a member of the medical advisory board and received honoraria for giving lectures and refunds of travel expenses from Pulsion Medical Systems. BS received institutional research grants, unrestricted research grants, and refunds of travel expenses from Tensys Medical (San Diego, CA, USA). BS received honoraria for giving lectures and refunds of travel expenses from CNSystems Medizintechnik (Graz, Austria). BS received honoraria for giving lectures and research support from Edwards Lifesciences (Irvine, CA, USA). All other authors have no conflicts of interest to declare.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Joosten, A., Jacobs, A., Desebbe, O. et al. Monitoring of pulse pressure variation using a new smartphone application (Capstesia) versus stroke volume variation using an uncalibrated pulse wave analysis monitor: a clinical decision making study during major abdominal surgery. J Clin Monit Comput 33, 787–793 (2019). https://doi.org/10.1007/s10877-018-00241-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-018-00241-4