Abstract
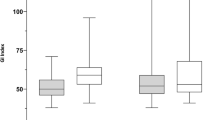
The Integrated Pulmonary Index (IPI) is an algorithm included in commercially available monitors that constitutes a representation of 4 parameters: EtCO2, RR, SpO2 and PR. The IPI index has been validated for adults and children older than 1 year of age. In this study we aimed to study the value of IPI monitoring during pediatric endoscopic procedures. Our data consisted of 124 measurements of 109 patients undergoing different procedures (upper endoscopy 84 patients, colonoscopy 6 patients, both 9 patients). The data was divided into 3 groups based on the drug type used: propofol only, 5 patients (group 1); propofol & midazolam, 89 patients (group 2); propofol, midazolam and Fentanyl, 15 patients (group 3). Patients in group 2 and 3 had significantly higher IPI levels than group 1. Significantly lower IPI values were found between ages 4–6 compared to 7–12 years old. High midazolam dose was associated with lower IPI levels during the procedure. No significant differences were found for propofol doses. Patients who had an anesthetist present had lower IPI levels during the procedure compared to those who did not. No differences were noted between the different procedures. IPI alerted all apnea episodes (58 events, IPI = 1) and hypoxia (26 events, IPI ≤ 3) episodes, whereas pulse oximetry captured only the hypoxia episodes (IPI sensitivity = 1, specificity 0.98, positive predictive value 0.95). Younger patient age, use of propofol alone, higher midazolam doses and presence of anesthetist are all associated with lower IPI levels.



Similar content being viewed by others
References
Cohen LB, Delegge MH, Aisenberg J, Brill JV, Inadomi JM, Kochman ML, Piorkowski JD Jr. AGA Institute review of endoscopic sedation. Gastroenterology. 2007;133(2):675–701.
Radaelli F, Terruzzi V, Minoli G. Extended/advanced monitoring techniques in gastrointestinal endoscopy. Gastrointest Endosc Clin N Am. 2004;14(2):335–52.
Waring JP, Baron TH, Hirota WK, Goldstein JL, Jacobson BC, Leighton JA, Mallery JS, Faigel DO. Guidelines for conscious sedation and monitoring during gastrointestinal endoscopy. Gastrointest Endosc. 2003;58(3):317–22.
Cote CJ, Wilson S. Guidelines for monitoring and management of pediatric patients during and after sedation for diagnostic and therapeutic procedures: an update. Pediatrics. 2006;118(6):2587–602.
Lichtenstein DR, Jagannath S, Baron TH, Anderson MA, Banerjee S, Dominitz JA, Fanelli RD, Gan SI, Harrison ME, Ikenberry SO, Shen B, Stewart L, Khan K, Vargo JJ. Sedation and anesthesia in GI endoscopy. Gastrointest Endosc. 2008;68(5):815–26.
Dar AQ, Shah ZA. Anesthesia and sedation in pediatric gastrointestinal endoscopic procedures: a review. World J Gastrointest Endosc. 2010;2(7):257–62.
Koniaris LG, Wilson S, Drugas G, Simmons W. Capnographic monitoring of ventilatory status during moderate (conscious) sedation. Surg Endosc. 2003;17(8):1261–5.
Vargo JJ, Cohen LB, Rex DK, Kwo PY. Position statement: nonanesthesiologist administration of propofol for GI endoscopy. Gastroenterology. 2009;137(6):2161–7.
American Academy of Pediatrics Committee on Drugs. Guidelines for monitoring and management of pediatric patients during and after sedation for diagnostic and therapeutic procedures. Pediatrics. 1992;89(6 Pt 1):1110–5.
Beitz A, Riphaus A, Meining A, Kronshage T, Geist C, Wagenpfeil S, Weber A, Jung A, Bajbouj M, Pox C, Schneider G, Schmid RM, Wehrmann T, von DS. Capnographic monitoring reduces the incidence of arterial oxygen desaturation and hypoxemia during propofol sedation for colonoscopy: a randomized, controlled study (ColoCap Study). Am J Gastroenterol. 2012;107(8):1205–12.
Berkenbosch JW, Lam J, Burd RS, Tobias JD. Noninvasive monitoring of carbon dioxide during mechanical ventilation in older children: end-tidal versus transcutaneous techniques. Anesth Analg. 2001;92(6):1427–31.
Berkenstadt H, Ben-Menachem E, Herman A, Dach R. An evaluation of the Integrated Pulmonary Index (IPI) for the detection of respiratory events in sedated patients undergoing colonoscopy. J Clin Monit Comput. 2012;26(3):177–81.
Bhende MS. End-tidal carbon dioxide monitoring in pediatrics: concepts and technology. J Postgrad Med. 2001;47(2):153–6.
Cacho G, Perez-Calle JL, Barbado A, Lledo JL, Ojea R, Fernandez-Rodriguez CM. Capnography is superior to pulse oximetry for the detection of respiratory depression during colonoscopy. Rev Esp Enferm Dig. 2010;102(2):86–9.
Hart LS, Berns SD, Houck CS, Boenning DA. The value of end-tidal CO2 monitoring when comparing three methods of conscious sedation for children undergoing painful procedures in the emergency department. Pediatr Emerg Care. 1997;13(3):189–93.
Heuss LT, Chhajed PN, Schnieper P, Hirt T, Beglinger C. Combined pulse oximetry/cutaneous carbon dioxide tension monitoring during colonoscopies: pilot study with a smart ear clip. Digestion. 2004;70(3):152–8.
Kunkov S, Pinedo V, Silver EJ, Crain EF. Predicting the need for hospitalization in acute childhood asthma using end-tidal capnography. Pediatr Emerg Care. 2005;21(9):574–7.
Lightdale JR, Goldmann DA, Feldman HA, Newburg AR, DiNardo JA, Fox VL. Microstream capnography improves patient monitoring during moderate sedation: a randomized, controlled trial. Pediatrics. 2006;117(6):e1170–8.
McQuillen KK, Steele DW. Capnography during sedation/analgesia in the pediatric emergency department. Pediatr Emerg Care. 2000;16(6):401–4.
Nagler J, Wright RO, Krauss B. End-tidal carbon dioxide as a measure of acidosis among children with gastroenteritis. Pediatrics. 2006;118(1):260–7.
Nelson DB, Freeman ML, Silvis SE, Cass OW, Yakshe PN, Vennes J, Stahnke LL, Herman M, Hodges J. A randomized, controlled trial of transcutaneous carbon dioxide monitoring during ERCP. Gastrointest Endosc. 2000;51(3):288–95.
Sullivan KJ, Kissoon N, Goodwin SR. End-tidal carbon dioxide monitoring in pediatric emergencies. Pediatr Emerg Care. 2005;21(5):327–32.
Thakkar K, El-Serag HB, Mattek N, Gilger MA. Complications of pediatric EGD: a 4-year experience in PEDS-CORI. Gastrointest Endosc. 2007;65(2):213–21.
Tirosh E, Bilker A, Bader D, Cohen A. Capnography in spontaneously breathing preterm and term infants. Clin Physiol. 2001;21(2):150–4.
Tobias JD, Meyer DJ. Noninvasive monitoring of carbon dioxide during respiratory failure in toddlers and infants: end-tidal versus transcutaneous carbon dioxide. Anesth Analg. 1997;85(1):55–8.
Waugh JB, Epps CA, Khodneva YA. Capnography enhances surveillance of respiratory events during procedural sedation: a meta-analysis. J Clin Anesth. 2011.
Wilson J, Russo P, Russo J, Tobias JD. Noninvasive monitoring of carbon dioxide in infants and children with congenital heart disease: end-tidal versus transcutaneous techniques. J Intensive Care Med. 2005;20(5):291–5.
Yarchi D, Cohen A, Umansky T, Sukhotnik I, Shaoul R. Assessment of end-tidal carbon dioxide during pediatric and adult sedation for endoscopic procedures. Gastrointest Endosc. 2009;69(4):877–82.
Yldzdas D, Yapcoglu H, Ylmaz HL. The value of capnography during sedation or sedation/analgesia in pediatric minor procedures. Pediatr Emerg Care. 2004;20(3):162–5.
Gozal Y, Gozal D. The Integrated Pulmonary Index: validity and application in the pediatric population. 2009.
Gozal Y, Gozal D. Reliability of the Integrated Pulmonary Index Postoperatively. 2009.
Lightdale J, Fredette M, Atmadja M, Heard L, Jiang H. Pilot Study of the Smart Capnography Integrated Pulmonary IndexTM in a pediatric gastroenterology procedure unit. Gastrointest Endosc. 2010;71(5):AB255.
Sabbatani P, Mantovan R. Electrical cardioversion of atrial fibrillation: evaluation of sedation safety with midazolam by means of EtCO(2) and IPI algorithm analysis. Int J Cardiol. 2013;169(6):430–2.
Rusconi F, Castagneto M, Gagliardi L, Leo G, Pellegatta A, Porta N, Razon S, Braga M. Reference values for respiratory rate in the first 3 years of life. Pediatrics. 1994;94(3):350–5.
Wallis LA, Healy M, Undy MB, Maconochie I. Age related reference ranges for respiration rate and heart rate from 4 to 16 years. Arch Dis Child. 2005;90(11):1117–21.
National Institutes of Health Consensus Development Conference on Infantile Apnea and Home Monitoring, Sept 29 to Oct 1, 1986. Pediatrics 1987;79(2):292–9.
Cote CJ, Wilson S. Guidelines for monitoring and management of pediatric patients during and after sedation for diagnostic and therapeutic procedures: an update. Paediatr Anaesth. 2008;18(1):9–10.
Vargo JJ, Zuccaro G Jr, Dumot JA, Conwell DL, Morrow JB, Shay SS. Automated graphic assessment of respiratory activity is superior to pulse oximetry and visual assessment for the detection of early respiratory depression during therapeutic upper endoscopy. Gastrointest Endosc. 2002;55(7):826–31.
Elitsur Y, Blankenship P, Lawrence Z. Propofol sedation for endoscopic procedures in children. Endoscopy. 2000;32(10):788–91.
VanNatta ME, Rex DK. Propofol alone titrated to deep sedation versus propofol in combination with opioids and/or benzodiazepines and titrated to moderate sedation for colonoscopy. Am J Gastroenterol. 2006;101(10):2209–17.
Acknowledgments
Funding for this study was available from a research grant from Oridion.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Garah, J., Adiv, O.E., Rosen, I. et al. The value of Integrated Pulmonary Index (IPI) monitoring during endoscopies in children. J Clin Monit Comput 29, 773–778 (2015). https://doi.org/10.1007/s10877-015-9665-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-015-9665-z