Abstract
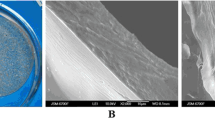
A novel bilayer knitted fabric-reinforced composite for potentially being used as a dural substitute was developed by solution infiltration of oxidized regenerated cellulose knitted fabric (ORC) with poly ε-caprolactone (PCL) solution at various concentrations ranging 10–40 g/100 mL. It was found that the density of all formulations did not differ significantly and was lower than that of the human dura. Microstructure of the samples typically comprised a bilayer structure having a nonporous PCL layer on one side and the ORC/PCL composite layer on another side. Tensile modulus and strength of the samples initially decreased with increasing PCL solution concentration for up to 20 g/100 mL and re-increased again with further increasing PCL solution concentration. Strain at break of all formulations were not significantly different. Watertight test revealed that all composites could prevent leakage at the pressure within the normal range of intracranial pressure. In vitro degradation study revealed that the weight loss percentage and change in tensile properties of all samples displayed biphasic profile comprising an initially rapid decrease and followed by a gradual decrease with incubation times afterward. Micro and macro porous channels were observed to be in situ generated in the composite layer by ORC dissolution and PCL resorption during degradation while nonporous layer remained relatively unchanged. The degradation rate was found to decrease with increasing PCL solution concentration. In vitro biocompatibility using alamar blue assay on selected samples showed that fibroblasts could attach and proliferate well at all incubation periods.











Similar content being viewed by others
References
Malliti M, Page P, Gury C, Chomette E, Nataf F, Roux FX. Comparison of deep wound infection rates using a synthetic dural substitute (neuro-patch) or pericranium graft for dural closure: a clinical review of 1 year. Neurosurgery. 2004;54:599–603.
Della Pepa GM, Montano N, Lucantoni C, Alexandre AM, Papacci F, Meglio M. Craniotomy repair with the retrosigmoid approach: the impact on quality of life of meticulous reconstruction of anatomical layers. Acta Neurochir (Wien). 2011;153:2255–8.
Sekhar LN, Mai JC. Dural Repair after craniotomy and the use of dural substitutes and dural Sealants. World Neurosurg. 2013;79:440–2.
Yamada K, Miyamoto S, Nagata I, Kikuchi H, Ikada Y, Iwata H, Yamamoto K. Development of a dural substitute from synthetic bioabsorbable polymers. J Neurosurg. 1997;86:1012–7.
Parlato C, di Nuzzo G, Luongo M, Parlato RS, Accardo M, Cuccurullo L, Moraci A. Use of a collagen biomatrix (TissuDura) for dura repair: a long-term neuroradiological and neuropathological evaluation. Acta Neurochir. 2011;153:142–7.
Tanaka S, Fukushima M. Size of Creutzfeldt-Jakob disease epidemic associated with cadaveric dura transplantation. Neuroepidemiology. 2010;34:232–7.
Ishida C, Okino S, Kitamoto T, Yamada M. Involvement of the peripheral nervous system in human prion diseases including dural graft associated Creutzfeldt-Jakob disease. J Neurol Neurosurg Psychiatry. 2005;76:325–9.
Berjano R, Vinas FC, Dujovny M. A review of dural substitutes used in neurosurgery. Crit Rev Neurosurg. 1999;9:217–22.
Hida K, Yamaguchi S, Seki T, Yano S, Akino M, Terasaka S, Uchida T, Iwasaki Y. Nonsuture dural repair using polyglycolic acid mesh and fibrin glue: clinical application to spinal surgery. Surg Neuro. 2006;65:136–43.
Kim DW, Eum WS, Jang SH, Park J, Heo DH, Sheen SH, Lee HR, Kweon H, Kang SW, Lee KG, Cho SY, Jin HJ, Cho YJ, Choi SY. A transparent artificial dura mater made of silk fibroin as an inhibitor of inflammation in craniotomized rats. J Neurosurg. 2011;114:485–90.
Suzuki Y, Iwaki M, Tani S, Oohashi G, Kamio M. Ion implantation into ePTFE for application of a dural substitute. Nucl Instr Meth Phys Res B. 2003;206:538–42.
Gonzalez-Lopez P, Harput MV, Türe H, Atalay B, Türe U. Efficacy of placing a thin layer of gelatin sponge over the subdural space during dural closure in preventing meningo-cerebral adhesion. World Neurosurg. 2015;83:93–101.
Sanchez JHS, Zuniga RR, de Anda SL, Dellamary FL, Castaneda RG, Jaimes JDCR, Espinoza GJ. A new bilayer chitosan scaffolding as a dural substitute: experimental evaluation. World Neurosurg. 2012;77:577–82.
Tsunoda M, Ikeuchi R, Tsuji M, Inoue Y, Ito K, Katagiri H, Akita H, Saji M, Yuba T, Yamada T, Tsuchiya T, Aizawa Y. Evaluation of neurotoxicity of artificial dura mater and dura mater containing a high concentration of dibutyltin in rats after intracranial implantation. Kitasato Med J. 2012;42:67–75.
Islam S, Ogane K, Ohkuma H, Suzuki S. Usefulness of acellular dermal graft as a dural substitute in experimental model. Surg Neurol. 2004;61:297–303.
Esposito F, Cappabianca P, Fusco M, Cavallo LM, Bani GG, Biroli F, Sparano A, de Divitiis O, Signorelli A. Collagen-only biomatrix as a novel dural substitute. Examination of the efficacy, safety and outcome: clinical experience on a series of 208 patients. Clin Neurol Neurosurg. 2008;110:343–51.
Siccardi D, Ventimiglia A. Fibrotic-haemorrhagic reaction to synthetic dural substitute. Acta Neurochir. 1995;132:148–9.
Costa BS, Cavalcanti-Mendes GA, Abreu MS, Sousa AA. Clinical experience with a novel bovine collagen dura mater substitute. Arq Neuropsiquiatr. 2011;69:217–20.
Knopp U, Christmann F, Reusche E, Sepehrnia A. A new collagen biomatrix of equine origin versus a cadaveric dura graft for the repair of dural defects-a comparative animal experimental study. Acta Neurochir. 2005;147:877–87.
Haq I, Cruz-Almeida Y, Siqueira EB, Norenberg M, Green BA, Levi AD. Postoperative fibrosis after surgical treatment of the porcine spinal cord: a comparison of dural substitutes. J Neurosurg Spine. 2005;2:50–4.
Woodruff MA, Hutmacher DW. The return of a forgotten polymer-Polycaprolactone in the 21st century. Prog Polym Sci. 2010;35:1217–56.
Lowry KJ, Hamson KR, Bear L, Peng YB, Celaluce R, Evans ML, Anglen OJ, Allen WC. Polycaprolactone/glass bioabsorbable implant in a rabbit humerus fracture model. J Biomed Mater Res. 1997;36:536–41.
Sung HJ, Meredith C, Johnson C, Galis ZS. The effect of scaffold degradation rate on three-dimensional cell growth and angiogenesis. Biomaterials. 2004;25:5735–42.
Shih TY, Yang JD, Chen JH. Synthesis, characterization and evaluation of segmented polycaprolactone for development of dura substitute. Procedia Eng. 2012;36:144–9.
Wang H, Dong H, Kang CG, Lin C, Ye X, Zhao YL. Preliminary exploration of the development of a collagenous artificial dura mater for sustained antibiotic release. Chin Med J (Engl). 2013;126:3329–33.
van Noort R, Black MM, Martin TRP, Meanley S. A study of the uniaxial mechanical properties of human dura mater preserved in glycerol. Biomaterials. 1981;2:41–5.
Leong KH, Ramakrishna S, Huang ZM, Bibo GA. The potential of knitting for engineering composites—a review. Compos A. 2000;31:197–220.
Neulen A, Gutenberg A, Takacs I, Weber G, Wegmann J, Schaeffer WS, Giese A. Evaluation of efficacy and biocompatibility of a novel semisynthetic collagen matrix as a dural onlay graft in a large animal model. Acta Neurochir. 2011;153:2241–50.
Hong JK, Madihally SV. 3D scaffold of electrosprayed fibers with large pore size for tissue regeneration. Acta Biomater. 2010;6:4734–42.
van Noort R, Martin TRP, Black MM, Barker AT, Montero CG. The mechanical properties of human dura mater and the effects of storage media. Clin Phys Physiol Meas. 1981;2:197–203.
Zarzur E. Mechanical properties of the human lumbar dura mater. Arq Neuropsiquiatr. 1996;54:455–60.
Duhovic M, Bhattacharyya D. Simulating the deformation mechanisms of knitted fabric composites. Compos A. 2006;37:1897–915.
Huysmans G, Verpoest I, Houtte PV. A damage model for knitted fabric composites. Compos A. 2001;32:1465–75.
Bini TB, Ramakrishna S, Huang ZM, Lim CT. Structure–tensile property relationship of knitted fabric composites. Polym Compos. 2001;22:11–21.
Lim CT, Ramakrishna S, Ong LB, Huang ZM. Investigating the effects of anisotropy of knitted fabric reinforced polymer (KFRP) composite. J Reinf Plast Compos. 2001;20:685–96.
Andresen M, Juhler M. Intracranial pressure following complete removal of a small demarcated brain tumor: a model for normal intracranial pressure in humans. J Neurosurg. 2014;121:797–801.
Luciano RM, Zavaglia CAC, Duek EAR, Alberto-Rincon MC. Synthesis and characterization of poly(L-lactic acid) membranes: studies in vitro and in vivo. J Mater Sci: Mater Med. 2003;14:87–94.
Middleton JC, Tipton AJ. Synthetic biodegradable polymers as orthopaedic devices. Biomaterials. 2000;21:2335–46.
Pena J, Corrales T, Izquierdo-Barba I, Doadrio AL, Vallet-Regi M. Long term degradation of poly(ε-caprolactone) films in biologically related fluids. Polym Degrad Stab. 2006;91:1424–32.
von Burkersroda F, Schedl L, Göpferich A. Why degradable polymers undergo surface erosion or bulk erosion. Biomaterials. 2002;23:4221–31.
Salgado CL, Sanchez EMS, Zavaglia CAC, Granja PL. Biocompatibility and biodegradation of polycaprolactone-sebacic acid blended gels. J Biomed Mater Res A. 2012;100A:243–51.
Zhou F, Chen G, Zhang JM, Huang ZS. An in vitro culturing model for rabbit dural cells. Ann Clin Lab Sci Summer. 2006;36:341–4.
Hwang CM, Sant S, Masaeli M, Kachouie NN, Zamanian B, Lee SH, Khademhosseini A. Fabrication of three-dimensional porous cell-laden hydrogel for tissue engineering. Biofabrication. 2010;2:035003.
Liu H, Raghavan D, Melaku S, Stubbs J. Biological response of osteoblast-like UMR-106 cells to the modified PHBV matrix–effects of porosity and collagen dip coating. J Biomed Mater Res A. 2010;92:922–30.
Acknowledgments
Collaborative research project grant from the Faculty of Science and the Faculty of Medicine Ramathibodi Hospital, Mahidol University (2013–2015) was acknowledged for financially supporting this study. The authors would also like to thank W. Chokvivat for the help in cell culture experiment and National Metal and Materials Technology Center for the use of characterization instruments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Suwanprateeb, J., Luangwattanawilai, T., Theeranattapong, T. et al. Bilayer oxidized regenerated cellulose/poly ε-caprolactone knitted fabric-reinforced composite for use as an artificial dural substitute. J Mater Sci: Mater Med 27, 122 (2016). https://doi.org/10.1007/s10856-016-5736-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-016-5736-z