Abstract
Hydrogels are polymeric networks with tridimensional structure, which are able to load water and other substances. Such property makes hydrogels suitable for innumerous applications in biomedical field. Hydrogels are being used as raw materials in pharmaceutical formulations for more than 60 years, while significant progress is very well documented in topical use. Natural and synthetic polymers have been applied to develop smart hydrogels that respond to physiological stimuli to follow the release of the loaded bioactive ingredient. This paper discusses the most relevant polymers commonly used in pharmaceutical formulations for modified topical delivery.
Similar content being viewed by others
Introduction
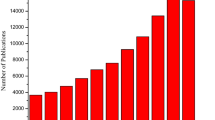
For almost 60 years, hydrogels have been explored in medical and pharmaceutical fields [1]. Their first successful synthesis was performed by Wichterle and Lim, when they developed soft hydrogel contact lenses [2]. Since then, a wide range of applications have emerged in researches worldwide [3].
Back in the 1970s, Nalbandian and coworkers developed a hydrogel made of Pluronic 127 carried with silver nitrate in order to threat thermal burns [4]. In the following decade, hydrogels were applied to encapsulate pancreas islets in alginate membranes [5] and in an association between collagen and shark cartilage for wound dressing [6].
From the 1990s to the present, extensive research brought the most important advances for hydrogels. Copolymers consisting of poly(ethylene oxide) (PEO) and poly(L-lactic acid) (PLLA) were synthesized, designed mainly for delivery of protein, in order to facilitate the loading of hydrophobic drugs [7]. Hyaluronic acid was used to develop a system to release GH and investigate the hydrogel’s potential for drug delivery [8].
The discovered possibility of hydrogels to release hydrophobic drugs opened new possibilities for the delivery of innumerous substances and therapeutics that once found difficulties in reaching the objective needed [9]. Following that, the progress of hydrogel science has led to the increased interest in the so-called smart hydrogels. Basically, they consist in polymeric matrixes with tunable properties and trigger stimuli [10].
Such characteristics point to the advantage of hydrogels in drug delivery, being that they make possible to tune mechanisms such as diffusion and swelling and to program responses to environmental stimuli [11]. In that sense, hydrogels have also shown the ability to carry proteins and peptides [12] and deliver drugs with the need of action improvement or targeting [11].
In the past three decades, it was possible to comprehend the importance of hydrogels in drug delivery: They can facilitate and sustain the release of biologically active agents. Such applicability contributes to the decreasing number of administrations, prevention of damage and successful dosage of drugs [3].
For that matter, it is important to highlight the versatility of hydrogels in different routes of administration [11], especially for transdermal and topical delivery. As pointed by Saha and coworkers, being the skin the largest human organ, with more surface area, drug administration passing through it has drawn much more attention than any other drug delivery system [13]. At the same time, topical and dermatological administration face limitation from the drugs applied, such as poor adherence skin, poor permeability and difficulties in the cooperation by patients [14].
In order to overcome such occurrences and improve treatments and therapies, hydrogels have been used as a viable alternative. Saha and coworkers, for example, were able to enhance the permeability and penetrability of the drugs tested by delivering them transdermally using pluronic lecithin organogels. With this approach, the levels of absorption by the systemic circulation could be enhanced [13].
On the other hand, studies have been performed in the attempt to use films to deliver drugs, both topical and transdermal, in order to improve their action both at the body tissue and systematically [14]. As for disorders occasioned to the skin, such as dermatitis and topical wounds, the use of hydrogels presents as an alternative to overcome problems in the currently used dressings [15].
Wound management is especially difficult since it involves a dynamic and complex process. To reach an ideal healing, treatment of choice must provide maintenance of high humidity at the wound site, removal of excess exudate, protection from infections and contaminants, the ability to be removed without causing further trauma, the allowance of gaseous exchange, comfortability and not frequent dressing change [11]. As pointed by Harrison and Spada, and by Aderibigbe and Buyana [11, 15], hydrogels have shown their importance more recently in wound treatment, mostly due to their fitting to the properties of an ideal dressing. More than that, hydrogels can enhance healing, as they are also able to deliver antibiotics and other needed substances.
Due to the shown properties and unique characteristics, hydrogels can be notably chosen for topical use as they exhibit many benefits over other commonly used drug delivery vehicles, while stepping toward innovative treatments. Recently, some authors have also published reviews considering the need to develop more assertive systems to wound dressing, healing and drug delivery. In the same knowledge field, our review paper aims to discuss commonly used polymers for modified topical delivery.
Hydrogels characteristics
Hydrogels are tridimensional polymeric networks able to absorb a considerable amount of water. Their main characteristic of hydrogels is associated with the presence of hydrophilic and hydrophobic groups in the polymeric chain [16]. The balance between these groups makes water absorption possible at levels from 10 to 99% [17]. At the same time, cross-links have to be present to avoid dissolution in aqueous environment [18].
Cross-links are responsible for connecting the networks, which determine whether the polymeric chain shows viscous-elastic or elastic behavior [18]. The volume of water absorbed by a hydrogel is limited by the elasticity of the polymeric networks, which defines its swelling capacity [19]. When swollen, the hydrogel absorbs such amount of water that the mass of liquid present in its polymeric networks becomes greater than the mass of the polymer that composes it [17].
For clinical use, hydrogels are recommended to be biodegradable, and for that, unstable bonds are frequently introduced into the hydrogel structure. These bonds can either be present in the polymer backbone or in the cross-links used to prepare the hydrogel. The bonds can be broken under physiological conditions, either enzymatically or chemically. A great variety of methods to establish cross-linking have therefore been used in hydrogel preparation [18].
For hydrogels’ synthesis, both physical and chemical methods have been applied. In physically cross-linked hydrogels, dissolution is prevented by physical interactions existing between polymeric chains [18]. Physical cross-links are based on hydrogen bonds, ionic bonds, van der Waals interactions or hydrophobic connections [20]. In chemically cross-linked hydrogels, covalent bonds are present between the polymeric chains [16]. Chemical cross-links require a mediator agent for the reaction to occur, but the formed gels offer higher mechanical stability, since covalent bonds are stronger [17].
The water content of a hydrogel determines its physical and chemical characteristics, which guarantees unique properties to this structure, with the capacity to modify the release profile of loaded drugs [21]. Compared to other classes of biomaterials, hydrogels have the advantages of offering biodegradability, biocompatibility, suitable mechanical strength and porous structure [22]. Hydrogels have also low elastic surface tension with water and other biological fluids, which makes them highly biotolerable [23].
Natural and synthetic hydrogels
Natural hydrogels are composed of biopolymers, polymers that occur in nature and are mainly biodegradable [24]. They are biodegradable and biocompatible and present low or non-toxicity [25]. Associated with that, hydrogels made of natural polymers present more similarities to the living tissue, which makes them more suitable for biomedical application [26].
Though natural hydrogels are supposedly better for medical and pharmaceutical use, most of the hydrogels currently available in the market are synthesized from synthetic polymers. This is especially due to their excellent physical, chemical and mechanical properties, which overcome the natural ones. At the same time, synthetic hydrogels present higher production cost and are not renewable and not environmental friendly [27].
Such duality of behavior presented by the types of hydrogel can point to trammels when it comes to use as the best alternative for innumerous applications. On the other hand, such implication can be exceeded by modifications in the polymeric chains of the hydrogels [23].
Several strategies have been applied to create hydrogels with defined network structures, desirable chemical compositions and tunable mechanical strength, making them suitable for different applications in topical route (Table 1). These hydrogels can be prepared from completely synthetic components and show incredible stability even under stressful environmental conditions [28]. By modifying the polymeric chains with stimuli-responsive functional groups, hydrogels can respond to different stimuli, such as heat, pH, light, chemical agents and magnetic fields [29].
At the same time, natural and synthetic polymers can have their polymeric chain blended as their important and usable characteristics are coupled. Therefore, an adjustment of the chemical and physical properties of both kinds of polymers can be reached [30].
Materials for hydrogel preparation
Alginate
Alginate is a copolymer produced by brown algae [25] and bacteria, such as Azotobacter and Pseudomonas. Structurally, alginate is composed of two uronic acids: d-mannuronic acid and l-guluronic acid. To form hydrogels of this material, it is necessary that the cross-linking reaction occurs by the substitution of sodium ions by calcium ions, as the following reaction [31]:
When the synthesis happens, during gelation, drugs and bioactives (e.g., proteins, cells and DNA) can be retained with full biological activity in the hydrogel matrix. Although loaded in the polymeric network, the bioactive is still free to diffuse within the gel network and be released in the site of action to exhibit its biological effect [31].
Alginate has been suggested for use in wound healing [32] and encapsulation of therapeutic agents [33, 34], especially because of its biocompatibility, biodegradability and facility to be obtained [35]. Hydrogels made of alginate have been considered for the treatment of several kinds of wounds, since their high water content, elasticity, permeability and ability to create a moist environment in the wound bed offer higher patients’ compliance [36].
Calcium alginate hydrogels have also been used to load poorly water-soluble drugs [37], with the aim to increase the solubility of such drugs and modify their release profile [38].
Carboxymethyl cellulose (NaCMC)
Sodium carboxymethyl cellulose (NaCMC) is a water-soluble adhesive polymer that occurs naturally [39]. Hydroxyl and carboxyl groups are present in its structure, which makes it suitable for chemical modifications [40].
NaCMC has been used as a viscosity inducer in ocular formulations, such as in eyes drops and in artificial substitutes for tears. When used alone, NaCMC forms a transparent thin film with low mechanical strength, which compromises its use as ocular biomaterial. To improve the biomechanical properties of NaCMC, the cellulose derivative can be blended with a rigid polymer as polyvinyl alcohol (PVA), while maintaining the biodegradable and bioadhesive properties of NaCMC [39].
The water absorbent properties of NaCMC are another attribute of this polymer, as its excellent skin and mucous membrane compatibility. NaCMC is able to maintain an optimal moist environment in wound region for extracellular matrix formation and re-epithelialization, being proper as a dressing for the treatment of burn wounds [41].
NaCMC can also be used as a hydrophilic polymer and a pH-responsive component to improve the swelling ratio of poly (n-isopropylacrylamide) (PNIPAAM) hydrogels. Such association can produce pH/temperature responsive hydrogels [42] that are suitable for the controlled release of drugs and bioactives [41].
Capanema et al. developed a carboxymethyl cellulose–doxorubicin (CMC-DOX) prodrug hydrogel for topical chemotherapy of melanoma skin cancer. More than analyzing that the degree of substitution of carboxymethyl cellulose in the hydrogels affects its swelling and gel fraction behavior, the study shows that CMC-DOX hydrogel has effective response toward melanoma cancer cells [43].
Chitosan
Chitosan is a semicrystalline, biocompatible and biodegradable amino polysaccharide. It is obtained from the exoskeletons of crustaceans in a process that involves demineralization, deproteinization, deacetylation of chitin, extraction of chitosan and precipitation [44, 45]. Chitosan is also non-toxic and can be used to produce gel membranes, coatings and fibers [46].
Chitosan hydrogels are also versatile, attributed to the presence of several hydroxyl groups that make the polymeric chain to swell rapidly, as it maintains its original shape. These hydrogels exhibit phase transition under environmental stimuli, e.g., pH, temperature or ionic strength [44].
Chitosan is one of the main choices for drug delivery. Its matrix has been used to encapsulate drugs and proteins [47,48,49,50,51,52,53,54], cells and growth factors, among other therapeutic agents [45], as well as to disperse nanoparticles to develop semisolid formulations [55, 56]. Chitosan hydrogels can be used in epidermal and internal implants, since they can keep the drug concentration constant for long periods of time [44].
Hydrogels based on natural polymers are often chosen for controlled release of drugs [57] and, when cross-linked with dialdehydes and dicarboxylic acids, have been described to exhibit less adverse side effects than the synthetic ones. However, there are only few in vivo tests regarding this application. In that sense, chitosan hydrogels have been prepared by cross-linking with glutaraldehyde and glutaric acid, in order to obtain compatible and biodegradable materials for topical use [44]. Synthesis of modified chitosan hydrogels to improve their adhesiveness and evaluate their suitability for topical application has been performed [58, 59].
Hydrogels can knowingly support the wound healing process, since they are able to provide moisture to the wound, preventing fluid loss [60]. Hydrogel dressings can be flexible and helpful in the epidermis repair [61]. In drug delivery, they offer higher flexibility and response to pH and temperature stimuli. Polyvinyl alcohol (PVA) and chitosan have proven excellent mechanical properties, biocompatibility and capacity to increase the collagen synthesis [62, 63].
Silver sulfadiazine (SSD) is considered as a gold standard in the treatment of burns. Commercially, silver sulfadiazine is available in a cream form, which presents many disadvantages. The formation of an adhesive eschar turns difficult to differentiate it from the burn eschar, and such occurrence prevents SSD to penetrate the wound [64]. Increased inflammation is also observed with the use of SSD as well as toxicity toward fibroblasts and keratinocytes [65].
In vitro studies evidenced SSD’s cytotoxicity, which was shown to be minimized by controlling its delivery [66]. Following that direction, an interest has been put in polymeric materials, which often offer valid scope for application in drug delivery. In view of that, chitosan/carbopol hydrogels had SSD incorporated in its matrix, in a way that enhanced burn healing while overcame the disadvantages of the current commercial formulation [65].
Cyclodextrins
Cyclodextrins are oligosaccharides that form tridimensional cyclic structures, exhibiting hydroxyl groups, which makes hydrophobic the inner compartment, while the exterior is hydrophilic. There are three forms of cyclodextrins, namely alpha-, beta- and gamma-cyclodextrins [67, 68].
The structure of cyclodextrins makes them suitable for developing hydrogels and to load drugs in their inner core. The result is the formation of noncovalent complexes with drugs, modifying their solubility, diffusivity and stability [69].
Copolymerization with cyclodextrins offers the possibility to form hydrogels with novel mechanisms of drug uptake and/or retention [70]. The obtained drug–cyclodextrin complex is dispersed within the gel network, being the drug released when in contact with the physiological fluids. However, copolymerization may significantly change physicochemical properties of the hydrogel, especially swelling and viscoelastic properties [71].
Implants based on cyclodextrin hydrogels were tested on rats and rabbits [9, 72]. The formulations were able to reduce the risk of drug loss in the tear fluid, thereby increasing its uptake from the cornea. Hydrogels may therefore be used to overcome the main problems regarding eye delivery, namely drug solubility in tear fluid and permeation through the cornea [73].
Dextran
Dextran is a polysaccharide showing biocompatibility and biodegradability, besides being non-immunogenic and non-antigenic. Such material has been widely used for several biomedical applications, such as drug delivery and tissue engineering. Scaffolds made of dextran are soft and flexible [74], which favors their handling for wound treatment, as well as for tissue re-epithelialization [75].
Dextran is soluble in water and in organic solvents, which makes it feasible for bioapplications. Because dextran can be copolymerized with other polymers, its physical and biological properties can be manipulated according to the required application [75].
Hydrogels made of dextran have been used as a platform to load drug, as well as growth factors for skin regeneration [76]. These hydrogels can also improve drug penetration in the skin and have an enhanced pharmacological effect [77].
Nanogels are hydrogels made in nanoscale. They work with the direct load of drugs, both hydrophilic and hydrophobic. Drug release kinetics can be controlled through degradation rate of cross-links or under stimuli, such as pH and temperature [78].
Nanogels based on N-isopropylacrylamide and 2-hydroxyl methacrylate-lactide-dextran macromer were successfully used for retinal drug delivery [79], being therefore a suitable alternative to eye drops [80].
Poly(ethylene glycol) (PEG)
Poly(ethylene glycol) is a polymer of ethylene oxide and can have a molecular weight lower than 100000. PEGs with molecular weights under 1000 tend to be viscous and colorless, while the ones with higher molecular weights are waxy and white. PEGs are amphiphilic and soluble in aqueous environments, as well as in organic solvents such as ethanol, acetone and chloroform [81].
Drug delivery systems of insoluble networks can be formed with PEG polymer alone; however, to reach stronger cross-links, additional groups must be added to the polymeric chain. Groups such as acrylate, amine and carboxyl can form a biomaterial with high mechanical strength and more resilient networks [82].
PEGs exhibit biocompatibility and non-immunogenicity and are approved by the Food and Drug Administration (FDA) for biomedical use. Examples include their use in tissue engineering and for wound healing [82].
PEG has been used to cover nanoparticle surfaces [83, 84], to enhance both shelf-life in vitro (steric stabilization) and half-life in vivo (stealth properties). In addition, it can provide site-specific drug release, with enhanced therapeutic activity, while limiting adverse side effects [85].
Gabriel et al. developed nanocarriers based on methoxy—poly(ethylene glycol)—hexyl-substituted poly(lactic acid) (mPEGhexPLA) containing tacrolimus (TAC) [86]. TAC is a potent immunosuppressive topic drug, approved for the treatment of dermatitis [87] and recommended for facial psoriasis [88].
Drug dosage could be reduced because of the higher site-specific delivery of TAC in the inflamed skin. The hydrogel formulation containing TAC has successfully been used to improve patients’ compliance and overcome the disadvantages encountered in the currently available formulations [86].
Poly(2-hydroxyethyl methacrylate) (PHEMA)
Poly(hydroxyethyl methacrylate) is one of the first developed synthetic polymers [89] being introduced by Wichterle and Lim in 1960 [2]. Since then, it has been applied in medical and pharmaceutical areas, especially for its non-toxicity and biocompatible properties [89].
PHEMA hydrogels have high water absorbing capacity being widely applied in drug delivery [90]. Their mechanical and swelling properties facilitate the delivery of loaded drugs. Such properties depend on the cross-linking agents used for the synthesis of the hydrogel [91]. The high water content of PHEMA hydrogels enables the uptake of drugs by the simple immersion in concentrated solution. Especially used for the development of contact lenses, PHEMA hydrogels allow the drug diffusion between the lens and the cornea, increasing the drug retention in the ocular tissues significantly, so ocular bioavailability can be enhanced considerably [92].
Wichterle and Lim were the firsts to describe a biocompatible synthetic material for contact lens applications [93, 94]. In their pioneer work, a hydrogel based on poly-2-hydroxyethylmethacrylate (PHEMA) has been developed [2], which later came to be optimized by Bausch and Lomb and then approved by the FDA in 1971 [94].
Contact lenses can be classified as hard or soft. Hard lenses are based on hydrophobic materials such as poly(methyl methacrylate) (PMMA) or poly(hexa-fluoroisopropyl methacrylate) (HFIM). Soft lenses are usually made of hydrogels [94].
Hydrogel contact lenses can be a more convenient way to transport drug through the eye. They exhibit chemical and mechanical stability, reasonable cost, high oxygen permeability and biocompatibility. Hydrogels also have the ability to control drug diffusion, being therefore highly applied for drug delivery [95].
Poly-hydroxyethylmethacrylate (PHEMA) is recognized as an effective biomaterial for the delivery of several ophthalmic drugs [96]. Ciolino, Hoare, Iwata, Behlau, Dohlman, Langer and Kohane [97] developed a prototype contact lenses by coating PLGA (poly[lactic-co-glycolic acid]) films containing test compounds with PHEMA (poly[hydroxyethyl methacrylate]) by ultraviolet light polymerization. In this study, they used fluorescein and ciprofloxacin to perform release studies and the system showed zero-order release kinetics at therapeutically relevant concentrations for 1 month, indicating that the system is suitable for ocular drug delivery. Using the same system changing the compound for econazole, an antifungal, the same group concluded that the econazole-eluting contact lenses could be used to provide extended antifungal activity for fungal ocular infections [98].
Poly(lactic-co-glycolic acid) (PLGA)
Poly(lactic-co-glycolic acid) is one of the most used polymers in biomedical applications. PLGA can be hydrolyzed into lactic acid and glycolic acid, which can be easily metabolized by the human body, via the citric acid cycle, offering a high degree of biodegradability. PLGA is approved by the FDA for use in humans, especially for drug delivery systems, e.g., nanoparticles and microparticles [84, 99,100,101,102,103,104].
The chemical degradation of PLGA is well characterized and is controllable [104, 105]. The drug release from PLGA networks can therefore be modified for site-specific delivery [106].
The physicochemical properties of PLGA are affected by factors that include polymer molecular weight, ratio of lactic to glycolic acid in the copolymers, polymer–drug ratio, preparation process and environmental conditions, such as pH and temperature [107]. These factors also affect the ability of PLGA to form nanoparticles and may control their hydrolysis and degradation. The type of drug is responsible for setting the release rate, as well as the mechanical strength and swelling behavior [108].
PLGA has been studied for controlled releases not just for topical uses but also for cancer treatment [109] and bone tissue regeneration [110]. Poly-(d,l-lactic acid-co-glycolic acid) (PLGA)–polyethylene glycol (PEG)–PLGA triblock copolymer system was used as a sustained-release system for ear drug delivery. Cidofovir was used as model drug for the release studies, showing that the hydrogel can provide sustained release and be controlled by the use of additives [111].
Poly(N-isopropylacrylamide) (PNIPAAm)
Poly(N-isopropylacrylamide) is a synthetic polymer known for its thermo-responsive behavior, since it reacts to temperature stimuli, with a defined lower critical solution temperature (LCST). LCST is a temperature in which the polymer is presented in different structures below and above it [112]. For hydrogels of PNIPAAM, the LCST is around 32°C [113].
PNIPAAm is one of the most extensively studied polymers, since it shows solubility in water at room temperature. Above the LCST, the polymeric solution transforms into an opaque gel, which is caused by hydrophobic interactions [114]. At temperatures below the LCST, hydrogen bonds are formed. When under heating, hydrophobic interactions between the polymeric chains become dominant, if the temperature is higher than the LCST [115].
The uptake and release profiles of drugs from PNIPAAm hydrogels depend on the physicochemical properties of the polymer [116]. In modified-release systems, the swelling of the polymer decreases the release of hydrophobic drugs, whereas the release of hydrophilic drugs is increased. Indeed, the water uptake by the hydrogel contributes to enhance the diffusion of water-soluble drugs within the polymeric network [117].
In attempt to overcome the semisolid limited of effectivity [118] due to short exposition of the area to the product (removal by contact, decrease of viscosity at body temperature, amongst other), in situ hydrogels formulation have gained attention [119]. Thermosensitive hydrogels as polyethylene glycol (PEG)–poly(N-isopropylacrylamide) (PNIPAAm), chitosan/poly(vinyl alcohol), show phase transition in face of temperature alterations. For vaginal administration, for instance, such formulations can be easily applied at room temperature, since they present low viscosity, which allow quickly spreading and flow into the vagina’s mucosa. Besides that, hydrogels can prologue residence of the loaded drug in the vagina [120].
Polyvinyl alcohol (PVA)
Polyvinyl alcohol is synthetic polymer known for its biodegradable and biocompatible properties [121]. Considered one of the oldest materials for hydrogels synthesis, PVA has been used for several biomedical applications, e.g., wound management, drug delivery systems and contact lenses [60].
Despite the wide use of PVA in semisolid formulations, hydrogels based on this polymer have insufficient elasticity and very limited hydrophilic characteristics. As for wound dressing, PVA hydrogels usually have to be blended with other polymers, either natural or synthetic [122], which may change the capacity of the polymer for swelling and its contribution for wound moisture [60]. Chemical modifications, e.g., cross-linking with other polymers, are therefore necessary to develop drug delivery systems with the required biomechanical properties (i.e. flexibility, adhesiveness and permeability) for wound applications [123].
Treatment for severe wounds generally requires drug administration at time intervals for long periods. The use of modified release systems has been proposed as an approach to reduce dosing frequency while keeping the drug released for longer periods of time for a prolonged therapy [124]. The development of a controlled release system by formulating simvastatin in a polyvinyl alcohol (PVA) hydrogel has been useful for wound healing, attributed to the prolonged release of the drug from the hydrogel while reducing dosing frequency [125].
Scleroglucan
Scleroglucan (SCLG) is a natural polysaccharide produced by Sclerotium fungi. Its structure offers interesting properties for the development of topical hydrogels [126]. SCLG is basically composed of a linear backbone of (1,3)-linked d-glucopyranosyl residues bearing a single (1,6)-linked d-glucopyranosyl unit every three sugar residues of the main chain [127]. In aqueous medium, SCLG shows triple helix conformation and pseudo-plastic behavior, which exhibits its transition from sol to gel status [128, 129].
SCLG can be applied in the preparation of modified-release dosage forms for topical drug delivery and may be altered with pH-responsive groups, which have considerable effect on the characteristics of the polymer [130, 131]. For instance, a carboxymethyl derivative of scleroglucan (SCLG-CM) is obtained by the reaction with chloroacetic acid in basic medium, which influences the gel properties. This modification makes SCLG-CM capable of forming hydrogels without the addition of any salt [132].
Paolicelli, Varani, Pacelli, Ogliani, Nardoni, Petralito, Adrover and Casadei [126] recently used three different compounds (fluconazole, diclofenac sodium salt and betamethasone phosphate sodium salt) to perform release studies with the carboxymethyl scleroglucan hydrogel, besides the rheological characterization. Depending on the compound, the mechanical properties slightly changed. Betamethasone made the hydrogel weaker; on the other side, diclofenac made the hydrogel stronger by interacting the carboxylic group with Scl-CM300. This interaction also slowed its release, making this hydrogel useful for a sustained topical release of diclofenac.
Stimuli-responsive hydrogels
Stimuli-responsive hydrogels are polymer networks developed to change in the presence of a stimuli, modifying its form or/and releasing its content. The stimuli for drug release may be physical, chemical or biochemical, causing degradation of the hydrogel itself or the release of the drug by scissile bonds [133]. This stimulus can be both endogenous, inherent to biochemical changes caused by pathology (pH, reactive oxygen species, temperature), and exogenous, from external manipulation (heat, light, ultrasound) [134, 135]. This diversity of stimuli for drug release can be explored and the response of the hydrogels to them can be tuned, leading to a control release and targeted drug delivery, protecting and stabilizing its content until release is triggered [133, 136].
A well-known smart polymer is the Poloxamer 407. P407 is a triblock structure formed by a hydrophobic group, propylene oxide (PO), and a hydrophilic group, ethylene oxide (EO), on the ends EO-PO-EO, and is a reverse thermal gelation polymer. This transition between liquid to gel form is due to the aggregation of copolymer molecules in micelles. When the hydrophobic PO block dehydrates, it forms the core of the micelle leaving the EO as an outer shell, hydrated, to swollen [137]. Yang, Sabharwal, Okonkwo, Shlykova, Tong, Lin, Wang, Guo, Rosowski, Pelton and Kohane [138] developed a hydrogel for otitis media treatment, using P407 due to thermal gelation properties, adding polybutylphosphoester (PBP) to both ends (EO) to maintain the mechanical strength of the hydrogel, forming a pentablock, PBP-EO-PO-EO-PBP. Applying to the tympanic membrane (TM), hydrogel turns into gel by meeting a higher temperature and adhere to TM during required time for disease treatment.
Using alginate and synthetic compounds 2-hydroxyethyl acrylate (HEA) and poly(ethylene glycol) diacrylate (PEGDA), Das, Pham, Lee and Noh [139] synthesized a terpolymeric semi-interpenetrating (semi-IPN) hydrogel using graft polymerization and cross-linking processes by free radical polymerization technique. They tested hydrogels in two different pHs, 2.5 and 7.4, and results show that when the hydrogel is at a lower pH (pH 2.5) it has less void space due to protonation, and the intramolecular H-bonding made the polymer network more rigid.
LeValley, Tibbitt, Noren, Kharkar, Kloxin, Anseth, Toner and Oakey [140] developed a photodegradable functionalized poly(ethylene glycol) to capture and release circulating tumor cells. Linking a photodegradable molecule, o-nitrobenzyl monomer, to PEG’s amino-end, the hydrogel would degrade in the presence of 365 nm light, releasing captured cells in a high-resolution controlled manner.
Future perspectives and conclusions
Programmable hydrogels represent great advance in the area since their development requires control not only when the drug or protein release starts but also when it finishes. For these hydrogels, different from what happens to the stimuli-responsive ones, internal and external factors must be considered (Table 2). Functional structures and properties of the polymers used have to go through alterations in order to develop a programmable hydrogel [141].
While hydrogels have been extensively study for a long time now, room still exists for novel, chemically modified polymers for a range of new applications in drug delivery. For topical use, many studies are promising, but standard applications and treatments are still preferred. Attributed to their biodegradability, biocompatibility and suitable biomechanical properties, one of the most promising uses of hydrogels is for wounds treatment and management. Chemically different hydrogels can be tailored to exhibit the required physicochemical properties for a set of drugs. Recently, we have modified the functionality of PNIPAAm hydrogels to incorporate and release bromelain, a set of proteolytic enzymes with anti-inflammatory and healing properties [142, 143]. New polymers with innumerous characteristics arise frequently, and for such, new techniques and developments must be performed in order to create new and alternative applications and treatments.
References
Dadsetan M, Liu Z, Pumberger M et al (2010) A stimuli-responsive hydrogel for doxorubicin delivery. Biomaterials 31:8051–8062. https://doi.org/10.1016/j.biomaterials.2010.06.054
Wichterle O, LÍM D (1960) Hydrophilic gels for biological use. Nature 185:117–118. https://doi.org/10.1038/185117a0
Buwalda SJ, Boere KW, Dijkstra PJ, Feijen J, Vermonden T, Hennink WE (2014) Hydrogels in a historical perspective: from simple networks to smart materials. J Control Release Off J Control Release Soc 190:254–273. https://doi.org/10.1016/j.jconrel.2014.03.052
Nalbandian RM, Henry RL, Wilks HS (1972) Artificial skin. II. Pluronic F-127 silver nitrate or silver lactate gel in the treatment of thermal burns. J Biomed Mater Res 6:583–590. https://doi.org/10.1002/jbm.820060610
Lim F, Sun AM (1980) Microencapsulated islets as bioartificial endocrine pancreas. Science 210:908–910
Yannas IV, Lee E, Orgill D, Skrabut EM, Murphy GF (1989) Synthesis and characterization of a model extracellular matrix that induces partial regeneration of adult mammalian skin. Proc Natl Acad Sci 86(3):933–937
Jeong B, Bae YH, Lee DS, Kim SW (1997) Biodegradable block copolymers as injectable drug-delivery systems. Nature 388:860. https://doi.org/10.1038/42218
Cascone MG, Sim B, Sandra D (1995) Blends of synthetic and natural polymers as drug delivery systems for growth hormone. Biomaterials 16:569–574. https://doi.org/10.1016/0142-9612(95)91131-H
Davis BM, Normando EM, Guo L et al (2014) Topical delivery of Avastin to the posterior segment of the eye in vivo using annexin A5-associated liposomes. Small 10:1575–1584. https://doi.org/10.1002/smll.201303433
Yahia LH, Chirani N, Gritsch L et al (2015) History and applications of hydrogels. J Biomedical Sci 4:2. https://doi.org/10.4172/2254-609X.100013
Harrison IP, Spada F (2018) Hydrogels for atopic dermatitis and wound management: a superior drug delivery vehicle. Pharmaceutics 10:71. https://doi.org/10.3390/pharmaceutics10020071
Ashley GW, Henise J, Reid R, Santi DV (2013) Hydrogel drug delivery system with predictable and tunable drug release and degradation rates. Proc Natl Acad Sci U S A 110:2318–2323. https://doi.org/10.1073/pnas.1215498110
Saha S, Shivarajakumar R, Karri VVSR (2018) Pluronic lecithin organogels: an effective topical and transdermal drug delivery system. Int J Pharm Sci Res 11:4540–4550. https://doi.org/10.13040/ijpsr.0975-8232.9
Kathe K, Kathpalia H (2017) Film forming systems for topical and transdermal drug delivery. Asian J Pharm Sci 12:487–497. https://doi.org/10.1016/j.ajps.2017.07.004
Aderibigbe BA, Buyana B (2018) Alginate in wound dressings. Pharmaceutics 10:42. https://doi.org/10.3390/pharmaceutics10020042
Samchenko Y, Ulberg Z, Korotych O (2011) Multipurpose smart hydrogel systems. Adv Colloid Interface Sci 168:247–262. https://doi.org/10.1016/j.cis.2011.06.005
Deligkaris K, Tadele TS, Olthuis W, van den Berg A (2010) Hydrogel-based devices for biomedical applications. Sens Actuators B Chem 147:765–774. https://doi.org/10.1016/j.snb.2010.03.083
Hennink WE, van Nostrum CF (2012) Novel crosslinking methods to design hydrogels. Adv Drug Deliv Rev 64:223–236. https://doi.org/10.1016/j.addr.2012.09.009
da Silva R, Ganzarolli de Oliveira M (2007) Effect of the cross-linking degree on the morphology of poly(NIPAAm-co-AAc) hydrogels. Polymer 48:4114–4122. https://doi.org/10.1016/j.polymer.2007.05.010
Ahmed EM (2015) Hydrogel: preparation, characterization, and applications: a review. J Adv Res 6:105–121. https://doi.org/10.1016/j.jare.2013.07.006
Tatiana A, Joana FF, Sajan J, Antonello S, Amelia MS, Eliana BS (2015) Hydrophilic polymers for modified-release nanoparticles: a review of mathematical modelling for pharmacokinetic analysis. Curr Pharm Des 21:3090–3096. https://doi.org/10.2174/1381612821666150531163617
Chai Q, Jiao Y, Yu X (2017) Hydrogels for biomedical applications: their characteristics and the mechanisms behind them. Gels 3:6
Hamidi M, Azadi A, Rafiei P (2008) Hydrogel nanoparticles in drug delivery. Adv Drug Deliv Rev 60:1638–1649. https://doi.org/10.1016/j.addr.2008.08.002
Martínez-Ruvalcaba A, Chornet E, Rodrigue D (2007) Viscoelastic properties of dispersed chitosan/xanthan hydrogels. Carbohydr Polym 67:586–595. https://doi.org/10.1016/j.carbpol.2006.06.033
Gyles DA, Castro LD, Silva JOC, Ribeiro-Costa RM (2017) A review of the designs and prominent biomedical advances of natural and synthetic hydrogel formulations. Eur Polym J 88:373–392. https://doi.org/10.1016/j.eurpolymj.2017.01.027
Tanan W, Panichpakdee J, Saengsuwan S (2019) Novel biodegradable hydrogel based on natural polymers: synthesis, characterization, swelling/reswelling and biodegradability. Eur Polym J 112:678–687. https://doi.org/10.1016/j.eurpolymj.2018.10.033
Xu X, Bai B, Ding C, Wang H, Suo Y (2015) Synthesis and properties of an ecofriendly superabsorbent composite by grafting the poly(acrylic acid) onto the surface of dopamine-coated sea buckthorn branches. Ind Eng Chem Res 54:3268–3278. https://doi.org/10.1021/acs.iecr.5b00092
Pan G, Guo Q, Ma Y, Yang H, Li B (2013) Thermo-responsive hydrogel layers imprinted with RGDS peptide: a system for harvesting cell sheets. Angew Chem (Int Ed Engl) 52:6907–6911. https://doi.org/10.1002/anie.201300733
Koetting MC, Guido JF, Gupta M, Zhang A, Peppas NA (2016) pH-responsive and enzymatically-responsive hydrogel microparticles for the oral delivery of therapeutic proteins: effects of protein size, crosslinking density, and hydrogel degradation on protein delivery. J Control Release 221:18–25. https://doi.org/10.1016/j.jconrel.2015.11.023
Sionkowska A, Skopinska-Wisniewska J, Planecka A, Kozlowska J (2010) The influence of UV irradiation on the properties of chitosan films containing keratin. Polym Degrad Stab 95:2486–2491. https://doi.org/10.1016/j.polymdegradstab.2010.08.002
Ciofani G, Raffa V, Pizzorusso T, Menciassi A, Dario P (2008) Characterization of an alginate-based drug delivery system for neurological applications. Med Eng Phys 30:848–855. https://doi.org/10.1016/j.medengphy.2007.10.003
Ataide JA, Cefali LC, Croisfelt FM, Zanchetta B, Souto EB, Nascimento LO, Mazzola PG (2018) Wound healing process and synthetic actives: a review. Skin Pharmacol Physiol 97(8):2892–2923
Horiguchi I, Sakai Y (2015) Alginate Encapsulation of Pluripotent Stem Cells Using a Co-axial Nozzle. J Vis Exp JoVE 101:e52835–e52835. https://doi.org/10.3791/52835
Severino P, Chaud MV, Shimojo A et al (2015) Sodium alginate-cross-linked polymyxin B sulphate-loaded solid lipid nanoparticles: antibiotic resistance tests and HaCat and NIH/3T3 cell viability studies. Colloids Surf B 129:191–197. https://doi.org/10.1016/j.colsurfb.2015.03.049
Li Y, Rodrigues J, Tomas H (2012) Injectable and biodegradable hydrogels: gelation, biodegradation and biomedical applications. Chem Soc Rev 41:2193–2221. https://doi.org/10.1039/c1cs15203c
Chiu CT, Lee JS, Chu CS, Chang YP, Wang YJ (2008) Development of two alginate-based wound dressings. J Mater Sci: Mater Med 19:2503. https://doi.org/10.1007/s10856-008-3389-2
Colinet I, Dulong V, Mocanu G, Picton L, Le Cerf D (2009) New amphiphilic and pH-sensitive hydrogel for controlled release of a model poorly water-soluble drug. Eur J Pharm Biopharm 73:345–350. https://doi.org/10.1016/j.ejpb.2009.07.008
Josef E, Zilberman M, Bianco-Peled H (2010) Composite alginate hydrogels: an innovative approach for the controlled release of hydrophobic drugs. Acta Biomater 6:4642–4649. https://doi.org/10.1016/j.actbio.2010.06.032
Jain D, Carvalho E, Banerjee R (2010) Biodegradable hybrid polymeric membranes for ocular drug delivery. Acta Biomater 6:1370–1379. https://doi.org/10.1016/j.actbio.2009.11.001
El-Hag Ali A, Abd El-Rehim HA, Kamal H, Hegazy DESA (2008) Synthesis of carboxymethyl cellulose based drug carrier hydrogel using ionizing radiation for possible use as site specific delivery system. J Macromol Sci Part A 45:628–634. https://doi.org/10.1080/10601320802168751
Namazi H, Rakhshaei R, Hamishehkar H, Kafil HS (2016) Antibiotic loaded carboxymethylcellulose/MCM-41 nanocomposite hydrogel films as potential wound dressing. Int J Biol Macromol 85:327–334. https://doi.org/10.1016/j.ijbiomac.2015.12.076
Ma J, Xu Y, Fan B, Liang B (2007) Preparation and characterization of sodium carboxymethylcellulose/poly(N-isopropylacrylamide)/clay semi-IPN nanocomposite hydrogels. Eur Polym J 43:2221–2228. https://doi.org/10.1016/j.eurpolymj.2007.02.026
Capanema NSV, Mansur AAP, Carvalho SM et al (2018) Bioengineered carboxymethyl cellulose-doxorubicin prodrug hydrogels for topical chemotherapy of melanoma skin cancer. Carbohydr Polym 195:401–412. https://doi.org/10.1016/j.carbpol.2018.04.105
Muñoz G, Valencia C, Valderruten N, Ruiz-Durántez E, Zuluaga F (2015) Extraction of chitosan from Aspergillus niger mycelium and synthesis of hydrogels for controlled release of betahistine. React Funct Polym 91–92:1–10. https://doi.org/10.1016/j.reactfunctpolym.2015.03.008
Solé I, Vílchez S, Miras J, Montanyà N, García-Celma MJ, Esquena J (2017) DHA and l-carnitine loaded chitosan hydrogels as delivery systems for topical applications. Colloids Surf A 525:85–92. https://doi.org/10.1016/j.colsurfa.2017.04.056
Dash M, Chiellini F, Ottenbrite RM, Chiellini E (2011) Chitosan—A versatile semi-synthetic polymer in biomedical applications. Prog Polym Sci 36:981–1014. https://doi.org/10.1016/j.progpolymsci.2011.02.001
Jose S, Prema MT, Chacko AJ, Thomas AC, Souto EB (2011) Colon specific chitosan microspheres for chronotherapy of chronic stable angina. Colloids Surf B 83:277–283. https://doi.org/10.1016/j.colsurfb.2010.11.033
Jose S, Fangueiro JF, Smitha J et al (2012) Cross-linked chitosan microspheres for oral delivery of insulin: taguchi design and in vivo testing. Colloids Surf B 92:175–179. https://doi.org/10.1016/j.colsurfb.2011.11.040
Severino P, de Oliveira GGG, Ferraz HG, Souto EB, Santana MHA (2012) Preparation of gastro-resistant pellets containing chitosan microspheres for improvement of oral didanosine bioavailability. J Pharm Anal 2:188–192. https://doi.org/10.1016/j.jpha.2012.02.005
Jose S, Fangueiro JF, Smitha J et al (2013) Predictive modeling of insulin release profile from cross-linked chitosan microspheres. Eur J Med Chem 60:249–253. https://doi.org/10.1016/j.ejmech.2012.12.011
Severino P, Da Silva CF, Dalla Costa TCT et al (2014) In vivo absorption of didanosine formulated in pellets composed of chitosan microspheres. Vivo 28:1045–1050
Severino P, da Silva CF, da Silva MA, Santana MHA, Souto EB (2016) Chitosan cross-linked pentasodium tripolyphosphate micro/nanoparticles produced by ionotropic gelation. Sugar Tech 18:49–54. https://doi.org/10.1007/s12355-014-0360-z
Ferreira C, da Silva P, Severino F Martins, Santana MHA, Souto EB (2015) Didanosine-loaded chitosan microspheres optimized by surface-response methodology: a modified “maximum likelihood classification” approach formulation for reverse transcriptase inhibitors. Biomed Pharmacother 70:46–52. https://doi.org/10.1016/j.biopha.2014.12.047
Severino P, Silva H, Souto EB, Santana MHA, Dalla Costa TCT (2012) Analysis of in vivo absorption of didanosine tablets in male adult dogs by HPLC. J Pharm Anal 2:29–34. https://doi.org/10.1016/j.jpha.2011.10.006
Cardoso AM, de Oliveira EG, Coradini K et al (2019) Chitosan hydrogels containing nanoencapsulated phenytoin for cutaneous use: skin permeation/penetration and efficacy in wound healing. Mater Sci Eng C 96:205–217. https://doi.org/10.1016/j.msec.2018.11.013
Souto EB, Wissing SA, Barbosa CM, Müller RH (2004) Evaluation of the physical stability of SLN and NLC before and after incorporation into hydrogel formulations. Eur J Pharm Biopharm 58:83–90. https://doi.org/10.1016/j.ejpb.2004.02.015
Fan Q, Ma J, Xu Q et al (2015) Animal-derived natural products review: focus on novel modifications and applications. Colloids Surf B 128:181–190. https://doi.org/10.1016/j.colsurfb.2015.02.033
Laffleur F (2017) Evaluation of chemical modified hydrogel formulation for topical suitability. Int J Biol Macromol. https://doi.org/10.1016/j.ijbiomac.2017.07.152
Barbosa GP, Debone HS, Severino P, Souto EB, da Silva CF (2016) Design and characterization of chitosan/zeolite composite films—Effect of zeolite type and zeolite dose on the film properties. Mater Sci Eng C 60:246–254. https://doi.org/10.1016/j.msec.2015.11.034
Kamoun EA, Chen X, Mohy Eldin MS, Kenawy E-RS (2015) Crosslinked poly(vinyl alcohol) hydrogels for wound dressing applications: a review of remarkably blended polymers. Arabian J Chem 8:1–14. https://doi.org/10.1016/j.arabjc.2014.07.005
Madaghiele M, Demitri C, Sannino A, Ambrosio L (2014) Polymeric hydrogels for burn wound care: advanced skin wound dressings and regenerative templates. Burns Trauma 2:153–161. https://doi.org/10.4103/2321-3868.143616
Ribeiro MP, Espiga A, Silva D, Baptista P, Henriques J, Ferreira C (2009) Development of a new chitosan hydrogel for wound dressing. Wound Repair Regen 17:817–824. https://doi.org/10.1111/j.1524-475x.2009.00538.x
Jaiswal M, Gupta A, Agrawal AK, Jassal M, Dinda AK, Koul V (2013) Bi-layer composite dressing of gelatin nanofibrous mat and poly vinyl alcohol hydrogel for drug delivery and wound healing application: in-vitro and in-vivo studies. J Biomed Nanotechnol 9:1495–1508. https://doi.org/10.1166/jbn.2013.1643
Atiyeh BS, Costagliola M, Hayek SN, Dibo SA (2007) Effect of silver on burn wound infection control and healing: review of the literature. Burns J Int Soc Burn Inj 33:139–148. https://doi.org/10.1016/j.burns.2006.06.010
Morsi NM, Abdelbary GA, Ahmed MA (2014) Silver sulfadiazine based cubosome hydrogels for topical treatment of burns: development and in vitro/in vivo characterization. Eur J Pharm Biopharm 86:178–189. https://doi.org/10.1016/j.ejpb.2013.04.018
Jodar KSP, Balcao VM, Chaud MV et al (2015) Development and characterization of a hydrogel containing silver sulfadiazine for antimicrobial topical applications. J Pharm Sci 104:2241–2254. https://doi.org/10.1002/jps.24475
de Paula E, Cereda CM, Tofoli GR, Franz-Montan M, Fraceto LF, de Araujo DR (2010) Drug delivery systems for local anesthetics. Recent Pat Drug Deliv Formul 4:23–34
Teixeira RS, Veiga FJB, Oliveira RS et al (2014) Effect of cyclodextrins and pH on the permeation of tetracaine: supramolecular assemblies and release behavior. Int J Pharm 466:349–358. https://doi.org/10.1016/j.ijpharm.2014.03.035
Sun Y, Du L, Liu Y et al (2014) Transdermal delivery of the in situ hydrogels of curcumin and its inclusion complexes of hydroxypropyl-β-cyclodextrin for melanoma treatment. Int J Pharm 469:31–39. https://doi.org/10.1016/j.ijpharm.2014.04.039
Thatiparti TR, von Recum HA (2010) Cyclodextrin complexation for affinity-based antibiotic delivery. Macromol Biosci 10:82–90. https://doi.org/10.1002/mabi.200900204
dos Santos JF, Alvarez-Lorenzo C, Silva M et al (2009) Soft contact lenses functionalized with pendant cyclodextrins for controlled drug delivery. Biomaterials 30:1348–1355. https://doi.org/10.1016/j.biomaterials.2008.11.016
Vaishya RD, Khurana V, Patel S, Mitra AK (2014) Controlled ocular drug delivery with nanomicelles Wiley interdisciplinary reviews. Nanomed Nanobiotechnol 6:422–437. https://doi.org/10.1002/wnan.1272
Loftsson T, Stefánsson E (2017) Cyclodextrins and topical drug delivery to the anterior and posterior segments of the eye. Int J Pharm 531:413–423. https://doi.org/10.1016/j.ijpharm.2017.04.010
Sun G, Zhang X, Shen YI, Sebastian R, Dickinson LE, Fox-Talbot K (2011) Dextran hydrogel scaffolds enhance angiogenic responses and promote complete skin regeneration during burn wound healing. Proc Natl Acad Sci USA. https://doi.org/10.1073/pnas.1115973108
Unnithan AR, Sasikala ARK, Murugesan P et al (2015) Electrospun polyurethane-dextran nanofiber mats loaded with Estradiol for post-menopausal wound dressing. Int J Biol Macromol 77:1–8. https://doi.org/10.1016/j.ijbiomac.2015.02.044
Ribeiro MP, Morgado PI, Miguel SP, Coutinho P, Correia IJ (2013) Dextran-based hydrogel containing chitosan microparticles loaded with growth factors to be used in wound healing. Mater Sci Eng C Mater Biol Appl. https://doi.org/10.1016/j.msec.2013.03.025
Cassano R, Trombino S, Muzzalupo R, Tavano L, Picci N (2009) A novel dextran hydrogel linking trans-ferulic acid for the stabilization and transdermal delivery of vitamin E. Eur J Pharm Biopharm 72:232–238. https://doi.org/10.1016/j.ejpb.2008.10.003
Kompella UB, Amrite AC, Pacha Ravi R, Durazo SA (2013) Nanomedicines for back of the eye drug delivery, gene delivery, and imaging. Prog Retin Eye Res 36:172–198. https://doi.org/10.1016/j.preteyeres.2013.04.001
Fomina N, McFearin C, Sermsakdi M, Edigin O, Almutairi A (2010) UV and near-IR triggered release from polymeric nanoparticles. J Am Chem Soc 132:9540–9542. https://doi.org/10.1021/ja102595j
Campos EJ, Campos A, Martins J, Ambrósio AF (2017) Opening eyes to nanomedicine: where we are, challenges and expectations on nanotherapy for diabetic retinopathy. Nanomed Nanotechnol Biol Med 13:2101–2113. https://doi.org/10.1016/j.nano.2017.04.008
Akhtar MF, Hanif M, Ranjha NM (2016) Methods of synthesis of hydrogels—a review. Saudi Pharm J 24:554–559. https://doi.org/10.1016/j.jsps.2015.03.022
Yu J, Xu X, Yao F et al (2014) In situ covalently cross-linked PEG hydrogel for ocular drug delivery applications. Int J Pharm 470:151–157. https://doi.org/10.1016/j.ijpharm.2014.04.053
Andreani T, Souza ALRD, Kiill CP et al (2014) Preparation and characterization of PEG-coated silica nanoparticles for oral insulin delivery. Int J Pharm 473:627–635. https://doi.org/10.1016/j.ijpharm.2014.07.049
Sánchez-López E, Egea MA, Cano A et al (2016) PEGylated PLGA nanospheres optimized by design of experiments for ocular administration of dexibuprofen—in vitro, ex vivo and in vivo characterization. Colloids Surf B 145:241–250. https://doi.org/10.1016/j.colsurfb.2016.04.054
Lin CC, Anseth KS (2009) PEG hydrogels for the controlled release of biomolecules in regenerative medicine. Pharm Res 26:631–643. https://doi.org/10.1007/s11095-008-9801-2
Gabriel D, Mugnier T, Courthion H et al (2016) Improved topical delivery of tacrolimus: a novel composite hydrogel formulation for the treatment of psoriasis. J Control Release 242:16–24. https://doi.org/10.1016/j.jconrel.2016.09.007
Rallis E, Korfitis C, Gregoriou S, Rigopoulos D (2007) Assigning new roles to topical tacrolimus. Expert Opin Investig Drugs 16:1267–1276. https://doi.org/10.1517/13543784.16.8.1267
Korman N, Menter A, Elmets CA, Feldman SR, Gelfand JM, Gordon KB et al (2009) Guidelines of care for the management of psoriasis and psoriatic arthritis. Guidelines of care for the management and treatment of psoriasis with topical therapies. J Am Acad Dermatol 60(4):643–659. https://doi.org/10.1016/j.jaad.2008.12.032
Mabilleau G, Aguado E, Stancu IC, Cincu C, Baslé MF, Chappard D (2008) Effects of FGF-2 release from a hydrogel polymer on bone mass and microarchitecture. Biomaterials 29:1593–1600. https://doi.org/10.1016/j.biomaterials.2007.12.018
Zeng N, Dumortier G, Maury M, Mignet N, Boudy V (2014) Influence of additives on a thermosensitive hydrogel for buccal delivery of salbutamol: relation between micellization, gelation, mechanic and release properties. Int J Pharm 467:70–83. https://doi.org/10.1016/j.ijpharm.2014.03.055
Sivashanmugam A, Arun Kumar R, Vishnu Priya M, Nair SV, Jayakumar R (2015) An overview of injectable polymeric hydrogels for tissue engineering. Eur Polymer J 72:543–565. https://doi.org/10.1016/j.eurpolymj.2015.05.014
dos Santos JF, Couceiro R, Concheiro A, Torres-Labandeira JJ, Alvarez-Lorenzo C (2008) Poly(hydroxyethyl methacrylate-co-methacrylated-beta-cyclodextrin) hydrogels: synthesis, cytocompatibility, mechanical properties and drug loading/release properties. Acta Biomater 4:745–755. https://doi.org/10.1016/j.actbio.2007.12.008
Venkatesh S, Sizemore SP, Byrne ME (2007) Biomimetic hydrogels for enhanced loading and extended release of ocular therapeutics. Biomaterials 28:717–724. https://doi.org/10.1016/j.biomaterials.2006.09.007
Caló E, Khutoryanskiy VV (2015) Biomedical applications of hydrogels: a review of patents and commercial products. Eur Polymer J 65:252–267. https://doi.org/10.1016/j.eurpolymj.2014.11.024
Ali M, Horikawa S, Venkatesh S, Saha J, Hong JW, Byrne ME (2007) Zero-order therapeutic release from imprinted hydrogel contact lenses within in vitro physiological ocular tear flow. J Control Release 124:154–162. https://doi.org/10.1016/j.jconrel.2007.09.006
Xinming L, Yingde C, Lloyd AW et al (2008) Polymeric hydrogels for novel contact lens-based ophthalmic drug delivery systems: a review. Contact Lens Anterior Eye 31:57–64. https://doi.org/10.1016/j.clae.2007.09.002
Ciolino JB, Hoare TR, Iwata NG et al (2009) A drug-eluting contact lens. Invest Ophthalmol Vis Sci 50:3346–3352. https://doi.org/10.1167/iovs.08-2826
Ciolino JB, Hudson SP, Mobbs AN et al (2011) A prototype antifungal contact lens. Invest Ophthalmol Vis Sci 52:6286–6291. https://doi.org/10.1167/iovs.10-6935
Araújo J, Vega E, Lopes C, Egea MA, Garcia ML, Souto EB (2009) Effect of polymer viscosity on physicochemical properties and ocular tolerance of FB-loaded PLGA nanospheres. Colloids Surf B 72:48–56. https://doi.org/10.1016/j.colsurfb.2009.03.028
Jose S, Sowmya S, Cinu TA, Aleykutty NA, Thomas S, Souto EB (2014) Surface modified PLGA nanoparticles for brain targeting of Bacoside-A. Eur J Pharm Sci 63:29–35. https://doi.org/10.1016/j.ejps.2014.06.024
Abrego G, Alvarado H, Souto EB et al (2015) Biopharmaceutical profile of pranoprofen-loaded PLGA nanoparticles containing hydrogels for ocular administration. Eur J Pharm Biopharm 95:261–270. https://doi.org/10.1016/j.ejpb.2015.01.026
Cañadas C, Alvarado H, Calpena AC et al (2016) In vitro, ex vivo and in vivo characterization of PLGA nanoparticles loading pranoprofen for ocular administration. Int J Pharm 511:719–727. https://doi.org/10.1016/j.ijpharm.2016.07.055
Sánchez-López E, Ettcheto M, Egea MA et al (2018) Memantine loaded PLGA PEGylated nanoparticles for Alzheimer’s disease: in vitro and in vivo characterization. J Nanobiotechnol 16:32. https://doi.org/10.1186/s12951-018-0356-z
Schoubben A, Blasi P, Deluca PP (2012) Effect of agitation regimen on the in vitro release of leuprolide from poly(lactic-co-glycolic) acid microparticles. J Pharm Sci 101:1212–1220. https://doi.org/10.1002/jps.23029
Abrego G, Alvarado H, Souto EB et al (2016) Biopharmaceutical profile of hydrogels containing pranoprofen-loaded PLGA nanoparticles for skin administration: in vitro, ex vivo and in vivo characterization. Int J Pharm 501:350–361. https://doi.org/10.1016/j.ijpharm.2016.01.071
Vega E, Egea MA, Garduno-Ramirez ML et al (2013) Flurbiprofen PLGA-PEG nanospheres: role of hydroxy-beta-cyclodextrin on ex vivo human skin permeation and in vivo topical anti-inflammatory efficacy. Colloids Surf B Biointerfaces 110:339–346. https://doi.org/10.1016/j.colsurfb.2013.04.045
Terukina T, Naito Y, Tagami T et al (2016) The effect of the release behavior of simvastatin from different PLGA particles on bone regeneration in vitro and in vivo: comparison of simvastatin-loaded PLGA microspheres and nanospheres. J Drug Deliv Sci Technol 33:136–142. https://doi.org/10.1016/j.jddst.2016.03.005
Makadia HK, Siegel SJ (2011) Poly lactic-co-glycolic acid (plga) as biodegradable controlled drug delivery carrier. Polymers 3:1377–1397. https://doi.org/10.3390/polym3031377
Gao Y, Ren F, Ding B et al (2011) A thermo-sensitive PLGA-PEG-PLGA hydrogel for sustained release of docetaxel. J Drug Target 19:516–527. https://doi.org/10.3109/1061186X.2010.519031
Yan Q, Xiao L-Q, Tan L et al (2015) Controlled release of simvastatin-loaded thermo-sensitive PLGA-PEG-PLGA hydrogel for bone tissue regeneration: in vitro and in vivo characteristics. J Biomed Mater Res Part A 103:3580–3589. https://doi.org/10.1002/jbm.a.35499
Liang F, Jonette AW, Li SK, Gaurav T, Jinsong H, Daniel IC (2014) Assessment of PLGA-PEG-PLGA copolymer hydrogel for sustained drug delivery in the ear. Curr Drug Deliv 11:279–286. https://doi.org/10.2174/1567201811666140118224616
Chen Y-S, Tsou P-C, Lo J-M, Tsai H-C, Wang Y-Z, Hsiue G-H (2013) Poly(N-isopropylacrylamide) hydrogels with interpenetrating multiwalled carbon nanotubes for cell sheet engineering. Biomaterials 34:7328–7334. https://doi.org/10.1016/j.biomaterials.2013.06.017
Alexander A, Ajazuddin J Khan, Saraf S, Saraf S (2014) Polyethylene glycol (PEG)–Poly(N-isopropylacrylamide) (PNIPAAm) based thermosensitive injectable hydrogels for biomedical applications. Eur J Pharm Biopharm 88:575–585. https://doi.org/10.1016/j.ejpb.2014.07.005
Kulkarni RV, Mangond BS, Mutalik S, Sa B (2011) Interpenetrating polymer network microcapsules of gellan gum and egg albumin entrapped with diltiazem–resin complex for controlled release application. Carbohydr Polym 83:1001–1007. https://doi.org/10.1016/j.carbpol.2010.09.017
Y-t Kim J-M, Caldwell RV Bellamkonda (2009) Nanoparticle-mediated local delivery of methylprednisolone after spinal cord injury. Biomaterials 30:2582–2590. https://doi.org/10.1016/j.biomaterials.2008.12.077
García-Uriostegui L, Burillo G, Bucio E (2012) Synthesis and characterization of thermosensitive interpenetrating polymer networks based on N-isopropylacrylamide/N-acryloxysuccinimide, crosslinked with polylysine, grafted onto polypropylene. Radiat Phys Chem 81:295–300. https://doi.org/10.1016/j.radphyschem.2011.11.053
de Sousa A, Maria DA, de Sousa RG, de Sousa EMB (2010) Synthesis and characterization of mesoporous silica/poly(N-isopropylacrylamide) functional hybrid useful for drug delivery. J Mater Sci 45:1478–1486. https://doi.org/10.1007/s10853-009-4106-3
D’Cruz OJ, Uckun FM (2014) Vaginal microbicides and their delivery platforms. Expert Opin Drug Deliv 11:723–740. https://doi.org/10.1517/17425247.2014.888055
Li C, Han C, Zhu Y, Lu W, Li Q, Liu Y (2014) In vivo evaluation of an in-situ hydrogel system for vaginal administration. Pharmazie 69:458–460
Priya James H, John R, Alex A, Anoop KR (2014) Smart polymers for the controlled delivery of drugs – a concise overview. Acta Pharm Sin B 4:120–127. https://doi.org/10.1016/j.apsb.2014.02.005
Jiang S, Liu S, Feng W (2011) PVA hydrogel properties for biomedical application. J Mech Behav Biomed Mater 4:1228–1233. https://doi.org/10.1016/j.jmbbm.2011.04.005
Coviello T, Matricardi P, Marianecci C, Alhaique F (2007) Polysaccharide hydrogels for modified release formulations. J Control Release 119:5–24. https://doi.org/10.1016/j.jconrel.2007.01.004
Singh B, Pal L (2012) Sterculia crosslinked PVA and PVA-poly(AAm) hydrogel wound dressings for slow drug delivery: mechanical, mucoadhesive, biocompatible and permeability properties. J Mech Behav Biomed Mater 9:9–21. https://doi.org/10.1016/j.jmbbm.2012.01.021
Lipsky BA, Hoey C (2009) Topical antimicrobial therapy for treating chronic wounds. Clin Infect Dis Off Publ Infect Dis Soc Am 49:1541–1549. https://doi.org/10.1086/644732
Yasasvini S, Anusa RS, VedhaHari BN, Prabhu PC, RamyaDevi D (2017) Topical hydrogel matrix loaded with Simvastatin microparticles for enhanced wound healing activity. Mater Sci Eng C 72:160–167. https://doi.org/10.1016/j.msec.2016.11.038
Paolicelli P, Varani G, Pacelli S et al (2017) Design and characterization of a biocompatible physical hydrogel based on scleroglucan for topical drug delivery. Carbohydr Polym 174:960–969. https://doi.org/10.1016/j.carbpol.2017.07.008
Lapasin R, Abrami M, Grassi M, Šebenik U (2017) Rheology of laponite-scleroglucan hydrogels. Carbohydr Polym 168:290–300. https://doi.org/10.1016/j.carbpol.2017.03.068
Grassi M, Lapasin R, Coviello T, Matricardi P, Di Meo C, Alhaique F (2009) Scleroglucan/borax/drug hydrogels: structure characterisation by means of rheological and diffusion experiments. Carbohydr Polym 78:377–383. https://doi.org/10.1016/j.carbpol.2009.04.025
Viñarta SC, Delgado OD, Figueroa LIC, Fariña JI (2013) Effects of thermal, alkaline and ultrasonic treatments on scleroglucan stability and flow behavior. Carbohydr Polym 94:496–504. https://doi.org/10.1016/j.carbpol.2013.01.063
Cerreto A, Corrente F, Botta B et al (2013) NMR characterization of carboxymethyl scleroglucan. Int J Polym Anal Charact 18:587–595. https://doi.org/10.1080/1023666X.2013.842286
Corrente F, Matricardi P, Paolicelli P, Tita B, Vitali F, Casadei MA (2009) Physical carboxymethylscleroglucan/calciumion hydrogels as modified drug delivery systems in topical formulations. Molecules 14:2684–2698. https://doi.org/10.3390/molecules14082684
Corrente F, Paolicelli P, Matricardi P, Tita B, Vitali F, Casadei MA (2012) Novel pH-sensitive physical hydrogels of carboxymethyl scleroglucan. J Pharm Sci 101:256–267. https://doi.org/10.1002/jps.22766
Ruskowitz ER, Comerford MP, Badeau BA, DeForest CA (2019) Logical stimuli-triggered delivery of small molecules from hydrogel biomaterials. Biomater Sci 7:542–546. https://doi.org/10.1039/C8BM01304G
Li X, Su X (2018) Multifunctional smart hydrogels: potential in tissue engineering and cancer therapy. J Mater Chem B 6:4714–4730. https://doi.org/10.1039/C8TB01078A
Sood N, Bhardwaj A, Mehta S, Mehta A (2016) Stimuli-responsive hydrogels in drug delivery and tissue engineering. Drug Deliv 23:748–770. https://doi.org/10.3109/10717544.2014.940091
Zhao H, Xu K, Zhu P, Wang C, Chi Q (2019) Smart hydrogels with high tunability of stiffness as a biomimetic cell carrier. Cell Biol Int 43:84–97. https://doi.org/10.1002/cbin.11091
Giuliano E, Paolino D, Fresta M, Cosco D (2018) Mucosal applications of poloxamer 407-based hydrogels: an overview. Pharmaceutics. https://doi.org/10.3390/pharmaceutics10030159
Yang R, Sabharwal V, Okonkwo OS et al (2016) Treatment of otitis media by transtympanic delivery of antibiotics. Sci Transl Med 8:356ra120. https://doi.org/10.1126/scitranslmed.aaf4363
Das D, Pham HTT, Lee S, Noh I (2019) Fabrication of alginate-based stimuli-responsive, non-cytotoxic, terpolymeric semi-IPN hydrogel as a carrier for controlled release of bovine albumin serum and 5-amino salicylic acid. Mater Sci Eng C 98:42–53. https://doi.org/10.1016/j.msec.2018.12.127
LeValley PJ, Tibbitt MW, Noren B et al (2019) Immunofunctional photodegradable poly(ethylene glycol) hydrogel surfaces for the capture and release of rare cells. Colloids Surf B 174:483–492. https://doi.org/10.1016/j.colsurfb.2018.11.049
Wang Y (2018) Programmable hydrogels. Biomaterials. https://doi.org/10.1016/j.biomaterials.2018.03.008
Croisfelt F, Martins BC, Rescolino R et al (2015) Poly(N-Isopropylacrylamide)-co-acrylamide hydrogels for the controlled release of bromelain from agroindustrial residues of Ananas comosus. Planta Med. https://doi.org/10.1055/s-0035-1557867
Croisfelt FM, Ataide JA, Tundisi LL et al (2018) Characterization of PNIPAAm-co-AAm hydrogels for modified release of bromelain. Eur Polym J 105:48–54. https://doi.org/10.1016/j.eurpolymj.2018.05.016
Ishii Y, Nakae T, Sakamoto F et al (2008) A transcutaneous vaccination system using a hydrogel patch for viral and bacterial infection. J Control Release 131:113–120. https://doi.org/10.1016/j.jconrel.2008.07.025
Chen C-C, Fang C-L, Al-Suwayeh SA, Leu Y-L, Fang J-Y (2011) Transdermal delivery of selegiline from alginate–pluronic composite thermogels. Int J Pharm 415:119–128. https://doi.org/10.1016/j.ijpharm.2011.05.060
Szabó B, Kállai N, Tóth G, Hetényi G, Zelkó R (2014) Drug release profiles and microstructural characterization of cast and freeze dried vitamin B12 buccal films by positron annihilation lifetime spectroscopy. J Pharm Biomed Anal 89:83–87. https://doi.org/10.1016/j.jpba.2013.10.031
Shiohira H, Fujii M, Koizumi N, Kondoh M, Watanabe Y (2009) Novel chronotherapeutic rectal aminophylline delivery system for therapy of asthma. Int J Pharm 379:119–124. https://doi.org/10.1016/j.ijpharm.2009.06.017
Rezvanian M, Ahmad N, Mohd Amin MCI, Ng S-F (2017) Optimization, characterization, and in vitro assessment of alginate-pectin ionic cross-linked hydrogel film for wound dressing applications. Int J Biol Macromol 97:131–140. https://doi.org/10.1016/j.ijbiomac.2016.12.079
Fetih G (2010) Meloxicam formulations for transdermal delivery: hydrogels versus organogels. J Drug Deliv Sci Technol 20:451–456. https://doi.org/10.1016/S1773-2247(10)50078-9
Das A, Kumar A, Patil NB, Viswanathan C, Ghosh D (2015) Preparation and characterization of silver nanoparticle loaded amorphous hydrogel of carboxymethylcellulose for infected wounds. Carbohydr Polym 130:254–261. https://doi.org/10.1016/j.carbpol.2015.03.082
Meher JG, Tarai M, Yadav NP, Patnaik A, Mishra P, Yadav KS (2013) Development and characterization of cellulose–polymethacrylate mucoadhesive film for buccal delivery of carvedilol. Carbohydr Polym 96:172–180. https://doi.org/10.1016/j.carbpol.2013.03.076
Sivashankari PR, Prabaharan M (2016) Prospects of chitosan-based scaffolds for growth factor release in tissue engineering. Int J Biol Macromol 93:1382–1389. https://doi.org/10.1016/j.ijbiomac.2016.02.043
Sajomsang W, Nuchuchua O, Saesoo S et al (2013) A comparison of spacer on water-soluble cyclodextrin grafted chitosan inclusion complex as carrier of eugenol to mucosae. Carbohydr Polym 92:321–327. https://doi.org/10.1016/j.carbpol.2012.08.106
Liu L, Gao Q, Lu X, Zhou H (2016) In situ forming hydrogels based on chitosan for drug delivery and tissue regeneration. Asian J Pharm Sci 11:673–683. https://doi.org/10.1016/j.ajps.2016.07.001
Casettari L, Illum L (2014) Chitosan in nasal delivery systems for therapeutic drugs. J Control Release 190:189–200. https://doi.org/10.1016/j.jconrel.2014.05.003
Wu Y, Wu S, Hou L et al (2012) Novel thermal-sensitive hydrogel enhances both humoral and cell-mediated immune responses by intranasal vaccine delivery. Eur J Pharm Biopharm 81:486–497. https://doi.org/10.1016/j.ejpb.2012.03.021
Wu Y, Wei W, Zhou M et al (2012) Thermal-sensitive hydrogel as adjuvant-free vaccine delivery system for H5N1 intranasal immunization. Biomaterials 33:2351–2360. https://doi.org/10.1016/j.biomaterials.2011.11.068
Xu J, Tam M, Samaei S et al (2017) Mucoadhesive chitosan hydrogels as rectal drug delivery vessels to treat ulcerative colitis. Acta Biomater 48:247–257. https://doi.org/10.1016/j.actbio.2016.10.026
Zhu Y, Hoshi R, Chen S et al (2016) Sustained release of stromal cell derived factor-1 from an antioxidant thermoresponsive hydrogel enhances dermal wound healing in diabetes. J Control Release 238:114–122. https://doi.org/10.1016/j.jconrel.2016.07.043
Yar M, Shahzadi L, Mehmood A et al (2017) Deoxy-sugar releasing biodegradable hydrogels promote angiogenesis and stimulate wound healing. Mater Today Commun 13:295–305. https://doi.org/10.1016/j.mtcomm.2017.10.015
Ciobanu BC, Cadinoiu AN, Popa M, Desbrières J, Peptu CA (2014) Modulated release from liposomes entrapped in chitosan/gelatin hydrogels. Mater Sci Eng C 43:383–391. https://doi.org/10.1016/j.msec.2014.07.036
Cheng Y-H, Hung K-H, Tsai T-H et al (2014) Sustained delivery of latanoprost by thermosensitive chitosan–gelatin-based hydrogel for controlling ocular hypertension. Acta Biomater 10:4360–4366. https://doi.org/10.1016/j.actbio.2014.05.031
Tang Q, Luo C, Lu B et al (2017) Thermosensitive chitosan-based hydrogels releasing stromal cell derived factor-1 alpha recruit MSC for corneal epithelium regeneration. Acta Biomater 61:101–113. https://doi.org/10.1016/j.actbio.2017.08.001
Xu J, Strandman S, Zhu JXX, Barralet J, Cerruti M (2015) Genipin-crosslinked catechol-chitosan mucoadhesive hydrogels for buccal drug delivery. Biomaterials 37:395–404. https://doi.org/10.1016/j.biomaterials.2014.10.024
Casimiro MH, Gil MH, Leal JP (2007) Drug release assays from new chitosan/pHEMA membranes obtained by gamma irradiation. Nucl Instrum Methods Phys Res Sect B 265:406–409. https://doi.org/10.1016/j.nimb.2007.09.013
Radhakumary C, Antonty M, Sreenivasan K (2011) Drug loaded thermoresponsive and cytocompatible chitosan based hydrogel as a potential wound dressing. Carbohydr Polym 83:705–713. https://doi.org/10.1016/j.carbpol.2010.08.042
Layek B, Rahman Nirzhor SS, Rathi S, Kandimalla KK, Wiedmann TS, Prabha S (2019) Design, development, and characterization of imiquimod-loaded chitosan films for topical delivery. AAPS Pharm Sci Tech 20:58. https://doi.org/10.1208/s12249-018-1288-5
Hebeish A, Hashem M, El-Hady MMA, Sharaf S (2013) Development of CMC hydrogels loaded with silver nano-particles for medical applications. Carbohydr Polym 92:407–413. https://doi.org/10.1016/j.carbpol.2012.08.094
Lam YL, Muniyandy S, Kamaruddin H, Mansor A, Janarthanan P (2015) Radiation cross-linked carboxymethyl sago pulp hydrogels loaded with ciprofloxacin: influence of irradiation on gel fraction, entrapped drug and in vitro release. Radiat Phys Chem 106:213–222. https://doi.org/10.1016/j.radphyschem.2014.07.018
Alibolandi M, Mohammadi M, Taghdisi SM, Abnous K, Ramezani M (2017) Synthesis and preparation of biodegradable hybrid dextran hydrogel incorporated with biodegradable curcumin nanomicelles for full thickness wound healing. Int J Pharm 532:466–477. https://doi.org/10.1016/j.ijpharm.2017.09.042
Choi SG, Baek EJ, Davaa E et al (2013) Topical treatment of the buccal mucosa and wounded skin in rats with a triamcinolone acetonide-loaded hydrogel prepared using an electron beam. Int J Pharm 447:102–108. https://doi.org/10.1016/j.ijpharm.2013.02.053
Luaces-Rodríguez A, Díaz-Tomé V, González-Barcia M et al (2017) Cysteamine polysaccharide hydrogels: study of extended ocular delivery and biopermanence time by PET imaging. Int J Pharm 528:714–722. https://doi.org/10.1016/j.ijpharm.2017.06.060
Singh B, Sharma S, Dhiman A (2013) Design of antibiotic containing hydrogel wound dressings: biomedical properties and histological study of wound healing. Int J Pharm 457:82–91. https://doi.org/10.1016/j.ijpharm.2013.09.028
Fiorica C, Palumbo FS, Pitarresi G, Bongiovì F, Giammona G (2017) Hyaluronic acid and beta cyclodextrins films for the release of corneal epithelial cells and dexamethasone. Carbohydr Polym 166:281–290. https://doi.org/10.1016/j.carbpol.2017.02.071
Chandrasekar MJN, Kumar SM, Manikandan D, Nanjan MJ (2011) Isolation and evaluation of a polysaccharide from Prunus amygdalus as a carrier for transbuccosal delivery of Losartan potassium. Int J Biol Macromol 48:773–778. https://doi.org/10.1016/j.ijbiomac.2011.02.023
de Santana DCAS, Pupo TT, Sauaia MG, da Silva RS, Lopez RFV (2010) Nitric oxide photorelease from hydrogels and from skin containing a nitro-ruthenium complex. Int J Pharm 391:21–28. https://doi.org/10.1016/j.ijpharm.2010.02.010
Koop HS, de Freitas RA, de Souza MM, Savi-Jr R, Silveira JLM (2015) Topical curcumin-loaded hydrogels obtained using galactomannan from schizolobium parahybae and xanthan. Carbohydr Polym 116:229–236. https://doi.org/10.1016/j.carbpol.2014.07.043
Tan G, Yu S, Li J, Pan W (2017) Development and characterization of nanostructured lipid carriers based chitosan thermosensitive hydrogel for delivery of dexamethasone. Int J Biol Macromol 103:941–947. https://doi.org/10.1016/j.ijbiomac.2017.05.132
Hao J, Zhao J, Zhang S et al (2016) Fabrication of an ionic-sensitive in situ gel loaded with resveratrol nanosuspensions intended for direct nose-to-brain delivery. Colloids Surf B 147:376–386. https://doi.org/10.1016/j.colsurfb.2016.08.011
Ribeiro A, Veiga F, Santos D, Torres-Labandeira JJ, Concheiro A, Alvarez-Lorenzo C (2012) Hydrophilic acrylic hydrogels with built-in or pendant cyclodextrins for delivery of anti-glaucoma drugs. Carbohydr Polym 88:977–985. https://doi.org/10.1016/j.carbpol.2012.01.053
Matsuo K, Ishii Y, Quan Y-S et al (2011) Transcutaneous vaccination using a hydrogel patch induces effective immune responses to tetanus and diphtheria toxoid in hairless rat. J Control Release 149:15–20. https://doi.org/10.1016/j.jconrel.2010.05.012
Van Hove AH, Burke K, Antonienko E, Brown E, Benoit DSW (2015) Enzymatically-responsive pro-angiogenic peptide-releasing poly(ethylene glycol) hydrogels promote vascularization in vivo. J Control Release 217:191–201. https://doi.org/10.1016/j.jconrel.2015.09.005
Anumolu SS, DeSantis AS, Menjoge AR et al (2010) Doxycycline loaded poly(ethylene glycol) hydrogels for healing vesicant-induced ocular wounds. Biomaterials 31:964–974. https://doi.org/10.1016/j.biomaterials.2009.10.010
Rolim WR, Pieretti JC, Renó DLS et al (2019) Antimicrobial activity and cytotoxicity to tumor cells of nitric oxide donor and silver nanoparticles containing PVA/PEG films for topical applications. ACS Appl Mater Interfaces 11:6589–6604. https://doi.org/10.1021/acsami.8b19021
Huang J, Wang W, Yu J et al (2017) Combination of dexamethasone and Avastin® by supramolecular hydrogel attenuates the inflammatory corneal neovascularization in rat alkali burn model. Colloids Surf B 159:241–250. https://doi.org/10.1016/j.colsurfb.2017.07.057
Gong C, Wu Q, Wang Y et al (2013) A biodegradable hydrogel system containing curcumin encapsulated in micelles for cutaneous wound healing. Biomaterials 34:6377–6387. https://doi.org/10.1016/j.biomaterials.2013.05.005
García-Millán E, Koprivnik S, Otero-Espinar FJ (2015) Drug loading optimization and extended drug delivery of corticoids from pHEMA based soft contact lenses hydrogels via chemical and microstructural modifications. Int J Pharm 487:260–269. https://doi.org/10.1016/j.ijpharm.2015.04.037
García-Millán E, Quintáns-Carballo M, Otero-Espinar FJ (2017) Improved release of triamcinolone acetonide from medicated soft contact lenses loaded with drug nanosuspensions. Int J Pharm 525:226–236. https://doi.org/10.1016/j.ijpharm.2017.03.082
Kapoor Y, Dixon P, Sekar P, Chauhan A (2017) Incorporation of drug particles for extended release of cyclosporine a from poly-hydroxyethyl methacrylate hydrogels. Eur J Pharm Biopharm 120:73–79. https://doi.org/10.1016/j.ejpb.2017.08.007
Glisoni RJ, García-Fernández MJ, Pino M et al (2013) β-Cyclodextrin hydrogels for the ocular release of antibacterial thiosemicarbazones. Carbohydr Polym 93:449–457. https://doi.org/10.1016/j.carbpol.2012.12.033
dos Santos J-FR, Couceiro R, Concheiro A, Torres-Labandeira J-J, Alvarez-Lorenzo C (2008) Poly(hydroxyethyl methacrylate-co-methacrylated-β-cyclodextrin) hydrogels: synthesis, cytocompatibility, mechanical properties and drug loading/release properties. Acta Biomater 4:745–755. https://doi.org/10.1016/j.actbio.2007.12.008
Maulvi FA, Lakdawala DH, Shaikh AA et al (2016) In vitro and in vivo evaluation of novel implantation technology in hydrogel contact lenses for controlled drug delivery. J Control Release 226:47–56. https://doi.org/10.1016/j.jconrel.2016.02.012
Hsu K-H, Fentzke RC, Chauhan A (2013) Feasibility of corneal drug delivery of cysteamine using vitamin E modified silicone hydrogel contact lenses. Eur J Pharm Biopharm 85:531–540. https://doi.org/10.1016/j.ejpb.2013.04.017
Santoveña A, Monzón C, Delgado A, Evora C, Llabrés M, Fariña JB (2017) Development of a standard method for in vitro evaluation of Triamcinolone and BMP-2 diffusion mechanism from thermosensitive and biocompatible composite hyaluronic acid-pluronic hydrogels. J Drug Deliv Sci Technol 42:284–291. https://doi.org/10.1016/j.jddst.2017.04.022
Qian S, Wong YC, Zuo Z (2014) Development, characterization and application of in situ gel systems for intranasal delivery of tacrine. Int J Pharm 468:272–282. https://doi.org/10.1016/j.ijpharm.2014.04.015
Jose S, Ansa CR, Cinu TA et al (2013) Thermo-sensitive gels containing lorazepam microspheres for intranasal brain targeting. Int J Pharm 441:516–526. https://doi.org/10.1016/j.ijpharm.2012.10.049
Heilmann S, Küchler S, Wischke C, Lendlein A, Stein C, Schäfer-Korting M (2013) A thermosensitive morphine-containing hydrogel for the treatment of large-scale skin wounds. Int J Pharm 444:96–102. https://doi.org/10.1016/j.ijpharm.2013.01.027
Pitt WG, Zhao Y, Jack DR, Nelson JL, Pruitt JD (2011) In vitro release of phospholipid from a silicone hydrogel contact lens. Contact Lens Anterior Eye 34:S15. https://doi.org/10.1016/S1367-0484(11)60077-5
Xiaobo W, Luis D, Rayne F, Qiang Y, Carl L, Fabrice P (2011) Principles of inner ear sustained release following intratympanic administration. Laryngosc 121:385–391. https://doi.org/10.1002/lary.21370
Yuan Y, Cui Y, Zhang L et al (2012) Thermosensitive and mucoadhesive in situ gel based on poloxamer as new carrier for rectal administration of nimesulide. Int J Pharm 430:114–119. https://doi.org/10.1016/j.ijpharm.2012.03.054
Karavasili C, Fatouros DG (2016) Smart materials: in situ gel-forming systems for nasal delivery. Drug Discov Today 21:157–166. https://doi.org/10.1016/j.drudis.2015.10.016
Vigato AA, Querobino SM, de Faria NC et al (2019) Synthesis and characterization of nanostructured lipid-poloxamer organogels for enhanced skin local anesthesia. Eur J Pharm Sci 128:270–278. https://doi.org/10.1016/j.ejps.2018.12.009
Liu X, Gan H, Hu C et al (2019) Silver sulfadiazine nanosuspension-loaded thermosensitive hydrogel as a topical antibacterial agent. Int J Nanomed 14:12
Fu Din O, Mustapha DW Kim et al (2015) Novel dual-reverse thermosensitive solid lipid nanoparticle-loaded hydrogel for rectal administration of flurbiprofen with improved bioavailability and reduced initial burst effect. Eur J Pharm Biopharm 94:64–72. https://doi.org/10.1016/j.ejpb.2015.04.019
Zeng N, Mignet N, Dumortier G et al (2015) Poloxamer bioadhesive hydrogel for buccal drug delivery: cytotoxicity and trans-epithelial permeability evaluations using TR146 human buccal epithelial cell line. Int J Pharm 495:1028–1037. https://doi.org/10.1016/j.ijpharm.2015.09.045
Zeng N, Seguin J, Destruel P-L et al (2017) Cyanine derivative as a suitable marker for thermosensitive in situ gelling delivery systems: in vitro and in vivo validation of a sustained buccal drug delivery. Int J Pharm 534:128–135. https://doi.org/10.1016/j.ijpharm.2017.09.073
Huang W, Zhang N, Hua H et al (2016) Preparation, pharmacokinetics and pharmacodynamics of ophthalmic thermosensitive in situ hydrogel of betaxolol hydrochloride. Biomed Pharmacother 83:107–113. https://doi.org/10.1016/j.biopha.2016.06.024
Donnelly RF, Cassidy CM, Loughlin RG et al (2009) Delivery of Methylene Blue and meso-tetra (N-methyl-4-pyridyl) porphine tetra tosylate from cross-linked poly(vinyl alcohol) hydrogels: a potential means of photodynamic therapy of infected wounds. J Photochem Photobiol B 96:223–231. https://doi.org/10.1016/j.jphotobiol.2009.06.010
Zhou G, Ruhan A, Ge H et al (2014) Research on a novel poly (vinyl alcohol)/lysine/vanillin wound dressing: biocompatibility, bioactivity and antimicrobial activity. Burns 40:1668–1678. https://doi.org/10.1016/j.burns.2014.04.005
Morgado PI, Miguel SP, Correia IJ, Aguiar-Ricardo A (2017) Ibuprofen loaded PVA/chitosan membranes: a highly efficient strategy towards an improved skin wound healing. Carbohydr Polym 159:136–145. https://doi.org/10.1016/j.carbpol.2016.12.029
Gao B, Yang Q, Zhao X, Jin G, Ma Y, Xu F (2016) 4D bioprinting for biomedical applications. Trends Biotechnol 34:746–756. https://doi.org/10.1016/j.tibtech.2016.03.004
Ruskowitz ER, DeForest CA (2018) Photoresponsive biomaterials for targeted drug delivery and 4D cell culture. Nat Rev Mater 3:17087. https://doi.org/10.1038/natrevmats.2017.87
Li S, Chen N, Gaddes ER, Zhang X, Dong C, Wang Y (2015) A drosera-bioinspired hydrogel for catching and killing cancer cells. Sci Rep 5:14297. https://doi.org/10.1038/srep14297
Lai J, Li S, Shi X et al (2017) Displacement and hybridization reactions in aptamer-functionalized hydrogels for biomimetic protein release and signal transduction. Chem Sci 8:7306–7311. https://doi.org/10.1039/C7SC03023A
Acknowledgements
Authors acknowledge FAPESP (process number 2016/03444-5), CNPq and CAPES for the financial support.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Croisfelt, F.M., Tundisi, L.L., Ataide, J.A. et al. Modified-release topical hydrogels: a ten-year review. J Mater Sci 54, 10963–10983 (2019). https://doi.org/10.1007/s10853-019-03557-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10853-019-03557-x