Abstract
Background
Cardiac ablation catheters are small in diameter and pose ergonomic challenges that can affect catheter stability. Significant finger dexterity and strength are necessary to maneuver them safely. We evaluated a novel torque tool to reduce muscle activation when manipulating catheters and improve perceived workload of ablation tasks. The objective was to evaluate measurable success, user perception of workload, and muscle usage when completing a simulated ablation task with and without the use of a catheter torque tool.
Methods
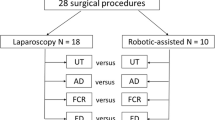
Cardiology attendings and fellows were fitted with surface electromyographic (EMG) sensors on 6 key muscle groups in the left hand and forearm. A standard ablation catheter was inserted into a pediatric cardiac ablation simulator and subjects navigated the catheter tip to 6 specific electrophysiologic targets, including a 1-min simulated radiofrequency ablation lesion. Time to complete the task, number of attempts required to complete the lesion, and EMG activity normalized to percentage of maximum voluntary contraction were collected throughout the task. The task was completed 4 times, twice with and twice without the torque tool, in semi-randomized order. A NASA Task Load Index survey was completed by the participant at the conclusion of each task.
Results
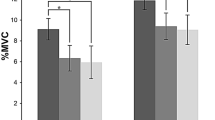
Time to complete the task and number of attempts to create a lesion were not altered by the tool. Subjectively, participants reported a significant decrease in physical demand, effort, and frustration, and a significant increase in performance. Muscle activation was decreased in 4 of 6 muscle groups.
Conclusion
The catheter torque tool may improve the perceived workload of cardiac ablation procedures and reduce muscle fatigue caused by manipulating catheters. This may result in improved catheter stability and increased procedural safety.





Similar content being viewed by others
References
Raymond-Paquin A, Andrade J, Macle L. Catheter ablation: an ongoing revolution. J Thorac Dis. 2019;11(S3):S212–5. https://doi.org/10.21037/jtd.2019.02.20.
Kugler JD, Danford DA, Houston KA, Felix G. Pediatric radiofrequency catheter ablation registry success, fluoroscopy time, and complication rate for supraventricular tachycardia: comparison of early and recent eras. J Cardiovasc Electrophysiol. 2002;13(4):336–41. https://doi.org/10.1046/j.1540-8167.2002.00336.x.
Van Hare GF, Javitz H, Carmelli D, et al. Prospective assessment after pediatric cardiac ablation: demographics, medical profiles, and initial outcomes. J Cardiovasc Electrophysiol. 2004;15(7):759–70. https://doi.org/10.1046/j.1540-8167.2004.03645.x.
Pilcher TA, Saarel EV. Anatomic challenges in pediatric catheter ablation. J Atr Fibrillation. Published online August 31, 2014. https://doi.org/10.4022/jafib.1054
Van Hare GF, Colan SD, Javitz H, et al. Prospective assessment after pediatric cardiac ablation: fate of intracardiac structure and function, as assessed by serial echocardiography. Am Heart J. 2007;153(5):815-820.e6. https://doi.org/10.1016/j.ahj.2007.02.009.
Friedman RA, Walsh EP, Silka MJ, et al. NASPE expert consensus conference: radiofrequency catheter ablation in children with and without congenital heart disease. Report of the Writing Committee. Pacing Clin Electrophysiol. 2002;25(6):1000–17. https://doi.org/10.1046/j.1460-9592.2002.01000.x.
Cappato R, Calkins H, Chen SA, et al. Updated worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circ: Arrhythmia Electrophysiol. 2010;3(1):32–8. https://doi.org/10.1161/CIRCEP.109.859116.
Bertaglia E, Zoppo F, Tondo C, et al. Early complications of pulmonary vein catheter ablation for atrial fibrillation: a multicenter prospective registry on procedural safety. Heart Rhythm. 2007;4(10):1265–71. https://doi.org/10.1016/j.hrthm.2007.06.016.
Bohnen M, Stevenson WG, Tedrow UB, et al. Incidence and predictors of major complications from contemporary catheter ablation to treat cardiac arrhythmias. Heart Rhythm. 2011;8(11):1661–6. https://doi.org/10.1016/j.hrthm.2011.05.017.
Allen DG, Lamb GD, Westerblad H. Skeletal muscle fatigue: cellular mechanisms. Physiol Rev. 2008;88(1):287–332. https://doi.org/10.1152/physrev.00015.2007.
Constantinescu MA, Lee SL, Ernst S, Hemakom A, Mandic D, Yang GZ. Probabilistic guidance for catheter tip motion in cardiac ablation procedures. Med Image Anal. 2018;47:1–14. https://doi.org/10.1016/j.media.2018.03.008.
Aizer A, Qiu JK, Cheng AV, et al. Rapid pacing and high-frequency jet ventilation additively improve catheter stability during atrial fibrillation ablation. J Cardiovasc Electrophysiol. 2020;31(7):1678–86. https://doi.org/10.1111/jce.14507.
Davis DR, Tang ASL, Gollob MH, Lemery R, Green MS, Birnie DH. Remote magnetic navigation-assisted catheter ablation enhances catheter stability and ablation success with lower catheter temperatures. Pacing Clin Electrophysiol. 2008;31(7):893–8. https://doi.org/10.1111/j.1540-8159.2008.01105.x.
Nguyen BL, Electrophysiology Section, Heart and Great Vessels Department, Umberto I Hospital, Sapienza University of Rome, Merino JL, Arrhythmia-Electrophysiology Research Unit, La Paz University Hospital, Madrid, Gang ES, Electrophysiology Section, Division of Cardiology, Cedars-Sinai Medical Center, Los Angeles, Cardiovascular Research Foundation, 414 North Camden Drive, Beverly Hills, CA 90210, US. E: gang@cvmg.com. Remote navigation for ablation procedures — a new step forward in the treatment of cardiac arrhythmias. Eur Cardiol Rev. 2010;6(3):50. https://doi.org/10.15420/ecr.2010.6.3.50
Kim AM, Turakhia M, Lu J, et al. Impact of remote magnetic catheter navigation on ablation fluoroscopy and procedure time. Pacing Clin Electrophysiol. 2008;31(11):1399–404. https://doi.org/10.1111/j.1540-8159.2008.01202.x.
Mass PN, Kumthekar RN, Berul CI, Opfermann JD. A novel tool for improved control and maneuverability in pediatric cardiac catheter ablation procedures. In: 2020 design of medical devices conference. Am Soc Mech Eng. 2020;V001T01A006. https://doi.org/10.1115/DMD2020-9039
Mass PN, Contento JM, Opfermann JD, Sumihara K, Kumthekar RN, Berul CI. An infant phantom for pediatric pericardial access and electrophysiology training. Heart Rhythm O2. Published online February 2022;S2666501822000563. https://doi.org/10.1016/j.hroo.2022.02.010
Hart SG, Staveland LE. Development of NASA-TLX (Task Load Index): results of empirical and theoretical research. In: Adv Psychol. 52. Elsevier. 1988;139–183. https://doi.org/10.1016/S0166-4115(08)62386-9
Hart SG. Nasa-Task Load Index (NASA-TLX); 20 years later. Proc Human Factors Ergon Soc Annu Meet. 2006;50(9):904–8. https://doi.org/10.1177/154193120605000909.
Ikeda A, Nakagawa H, Lambert H, et al. Relationship between catheter contact force and radiofrequency lesion size and incidence of steam pop in the beating canine heart: electrogram amplitude, impedance, and electrode temperature are poor predictors of electrode-tissue contact force and lesion size. Circ Arrhythm Electrophysiol. 2014;7(6):1174–80. https://doi.org/10.1161/CIRCEP.113.001094.
Hosseini SM, Rozen G, Saleh A, et al. Catheter ablation for cardiac arrhythmias. JACC: Clin Electrophysiol. 2017;3(11):1240–1248. https://doi.org/10.1016/j.jacep.2017.05.005
Rajappan K, Baker V, Richmond L, et al. A randomized trial to compare atrial fibrillation ablation using a steerable vs. a non-steerable sheath. Europace. 2009;11(5):571–575. https://doi.org/10.1093/europace/eup069
Acknowledgements
We would like to acknowledge the Team Trace Foundation, the Van Metre Companies Professorship, and the Children’s National Board of Visitors for financial support of our work.
Funding
This research is supported in part by the Team Trace Foundation, the Van Metre Companies Professorship, and the Children’s National Board of Visitors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Institional Review Boards at Children’s National Hospital, Nationwide Children’s Hospital, and Albert Einstein College of Medicine/Montefiore Medical Center. The studies were conducted in accordance with the Declaration of Helsinki.
Consent to participate
All participants voluntarily participated in the study after completing an informed consent document. All individuals depicted in the photographs included in this manuscript have provided informed consent of the publication of these photos.
Conflict of interest
Charles Berul, Bradley Clark, Justin Opfermann, and Paige Mass are co-inventors of the torque tool evaluated in this article.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mass, P.N., Kumthekar, R.N., Clark, B.C. et al. Muscle usage and workload assessment of cardiac ablation procedure with the use of a novel catheter torque tool in a pediatric simulator. J Interv Card Electrophysiol 65, 757–764 (2022). https://doi.org/10.1007/s10840-022-01348-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-022-01348-0