Abstract
Background
Pulmonary vein isolation (PVI) implies unavoidable ablation lesions to the left atrial posterior wall, which is closely related to the esophagus, leading to several potential complications. This study evaluates the usefulness of the esophageal fingerprint in avoiding temperature rises during paroxysmal atrial fibrillation (PAF) ablation.
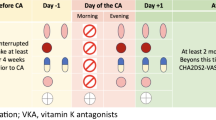
Methods
Isodistance maps of the atrio-esophageal relationship (esophageal fingerprint) were derived from the preprocedural computerized tomography. Patients were randomized (1:1) into two groups: (1) PRINT group, the PVI line was modified according to the esophageal fingerprint; (2) CONTROL group, standard PVI with operator blinded to the fingerprint. The primary endpoint was temperature rise detected by intraluminal esophageal temperature probe monitoring. Ablation settings were as specified on the Ablate BY-LAW study protocol.
Results
Sixty consecutive patients referred for paroxysmal AF ablation were randomized (42 (70%) men, mean age 60 ± 11 years). Temperature rise (> 39.1 °C) occurred in 5 (16%) patients in the PRINT group vs. 17 (56%) in the CONTROL group (p < 0.01). Three AF recurrences were documented at a mean follow-up of 12 ± 3 months (one (3%) in the PRINT group and 2 (6.6%) in the CONTROL group, p = 0.4).
Conclusion
The esophageal fingerprint allows for a reliable identification of the esophageal position and its use for PVI line deployment results in less frequent esophageal temperature rises when compared to the standard approach. Further studies are needed to evaluate the impact of PVI line modification to avoid esophageal heating on long-term outcomes. The development of new imaging-derived tools could ultimately improve patient safety (NCT04394923).
Graphical abstract







Similar content being viewed by others
Abbreviations
- AAD:
-
Antiarrhythmic drugs
- AEF:
-
Atrio-esophageal fistula
- AF:
-
Atrial fibrillation
- FAM:
-
Fast anatomical map
- LA:
-
Left atrium
- LAWT:
-
Left atrial wall thickness
- LET:
-
Luminal esophageal temperature
- MDCT:
-
Multidetector computerized tomography
- PAF:
-
Paroxysmal atrial fibrillation
- PVI:
-
Pulmonary vein isolation
- RF:
-
Radiofrequency
- TOE:
-
Transesophageal echocardiography
References
Chew DS, Jones KA, Loring Z, et al. Diagnosis-to-ablation time predicts recurrent atrial fibrillation and rehospitalization following catheter ablation. Heart Rhythm O2. 2022;3(1):23–31. https://doi.org/10.1016/j.hroo.2021.11.012.
Iwasaki Y, Nishida K, Kato T, Nattel S. Atrial fibrillation pathophysiology: implications for management. Circulation. 2011;124(20):2264–74. https://doi.org/10.1161/CIRCULATIONAHA.111.019893.
Kirchhof P, Camm AJ, Goette A, et al. Early rhythm-control therapy in patients with atrial fibrillation. N Engl J Med. 2020;383(14):1305–16. https://doi.org/10.1056/NEJMoa2019422.
Hindricks G, Potpara T, Dagres N, et al. ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACTS). Eur Heart J. August 2020. https://doi.org/10.1093/eurheartj/ehaa612
Halbfass P, Pavlov B, Muller P, et al. Progression from esophageal thermal asymptomatic lesion to perforation complicating atrial fibrillation ablation: a single-center registry. Circ Arrhythm Electrophysiol. 2017;10(8). https://doi.org/10.1161/CIRCEP.117.005233
Lakkireddy D, Reddy YM, Atkins D, et al. Effect of atrial fibrillation ablation on gastric motility: the atrial fibrillation gut study. Circ Arrhythm Electrophysiol. 2015;8(3):531–6. https://doi.org/10.1161/CIRCEP.114.002508.
Kadado AJ, Akar JG, Hummel JP. Luminal esophageal temperature monitoring to reduce esophageal thermal injury during catheter ablation for atrial fibrillation: a review. Trends Cardiovasc Med. 2019;29(5):264–71. https://doi.org/10.1016/j.tcm.2018.09.010.
Turagam MK, Miller S, Sharma SP, et al. Differences in transient thermal response of commercial esophageal temperature probes: insights from an experimental study. JACC Clin Electrophysiol. 2019;5(11):1280–8. https://doi.org/10.1016/j.jacep.2019.07.013.
Schoene K, Arya A, Grashoff F, et al. Oesophageal Probe Evaluation in Radiofrequency Ablation of Atrial Fibrillation (OPERA): results from a prospective randomized trial. Europace. 2020;22(10):1487–94. https://doi.org/10.1093/europace/euaa209.
Grosse Meininghaus D, Blembel K, Waniek C, et al. Temperature monitoring and temperature-driven irrigated radiofrequency energy titration do not prevent thermally induced esophageal lesions in pulmonary vein isolation: a randomized study controlled by esophagoscopy before and after catheter ablation. Heart Rhythm. 2021;18(6):926–34. https://doi.org/10.1016/j.hrthm.2021.02.003.
Kottkamp H, Piorkowski C, Tanner H, et al. Topographic variability of the esophageal left atrial relation influencing ablation lines in patients with atrial fibrillation. J Cardiovasc Electrophysiol. 2005;16(2):146–50. https://doi.org/10.1046/j.1540-8167.2005.40604.x.
Zhang X, Kuang X, Gao X, et al. RESCUE-AF in patients undergoing atrial fibrillation ablation: the RESCUE-AF trial. Circ Arrhythm Electrophysiol. 2019;12(5):e007044. https://doi.org/10.1161/CIRCEP.118.007044.
Aguinaga L, Palazzo A, Bravo A, et al. Esophageal deviation with vacuum suction and mechanical deflection during ablation of atrial fibrillation: first in man evaluation. J Cardiovasc Electrophysiol. 2021;32(1):67–70. https://doi.org/10.1111/jce.14801.
Leung LWM, Bajpai A, Zuberi Z, et al. Randomized comparison of oesophageal protection with a temperature control device: results of the IMPACT study. Europace. 2021;23(2):205–15. https://doi.org/10.1093/europace/euaa276.
Teres C, Soto-Iglesias D, Penela D, et al. Personalized paroxysmal atrial fibrillation ablation by tailoring ablation index to the left atrial wall thickness: the “Ablate by-LAW” single-centre study-a pilot study. Europace. 2022;24(3):390–9. https://doi.org/10.1093/europace/euab216.
Teres C, Soto-Iglesias D, Penela D, et al. Relationship between the posterior atrial wall and the esophagus: esophageal position during atrial fibrillation ablation. In Press Corrected Proof. Published online: February 13, 2022. https://doi.org/10.1016/j.hroo.2022.02.007
Falasconi G, Penela D, Soto-Iglesias D, et al. A standardized stepwise zero-fluoroscopy approach with transesophageal echocardiography guidance for atrial fibrillation ablation. J Interv Card Electrophysiol. 2021. https://doi.org/10.1007/s10840-021-01086-9.
Teres C, Soto-Iglesias D, Penela D, et al. Left atrial wall thickness of the pulmonary vein reconnection sites during atrial fibrillation redo procedures. Pacing Clin Electrophysiol. 2021;44(5):824–34. https://doi.org/10.1111/pace.14222.
Ye Y, Chen S-Q, Lu Y-F, et al. PV isolation guided by esophageal visualization with a tailored ablation strategy for the avoidance of esophageal thermal injury: a randomized trial. J Interv Card Electrophysiol an Int J Arrhythm pacing. 2020;58(2):219–27. https://doi.org/10.1007/s10840-019-00572-5.
Parikh V, Swarup V, Hantla J, et al. Feasibility, safety, and efficacy of a novel preshaped nitinol esophageal deviator to successfully deflect the esophagus and ablate left atrium without esophageal temperature rise during atrial fibrillation ablation: the DEFLECT GUT study. Heart Rhythm. 2018;15(9):1321–7. https://doi.org/10.1016/j.hrthm.2018.04.017.
Leung LWM, Akhtar Z, Sheppard MN, Louis-Auguste J, Hayat J, Gallagher MM. Preventing esophageal complications from atrial fibrillation ablation: a review. Heart Rhythm O2. 2021;2(6Part A):651–64. https://doi.org/10.1016/j.hroo.2021.09.004.
Carroll BJ, Contreras-Valdes FM, Heist EK, et al. Multi-sensor esophageal temperature probe used during radiofrequency ablation for atrial fibrillation is associated with increased intraluminal temperature detection and increased risk of esophageal injury compared to single-sensor probe. J Cardiovasc Electrophysiol. 2013;24(9):958–64. https://doi.org/10.1111/jce.12180.
Müller P, Dietrich J-W, Halbfass P, et al. Higher incidence of esophageal lesions after ablation of atrial fibrillation related to the use of esophageal temperature probes. Heart Rhythm. 2015;12(7):1464–9. https://doi.org/10.1016/j.hrthm.2015.04.005.
Sherzer AI, Feigenblum DY, Kulkarini S, et al. Continuous nonfluoroscopic localization of the esophagus during radiofrequency catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol. 2007;18(2):157–60. https://doi.org/10.1111/j.1540-8167.2006.00674.x.
Hayashi K, Okumura K, Okamatsu H, Kaneko S, Negishi K, Tsurugi T, Tanaka Y, Nakao K, Sakamoto T, Koyama J. Real-time visualization of the esophagus and left atrial posterior wall by intra-left atrial echocardiography. J Interv Card Electrophysiol. 2022;63(3):629–37. https://doi.org/10.1007/s10840-021-01093-w.
Nakatani Y, Nuñez-Garcia M, Cheniti G, et al. Preoperative personalization of atrial fibrillation ablation strategy to prevent esophageal injury: impact of changes in esophageal position. J Cardiovasc Electrophysiol. 2022;33(5):908–16. https://doi.org/10.1111/jce.15447.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The local ethics committee approved the study protocol.
Informed consent
All participants included in the study provided written informed consent.
Conflict of interest
Dr. Berruezo is stockholder of Galgo Medical. Dr. Soto-Iglesias is an employee of Biosense Webster. All remaining authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Teres, C., Soto-Iglesias, D., Penela, D. et al. Relationship between the posterior atrial wall and the esophagus: esophageal position and temperature measurement during atrial fibrillation ablation (AWESOME-AF). A randomized controlled trial. J Interv Card Electrophysiol 65, 651–661 (2022). https://doi.org/10.1007/s10840-022-01302-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-022-01302-0