Abstract
Purpose
The ideal periprocedural anticoagulation strategy for patients being treated with a novel oral anticoagulant (NOAC) during catheter ablation (CA) for atrial fibrillation (AF) is unclear. We evaluated the safety and efficacy of using a minimally interrupted NOAC strategy versus an uninterrupted NOAC or vitamin K antagonist (VKA) strategy during AF ablation.
Methods
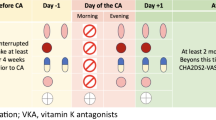
The Cochrane Library, PubMed, and EMBASE databases were searched for randomized controlled or prospective observational studies that compared a minimally interrupted NOAC strategy with an uninterrupted NOAC or VKA strategy from the time of database establishment up to December 2019. The primary endpoints were major bleeding, minor bleeding, and symptomatic thromboembolism. The secondary endpoint was silent cerebral infarction (SCI) as detected by post-ablation brain magnetic resonance imaging (MRI). A measurement of treatment effect for the endpoint was reported as pooled odds ratio (OR) with 95% confidence interval (CI).
Results
A total of 18 studies (6 randomized, 11 observational, and 1 randomized registry) with 6203 patients were included in the final analysis (47% of the patients received minimally interrupted NOAC). There was no significant difference between treatment groups regarding the risk for major bleeding (OR 1.04, 95% CI 0.69–1.57, P = 0.86, I2 = 27%). Different stratification methods did not yield significant difference regarding the risk for major bleeding. There was no difference between groups regarding the risk for minor bleeding (P = 1.00) or symptomatic thromboembolism (P = 0.26). Brain MRI results showed that both uninterrupted NOAC (OR 0.44, 95% CI 0.23–0.83, P = 0.01, I2 = 72%) and uninterrupted VKA (OR 0.48, 95% CI 0.24–0.97, P = 0.04, I2 = 36%) produced a significant reduction in the rate of SCI when compared with minimally interrupted NOAC.
Conclusions
A periprocedural anticoagulation strategy of minimally interrupted NOAC is not superior to uninterrupted NOAC or VKA when used during AF ablation. There is evidence favoring the use of uninterrupted NOAC or VKA in terms of the risk for SCI.






Similar content being viewed by others
References
Freeman JV, Wang Y, Akar J, Desai N, Krumholz H. National trends in atrial fibrillation hospitalization, readmission, and mortality for Medicare beneficiaries, 1999–2013. Circulation. 2017;135:1227–39.
Deshmukh A, Patel NJ, Pant S, Shah N, Chothani A, Mehta K, et al. In-hospital complications associated with catheter ablation of atrial fibrillation in the United States between 2000 and 2010: analysis of 93 801 procedures. Circulation. 2013;128:2104–12.
Nogami A, Harada T, Sekiguchi Y, Otani R, Yoshida Y, Yoshida K, et al. Safety and efficacy of minimally interrupted dabigatran vs uninterrupted warfarin therapy in adults undergoing atrial fibrillation catheter ablation: a randomized clinical trial. JAMA Netw Open. 2019;2:e191994.
Di Biase L, Burkhardt JD, Santangeli P, Mohanty P, Sanchez JE, Horton R, et al. Periprocedural stroke and bleeding complications in patients undergoing catheter ablation of atrial fibrillation with different anticoagulation management: results from the Role of Coumadin in Preventing Thromboembolism in Atrial Fibrillation (AF) Patients Undergoing Catheter Ablation (COMPARE) randomized trial. Circulation. 2014;129:2638–44.
Calkins H, Hindricks G, Cappato R, Kim YH, Saad EB, Aguinaga L, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Europace. 2018;20:e1–e160.
Patel PA, Zhao X, Fonarow GC, Lytle BL, Smith EE, Xian Y, et al. Novel oral anticoagulant use among patients with atrial fibrillation hospitalized with ischemic stroke or transient ischemic attack. Circ Cardiovasc Qual Outcomes. 2015;8:383–92.
Zhao Y, Lu Y, Qin Y. A meta-analysis of randomized controlled trials of uninterrupted periprocedural anticoagulation strategy in patients undergoing atrial fibrillation catheter ablation. Int J Cardiol. 2018;270:167–71.
Romero J, Cerrud-Rodriguez RC, Alviz I, Diaz JC, Rodriguez D, Arshad S, et al. Significant benefit of uninterrupted DOACs versus VKA during catheter ablation of atrial fibrillation. JACC Clin Electrophysiol. 2019;5:1396–405.
Pollack CJ. Coagulation assessment with the new generation of oral anticoagulants. Emerg Med J. 2016;33:423–30.
Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. The Cochrane Collaboration. 2011. Available from www.handbook.cochrane.org.
Egger M, Davey SG, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Reynolds MR, Allison JS, Natale A, Weisberg IL, Ellenbogen KA, Richards M, et al. A prospective randomized trial of apixaban dosing during atrial fibrillation ablation: the AEIOU trial. JACC Clin Electrophysiol. 2018;4:580–8.
Ando M, Inden Y, Yoshida Y, Sairaku A, Yanagisawa S, Suzuki H, et al. Differences in prothrombotic response between the uninterrupted and interrupted apixaban therapies in patients undergoing cryoballoon ablation for paroxysmal atrial fibrillation: a randomized controlled study. Heart Vessel. 2019;34:1533–41.
Nakamura K, Naito S, Sasaki T, Take Y, Minami K, Kitagawa Y, et al. Uninterrupted vs interrupted periprocedural direct oral anticoagulants for catheter ablation of atrial fibrillation: a prospective randomized single-centre study on post-ablation thrombo-embolic and haemorrhagic events. Europace. 2019;21:259–67.
Nagao T, Suzuki H, Matsunaga S, Nishikawa Y, Harada K, Mamiya K, et al. Impact of periprocedural anticoagulation therapy on the incidence of silent stroke after atrial fibrillation ablation in patients receiving direct oral anticoagulants: uninterrupted vs interrupted by one dose strategy. Europace. 2019;21:590–7.
Yu HT, Shim J, Park J, Kim TH, Uhm JS, Kim JY, et al. When is it appropriate to stop non-vitamin K antagonist oral anticoagulants before catheter ablation of atrial fibrillation? A multicentre prospective randomized study. Eur Heart J. 2019;40:1531–7.
Nakamura R, Okishige K, Shigeta T, Nishimura T, Kurabayashi M, Yamauchi Y, et al. Clinical comparative study regarding interrupted and uninterrupted dabigatran therapy during perioperative periods of cryoballoon ablation for paroxysmal atrial fibrillation. J Cardiol. 2019;74:150–5.
Bassiouny M, Saliba W, Rickard J, Shao M, Sey A, Diab M, et al. Use of dabigatran for periprocedural anticoagulation in patients undergoing catheter ablation for atrial fibrillation. Circ Arrhythm Electrophysiol. 2013;6:460–6.
Efremidis M, Vlachos K, Letsas KP, Giannopoulos G, Lioni L, Georgopoulos S, et al. Low dose dabigatran versus uninterrupted acenocoumarol for peri-procedural anticoagulation in atrial fibrillation catheter ablation. J Electrocardiol. 2015;48:840–4.
Kim JS, She F, Jongnarangsin K, Chugh A, Latchamsetty R, Ghanbari H, et al. Dabigatran vs warfarin for radiofrequency catheter ablation of atrial fibrillation. Heart Rhythm. 2013;10:483–9.
Lakkireddy D, Reddy YM, Di Biase L, Vanga SR, Santangeli P, Swarup V, et al. Feasibility and safety of dabigatran versus warfarin for periprocedural anticoagulation in patients undergoing radiofrequency ablation for atrial fibrillation: results from a multicenter prospective registry. J Am Coll Cardiol. 2012;59:1168–74.
Vlachos K, Efremidis M, Bazoukis G, Letsas KP, Saplaouras A, Georgopoulos S, et al. Safety and efficacy of DOACs vs acenocoumarol in patients undergoing catheter ablation of atrial fibrillation. Clin Cardiol. 2017;40:847–52.
Yoshimura A, Iriki Y, Ichiki H, Oketani N, Okui H, Maenosono R, et al. Evaluation of safety and efficacy of periprocedural use of rivaroxaban and apixaban in catheter ablation for atrial fibrillation. J Cardiol. 2017;69:228–35.
Muller P, Halbfass P, Szollosi A, Dietrich JW, Fochler F, Nentwich K, et al. Impact of periprocedural anticoagulation strategy on the incidence of new-onset silent cerebral events after radiofrequency catheter ablation of atrial fibrillation. J Interv Card Electrophysiol. 2016;46:203–11.
Ichiki H, Oketani N, Ishida S, Iriki Y, Okui H, Maenosono R, et al. The incidence of asymptomatic cerebral microthromboembolism after atrial fibrillation ablation: comparison of warfarin and dabigatran. Pacing Clin Electrophysiol. 2013;36:1328–35.
Shin DG, Kim TH, Uhm JS, Kim JY, Joung B, Lee MH, et al. Early experience of novel oral anticoagulants in catheter ablation for atrial fibrillation: efficacy and safety comparison to warfarin. Yonsei Med J. 2016;57:342–9.
Aoyama D, Miyazaki S, Hasegawa K, Kaseno K, Ishikawa E, Mukai M, et al. Feasibility of uninterrupted direct oral anticoagulants with temporary switching to dabigatran (“dabigatran bridge”) for catheter ablation of atrial fibrillation. Int Heart J. 2019;60:1315–20.
Bin AA, Kennedy KF, Gupta S, Giocondo M, Ramza B, Wimmer AP. Effect of pre-procedural interrupted apixaban on heparin anticoagulation during catheter ablation for atrial fibrillation: a prospective observational study. J Interv Card Electrophysiol. 2015;44:91–6.
Cappato R, Marchlinski FE, Hohnloser SH, Naccarelli GV, Xiang J, Wilber DJ, et al. Uninterrupted rivaroxaban vs. uninterrupted vitamin K antagonists for catheter ablation in non-valvular atrial fibrillation. Eur Heart J. 2015;36:1805–11.
Calkins H, Willems S, Gerstenfeld EP, Verma A, Schilling R, Hohnloser SH, et al. Uninterrupted dabigatran versus warfarin for ablation in atrial fibrillation. N Engl J Med. 2017;376:1627–36.
Kuwahara T, Abe M, Yamaki M, Fujieda H, Abe Y, Hashimoto K, et al. Apixaban versus warfarin for the prevention of periprocedural cerebral thromboembolism in atrial fibrillation ablation: multicenter prospective randomized study. J Cardiovasc Electrophysiol. 2016;27:549–54.
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Europace. 2016;18:1609–78.
Tripathi B, Arora S, Kumar V, Abdelrahman M, Lahewala S, Dave M, et al. Temporal trends of in-hospital complications associated with catheter ablation of atrial fibrillation in the United States: an update from Nationwide Inpatient Sample database (2011-2014). J Cardiovasc Electrophysiol. 2018;29:715–24.
Yanagisawa S, Inden Y, Fujii A, Ando M, Funabiki J, Murase Y, et al. Uninterrupted direct oral anticoagulant and warfarin administration in elderly patients undergoing catheter ablation for atrial fibrillation: a comparison with younger patients. JACC Clin Electrophysiol. 2018;4:592–600.
Kimura T, Kashimura S, Nishiyama T, Katsumata Y, Inagawa K, Ikegami Y, et al. Asymptomatic cerebral infarction during catheter ablation for atrial fibrillation: comparing uninterrupted rivaroxaban and warfarin (ASCERTAIN). JACC Clin Electrophysiol. 2018;4:1598–609.
Deneke T, Nentwich K, Krug J, Muller P, Grewe PH, Mugge A, et al. Silent cerebral events after atrial fibrillation ablation - overview and current data. J Atr Fibrillation. 2014;6:996.
Medi C, Evered L, Silbert B, Teh A, Halloran K, Morton J, et al. Subtle post-procedural cognitive dysfunction after atrial fibrillation ablation. J Am Coll Cardiol. 2013;62:531–9.
Shea S, Di Tullio M. Atrial fibrillation, silent cerebral ischemia, and cognitive function. J Am Coll Cardiol. 2013;62:1998–9.
Kirchhof P, Haeusler KG, Blank B, De Bono J, Callans D, Elvan A, et al. Apixaban in patients at risk of stroke undergoing atrial fibrillation ablation. Eur Heart J. 2018;39:2942–55.
Elgendy AY, Mahtta D, Barakat AF, Abuzaid A, Mahmoud A, Mentias A, et al. Meta-analysis of safety and efficacy of uninterrupted non-vitamin K antagonist oral anticoagulants versus vitamin K antagonists for catheter ablation of atrial fibrillation. Am J Cardiol. 2017;120:1830–6.
Wu S, Yang YM, Zhu J, Wan HB, Wang J, Zhang H, et al. Meta-analysis of efficacy and safety of new Oral anticoagulants compared with uninterrupted vitamin K antagonists in patients undergoing catheter ablation for atrial fibrillation. Am J Cardiol. 2016;117:926–34.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mao, Yj., Wang, H. & Huang, Pf. Meta-analysis of the safety and efficacy of using minimally interrupted novel oral anticoagulants in patients undergoing catheter ablation for atrial fibrillation. J Interv Card Electrophysiol 60, 407–417 (2021). https://doi.org/10.1007/s10840-020-00754-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-020-00754-6