Abstract
Research question
In women with singleton pregnancies conceived after assisted reproductive technologies, does the in vitro fertilization with oocyte donation (IVF-OD) affect the perinatal and maternal outcomes compared to autologous in vitro fertilization (IVF-AO)?
Design
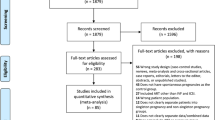
Systematic review and meta-analysis of studies comparing perinatal and maternal outcomes in singleton pregnancies resulting from IVF-OD versus IVF-AO. An electronic literature search in Pubmed, MEDLINE, and Cochrane database was performed. The main outcome measures were hypertensive disorders in pregnancy, preeclampsia, severe preeclampsia, pregnancy-induced hypertension, preterm birth, early preterm birth, low birth weight, and very low birth weight.
Results
Twenty-three studies were included. IVF-OD is associated with a higher risk of hypertensive disorders in pregnancy (OR 2.63, 2.17–3.18), preeclampsia (OR 2.64; 2.29–3.04), severe preeclampsia (OR 3.22; 2.30–4.49), pregnancy-induced hypertension (OR 2.16; 1.79–2.62), preterm birth (OR 1.57; 1.33–1.86), early preterm birth (OR 1.80; 1.51–2.15), low birth weight (OR 1.25, 1.20–1.30), very low birth weight (OR 1.37, 1.22–1.54), gestational diabetes (OR 1.27; 1.03–1.56), and cesarean section (OR 2.28; 2.14–2.42). There was no significant difference in the risk of preterm birth or low birth weight when adjusted for preeclampsia.
Conclusions
IVF-OD patients should be considered an independent risk factor for some adverse perinatal outcomes, mainly hypertensive disorders in pregnancy, preeclampsia, and severe preeclampsia. Immunological and hormonal aspects may be involved in these results, and further research focusing in the etiopathogenesis of these pathologies are needed.









Similar content being viewed by others
Change history
13 December 2019
The original article unfortunately contained a mistake. the authors have written the wrong volume/issue/pages.
References
Sauer MV. Reproduction at an advanced maternal age and maternal health. Fertil Steril. 2015;103:1136–43.
Wu Y, Chen Y, Shen M, Guo Y, Wen SW, Lanes A, et al. Adverse maternal and neonatal outcomes among singleton pregnancies in women of very advanced maternal age: a retrospective cohort study. BMC Pregnancy Childbirth. 2019;19(1):3.
Adamson GD, de Mouzon J, Chambers GM, Zegers-Hochschild F, Mansour R, Ishihara O, et al. International Committee for Monitoring Assisted Reproductive Technology: world report on assisted reproductive technology, 2011. Fertil Steril. 2018;110(6):1067–80.
De Geyter C, Calhaz-Jorge C, Kupka MS, Wyns C, Mocanu E, Motrenko T, et al. European IVF-monitoring consortium (EIM) for the European Society of Human Reproduction and Embryology (ESHRE). Hum Reprod. 2018;33(9):1586–601.
Cetinkaya MB, Siano LJ, Benadiva C, Sakkas D, Patrizio P. Reproductive outcome of women 43 years and beyond undergoing ART treatment with their own oocytes in two Connecticut university programs. J Assist Reprod Genet. 2013;30:673–8.
Busnelli A, Papaleo E, Del Prato D, et al. A retrospective evaluation of prognosis and cost-effectiveness of IVF in poor responders according to the Bologna criteria. Hum Reprod. 2015;30:315–22.
La Marca A, Grisendi V, Giulini S, et al. Live birth rates in the different combinations of the Bologna criteria poor ovarian responders: a validation study. J Assist Reprod Genet. 2015;32:931–7.
Coulam CB, Adamson SC, Annegers JF. Incidence of premature ovarian failure. Obstet Gynecol. 1986;67:604–6.
Lydic ML, Liu JH, Rebar RW, Thomas MA, Cedars MI. Success of donor oocyte in in vitro fertilization-embryo transfer in recipients with and without premature ovarian failure. Fertil Steril. 1996;65:98–102.
Ameratunga D, Weston G, Osianlis T, Catt J, Vollenhoven B. In vitro fertilisation (IVF) with donor eggs in postmenopausal women: are there differences in pregnancy outcomes in women with premature ovarian failure (POF) compared with women with physiological age-related menopause? J Assist Reprod Genet. 2009;26:511–4.
Centers for Disease Control and Prevention, American Society for Reproductive Medicine, Society for Assisted Reproductive Technology. 2012 Assisted reproductive technology fertility clinic success rates report. Atlanta (GA): US Dept of Health and Human Services; 2014.
Toner JP, Grainger DA, Frazier LM. Clinical outcomes among recipients of donated eggs: an analysis of the U.S. national experience, 1996–1998. Fertil Steril. 2002;78:1038–45.
Hudson N, Culley L, Blyth E, Norton W, Rapport F, Pacey A. Cross-border reproductive care: a review of the literature. Reprod BioMed Online. 2011;22:673–85.
Lean SC, Derricott H, Jones RL, Heazell AEP. Advanced maternal age and adverse pregnancy outcomes: a systematic review and meta-analysis. PLoS One. 2017;12(10):e0186287.
Goisis A, Remes H, Martikainen P, Klemetti R, Myrskylä M. Medically assisted reproduction and birth outcomes: a within-family analysis using Finnish population registers. Lancet. 2019
Pinborg A, Wennerholm UB, Romundstad LB, Loft A, Aittomaki K, Söderström-Anttila V, et al. Why do singletons conceived after assisted reproduction technology have adverse perinatal outcome? Systematic review and meta-analysis. Hum Reprod Update. 2013;19(2):87–104.
Roque M, Haahr T, Geber S, Esteves SC, Humaidan P. Fresh versus elective frozen embryo transfer in IVF/ICSI cycles: a systematic review and meta-analysis of reproductive outcomes. Hum Reprod Update. 2019;25(1):2–14.
Sha T, Yin X, Cheng W, Massey IY. Pregnancy-related complications and perinatal outcomes resulting from transfer of cryopreserved versus fresh embryos in vitro fertilization: a meta-analysis. Fertil Steril. 2018;109(2):330–342.e9.
Vidal M, Vellvé K, González-Comadran M, Robles A, Prat M, Torné M, et al. Perinatal outcomes in children born after fresh or frozen embryo transfer: a Catalan cohort study based on 14,262 newborns. Fertil Steril. 2017;107(4):940–7.
Soderstrom-Anttila V, Tiitinen A, Foudila T, Hovatta O. Obstetric and perinatal outcome after oocyte donation: comparison with in-vitro fertilization pregnancies. Hum Reprod. 1998;13:483–90.
Malchau SS, Loft A, Larsen EC, Aaris Henningsen AK, Rasmussen S, Andersen AN, et al. Perinatal outcomes in 375 children born after oocyte donation: a Danish national cohort study. Fertil Steril. 2013;99:1637–43.
Adams DH, Clark RA, Davies MJ, de Lacey S. A meta-analysis of neonatal health outcomes from oocyte donation. J Dev Orig Health Dis. 2015:1–16.
Storgaard M, Loft A, Bergh C, Wennerholm UB, Söderström-Anttila V, Romundstad LB, et al. Obstetric and neonatal complications in pregnancies conceived after oocyte donation: a systematic review and meta-analysis. BJOG. 2017;124(4):561–72.
Masoudian P, Nasr A, de Nanassy J, Fung-Kee-Fung K, Bainbridge SA, El Demellawy D. Oocyte donation pregnancies and the risk of preeclampsia or gestational hypertension: a systematic review and metaanalysis. Am J Obstet Gynecol. 2016;214(3):328–39.
Blázquez A, García D, Rodríguez A, Vassena R, Figueras F, Vernaeve V. Is oocyte donation a risk factor for preeclampsia? A systematic review and meta-analysis. J Assist Reprod Genet. 2016;33(7):855–63.
Corradetti A, Talebi Chahvar S, Biondini V, Giannubilo SR, Tranquilli AL. PP093 maternal and fetal outcomes in oocyte donor pregnancies. Pregnancy Hypertens. 2012;2:290–1.
Stoop D, Baumgarten M, Haentjens P, Polyzos NP, De Vos M, Verheyen G, et al. Obstetric outcome in donor oocyte pregnancies: a matched-pair analysis. Reprod Biol Endocrinol RBE. 2012;10:42.
Jeve YB, Potdar N, Opoku A, Khare M. Three-arm age-matched retrospective cohort study of obstetric outcomes of donor oocyte pregnancies. Int J Gynaecol Obstet. 2016 May;133(2):156–8.
Tarlatzi TB, Imbert R, Alvaro Mercadal B, Demeestere I, Venetis CA, Englert Y, et al. Does oocyte donation compared with autologous oocyte IVF pregnancies have a higher risk of preeclampsia? Reprod BioMed Online. 2017;34(1):11–8.
Rodriguez-Wallberg KA, Berger AS, Fagerberg A, Olofsson JI, Scherman-Pukk C, Lindqvist PG, et al. Increased incidence of obstetric and perinatal complications in pregnancies achieved using donor oocytes and single embryo transfer in young and healthy women. A prospective hospital-based matched cohort study. Gynecol Endocrinol. 2019;9:1–6.
Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA group. Preferred reporting items for systematic review and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–12.
Schünemann B, Guyatt O. GRADE Handbook. 2018.
Maheshwari A, Pandey S, Amalraj Raja E, Shetty A, Hamilton M, Bhattacharya S. Is frozen embryo transfer better for mothers and babies? Can cumulative meta-analysis provide a definitive answer? Hum Reprod Update. 2018 Jan 1;24(1):35–58.
Brown MA, Lindheimer MD, de Swiet M, Van AA, Moutquin JM. The classification and diagnosis of the hypertensive disorders of pregnancy: statement from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Hypertens Pregnancy. 2001;20:Ix–xiv.
Zegers-Hochschild F, Adamson GD, Dyer S, Racowsky C, de Mouzon J, Sokol R, et al. The International Glossary on Infertility and Fertility Care, 2017. Hum Reprod. 2017;32(9):1786–801.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5.
Wiggins DA, Main E. Outcomes of pregnancies achieved by donor egg in vitro fertilization--a comparison with standard in vitro fertilization pregnancies. Am J Obstet Gynecol. 2005;192(6):2002–6.
Krieg SA, Henne MB, Westphal LM. Obstetric outcomes in donor oocyte pregnancies compared with advanced maternal age in in vitro fertilization pregnancies. Fertil Steril. 2008;90(1):65–70.
Zegers-Hochschild F, Masoli D, Schwarze JE, Iaconelli A, Borges E, Pacheco IM. Reproductive performance in oocyte donors and their recipients: comparative analysis from implantation to birth and lactation. Fertil Steril. 2010 May 1;93(7):2210–5.
Klatsky PC, Delaney SS, Caughey AB, Tran ND, Schattman GL, Rosenwaks Z. The role of embryonic origin in preeclampsia: a comparison of autologous in vitro fertilization and ovum donor pregnancies. Obstet Gynecol. 2010;116(6):1387–92.
Gibbons WE, Cedars M, Ness RB. Society for Assisted Reproductive Technologies Writing Group. Toward understanding obstetrical outcome in advanced assisted reproduction: varying sperm, oocyte, and uterine source and diagnosis. Fertil Steril. 2011;95(5):1645–9.e1.
Cobo A, Serra V, Garrido N, Olmo I, Pellicer A, Remohí J. Obstetric and perinatal outcome of babies born from vitrified oocytes. Fertil Steril. 2014;102(4):1006–1015.e4.
Marino JL, Moore VM, Willson KJ, Rumbold A, Whitrow MJ, Giles LC, et al. Perinatal outcomes by mode of assisted conception and sub-fertility in an Australian data linkage cohort. PLoS One. 2014 Jan 8;9(1):e80398.
van Dorp W, Rietveld AM, Laven JS, van den Heuvel-Eibrink MM, Hukkelhoven CW, Schipper I. Pregnancy outcome of non-anonymous oocyte donation: a case-control study. Eur J Obstet Gynecol Reprod Biol. 2014;182:107–12.
Levron Y, Dviri M, Segol I, Yerushalmi GM, Hourvitz A, Orvieto R, et al. The ‘immunologic theory’ of preeclampsia revisited: a lesson from donor oocyte gestations. Am J Obstet Gynecol. 2014;211:383.
Baker VL, Brown MB, Luke B, Conrad KP. Association of number of retrieved oocytes with live birth rate and birth weight: an analysis of 231,815 cycles of in vitro fertilization. Fertil Steril. 2015;103(4):931–938.e2.
Letur H, Peigné M, Ohl J, Cédrin-Durnerin I, Mathieu-D'Argent E, Scheffler F, et al. Hypertensive pathologies and egg donation pregnancies: results of a large comparative cohort study. Fertil Steril. 2016;106(2):284–90.
Nejdet S, Bergh C, Källén K, Wennerholm UB, Thurin-Kjellberg A. High risks of maternal and perinatal complications in singletons born after oocyte donation. Acta Obstet Gynecol Scand. 2016;95(8):879–86.
Dude AM, Yeh JS, Muasher SJ. Donor oocytes are associated with preterm birth when compared to fresh autologous in vitro fertilization cycles in singleton pregnancies. Fertil Steril. 2016;106(3):660–5.
Kamath MS, Antonisamy B, Mascarenhas M, Sunkara SK. High-risk of preterm birth and low birth weight after oocyte donation IVF: analysis of 133,785 live births. Reprod BioMed Online. 2017;35(3):318–24.
Sites CK, Wilson D, Barsky M, Bernson D, Bernstein IM, Boulet S, et al. Embryo cryopreservation and preeclampsia risk. Fertil Steril. 2017;108(5):784–90.
Yu B, Vega M, Zaghi S, Fritz R, Jindal S, Buyuk E. Comparison of perinatal outcomes following frozen embryo transfer cycles using autologous versus donor oocytes in women 40 to 43 years old: analysis of SART CORS data. J Assist Reprod Genet. 2018;35:2025–9.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Cochrane. Review Manager. 5.3 ed. Copenhagen: The Nordic Cochrane Centre, 2014.
Jeve YB, Potdar N, Opoku A, Khare M. Donor oocyte conception and pregnancy complications: a systematic review and meta-analysis. BJOG. 2016;123(9):1471–80.
Schwarze JE, Borda P, Vásquez P, Ortega C, Villa S, Crosby JA, et al. Is the risk of preeclampsia higher in donor oocyte pregnancies? A systematic review and meta-analysis. JBRA Assist Reprod. 2018;22(1):15–9.
Keegan DA, Krey LC, Chang HC, Noyes N. Increased risk of pregnancy- induced hypertension in young recipients of donated oocytes. Fertil Steril. 2007;87:776–81.
Pecks U, Maass N, Neulen J. Oocyte donation: a risk factor for pregnancy-induced hypertension. Dtsch Arztebl Int. 2011;108:23–31.
van der Hoorn ML, Lashley EE, Bianchi DW, et al. Clinical and immunologic aspects of egg donation pregnancies: a systematic review. Hum Reprod Update. 2010;16:704–12.
Mascarenhas M, Sunkara SK, Antonisamy B, Kamath MS. Higher risk of preterm birth and low birth weight following oocyte donation: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2017;218:60–7.
Morgan TK. Role of the placenta in preterm birth: a review. Am J Perinatol. 2016;33(3):258–66.
Imudia AN, Awonuga AO, Doyle JO, Kaimal AJ, Wright DL, Toth TL, et al. Peak serum estradiol level during controlled ovarian hyperstimulation is associated with increased risk of small for gestational age and preeclampsia in singleton pregnancies after in vitro fertilization. Fertil Steril. 2012;97:1374–9.
Pereira N, Reichman DE, Goldschlag DE, Lekovich JP, Rosenwaks Z. Impact of elevated peak serum estradiol levels during controlled ovarian hyperstimulation on the birth weight of term singletons from fresh IVF-ET cycles. J Assist Reprod Genet. 2015;32(527–32):0434–1.
Farhi J, Ben Haroush A, Andrawus N, et al. High serum oestradiol concentrations in IVF cycles increase the risk of pregnancy complications related to abnormal placentation. Reprod BioMed Online. 2010;21:331e7.
Sunkara SK, La Marca A, Seed PT, Khalaf Y. Increased risk of preterm birth and low birthweight with very high number of oocytes following IVF: an analysis of 65 868 singleton live birth outcomes. Hum Reprod. 2015;30:1473–80.
Thilaganathan B. Placental syndromes: getting to the heart of the matter. Ultrasound Obstet Gynecol. 2017;49(1):7–9.
Shanis DL, Jessmon P, Sinaii N, Armant DR, Stratton P. IVF and increased risk for preeclampsia revisited: a meta-analysis. Fertil Steril. 2011;3(Suppl. 1):S181.
Savasi VM, Mandia L, Laoreti A, Ghisoni L, Duca P, Cetin I. First trimester placental markers in oocyte donation pregnancies. Placenta. 2015;36(8):921–5.
Rizzo G, Aiello E, Pietrolucci ME, Arduini D. Placental volume and uterine artery Doppler evaluation at 11 + 0 to 13 + 6 weeks’ gestation in pregnancies conceived with in-vitro fertilization: comparison between autologous and donor oocyte recipients. Ultrasound Obstet Gynecol. 2016;47(6):726–31.
Conrad KP, Baker VL. Corpus luteal contribution to maternal pregnancy physiology and outcomes in assisted reproductive technologies. Am J Phys Regul Integr Comp Phys. 2013;304:R69–72.
von Versen-Höynck F, Schaub AM, Chi YY, Chiu KH, Liu J, Lingis M, Stan Williams R, Rhoton-Vlasak A, Nichols WW, Fleischmann RR, Zhang W, Winn VD, Segal MS, Conrad KP, Baker VL. Increased preeclampsia risk and reduced aortic compliance with in vitro fertilization cycles in the absence of a corpus luteum. Hypertension. 2019.
von Versen-Höynck F, Narasimhan P, Selamet Tierney ES, Martinez N, Conrad KP, Baker VL, Winn VD. Absent or excessive corpus luteum number is associated with altered maternal vascular health in early pregnancy. Hypertension. 2019.
Shi Y, Sun Y, Hao C, Zhang H, Wei D, Zhang Y, et al. Transfer of fresh versus frozen embryos in ovulatory women. N Engl J Med. 2018;378:126–36.
Salha O, Sharma V, Dada T, Nugent D, Rutherford AJ, Tomlinson AJ, et al. The influence of donated gametes on the incidence of hypertensive disorders of pregnancy. Hum Reprod. 1999;14(9):2268–73.
Laresgoiti-Servitje E, Gomez-Lopez N, Olson DM. An immunological insight into the origins of pre-eclampsia. Hum Reprod Update. 2010;16:510–24.
van der Hoorn ML, Scherjon SA, Claas FH. Egg donation pregnancy as an immunological model for solid organ transplantation. Transpl Immunol. 2011;25:89–95 44,45.
Schonkeren D, Swings G, Roberts D, Claas F, de Heer E, Scherjon S. Pregnancy close to the edge: an immunosuppressive infiltrate in the chorionic plate of placentas from uncomplicated egg cell donation. PLoS One. 2012;7:e32347.
Gundogan F, Bianchi DW, Scherjon SA, Roberts DJ. Placental pathology in egg donor pregnancies. Fertil Steril. 2009;93:397–404.
Lashley LE, Haasnoot GW, Spruyt-Gerritse M, Claas FH. Selective advantage of HLA matching in successful uncomplicated oocyte donation pregnancies. J Reprod Immunol. 2015;112:29–33.
Moffett A, Chazara O, Colucci F, Johnson MH. Variation of maternal KIR and & fetal HLA-C genes in reproductive failure: too early for clinical intervention. Reprod BioMed Online. 2016;33:763–9.
Henderson JT, Whitlock EP, O’Conner E, Senger CA, Thompson JH, Rowland MG. Low-dose aspirin for the prevention of morbidity and mortality from preeclampsia: a systematic evidence review for the U.S. Preventive Services Task Force. Rockville: Agency for Healthcare Research and Quality (US), 2014. Report No.: 14–05207- EF-1. U.S. Preventive Services Task Force Evidence Syntheses, formerly Systematic Evidence Reviews.
Liu S, Liston RM, Joseph KS, Heaman M, Sauve R, Kramer MS, et al. Maternal mortality and severe morbidity associated with low-risk planned cesarean delivery versus planned vaginal delivery at term. CMAJ. 2007;176:455–60.
Visintin C, Mugglestone MA, Almerie MQ, Nherera LM, James D, Walkinshaw S. Management of hypertensive disorders during pregnancy: summary of NICE guidance. BMJ. 2010;341:c2207.
Braat DD, Schutte JM, Bernardus RE, Mooij TM, van Leeuwen FE. Maternal death related to IVF in the Netherlands 1984–2008. Hum Reprod (Oxford, England). 2010;25:1782–6.
Bujold E, Roberge S, Lacasse Y, Bureau M, Audibert F, Marcoux S, et al. Prevention of preeclampsia and intrauterine growth restriction with aspirin started in early pregnancy: a meta-analysis. Obstet Gynecol. 2010;116(2 Pt 1):402–14.
Bhattacharya S, Kamath MS. Reducing multiple births in assisted reproduction technology. Best Pract Res Clin Obstet Gynaecol. 2014;28:191–9 34.
Stoop D, Cobo A, Silber S. Fertility preservation for age-related fertility decline. Lancet. 2014;384:1311–9.
Glujovsky D, Riestra B, Sueldo C, Fiszbajn G, Repping S, Nodar F, et al. Vitrification versus slow freezing for women undergoing oocyte cryopreservation. Cochrane Database Syst Rev. 2014;9:CD010047.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Responsible editor: Claudio Bini
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 266 kb)
Rights and permissions
About this article
Cite this article
Moreno - Sepulveda, J., Checa, M.A. Risk of adverse perinatal outcomes after oocyte donation: a systematic review and meta-analysis. J Assist Reprod Genet 36, 2017–2037 (2019). https://doi.org/10.1007/s10815-019-01552-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-019-01552-4