Abstract
Purpose
Is there a difference in implantation and pregnancy rates between embryos transferred electively at cleavage or blastocyst stage in infertile women ≤ 38 years with at least four zygotes on day 1 post retrieval?
Methods
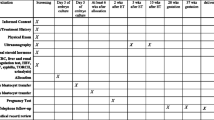
A randomized clinical trial was conducted in a single tertiary care hospital with a sample size of 194 patients in each arm for a total population of 388 women. Patients less than 39 years of age with more than three fertilized oocytes and less than four previous assisted reproductive technology (ART) attempts were inclusion criteria.
Results
The two groups were similar for age, years of infertility, indication to treatment, basal antimüllerian hormone and FSH, number of previous ART cycles, primary or secondary infertility, type of induction protocol, days of stimulation, total gonadotrophin dose, and estradiol (E2) and progesterone (P) levels at trigger. No statistically significant differences were found in terms of number of retrieved oocytes, inseminated oocytes, fertilization rate, canceled transfers (7.73% in blastocyst and 3.61% in cleavage stage group), and cycles with frozen embryos and/or oocytes. Although a higher number of fertilized oocytes were in the blastocyst stage group (6.18 ± 1.46 vs 5.89 ± 1.54, p = 0.052), a statistically greater number of embryos/randomized cycle were transferred at cleavage stage (1.93 ± 0.371) compared with the number of transferred blastocysts (1.80 ± 0.56), probably due to the number of embryos not reaching blastocyst stage (3.09%). The implantation rate (28.37 vs 25.67%), pregnancy rate per cycle (36.06 vs38.66%), transfer (39.66 vs 40.11%), spontaneous abortions (19.72% vs 12.00%), delivery rate per cycle (27.84 vs 32.99%), and transfer (30.17 vs 34.22%) were not significantly different between the blastocyst and cleavage stage groups. The twin delivery rate was higher in the blastocyst stage group, although not significant (42.59 vs 28.12%). The mean numbers of frozen blastocyst (2.30 ± 1.40 vs 2.02 ± 1.00) and frozen oocytes (7.09 ± 3.55vs 6.79 ± 3.26) were not significantly different between the two groups.
Conclusions
Fresh blastocyst-stage transfer versus cleavage-stage transfer did not show any significant difference in terms of implantation and pregnancy rate in this selected group of patients. A high twin delivery rate in both groups (35.59%) was registered, and although not significant, they were higher in the blastocyst transfer group (42.59 vs 28.12%). Our conclusion supports considering single embryo transfer (SET) policy, even in cleavage stage in patients younger than 39 years with at least four zygotes.
Trial registration
ClinicalTrials.gov registration number NCT02639000

Similar content being viewed by others
References
Human Fertilisation and Embryology Authority. Fertility treatment 2014 – Trends and figures. In. www.hfea.gov.uk. 2009–2010.
Glujovsky D, Farquhar C, Quinteiro Retamar AM, Alvarez Sedo CR, Blake D. Cleavage stage versus blastocyst stage embryo transfer in assisted reproductive technology. Cochrane Database Syst Rev 2016;(6):CD002118. https://doi.org/10.1002/14651858.CD002118.pub5.
Gosden RG. Oogenesis as a foundation for embryogenesis. Mol Cell Endocrinol. 2002;186:149–53.
Fragouli E, Alfarawati S, Spath K, Wells D. Morphological and cytogenetic assessment of cleavage and blastocyst stage embryos. Mol Hum Reprod. 2014;20:117–26.
Capalbo A, Rienzi L, Cimadomo D, Maggiulli R, Elliott T, Wright G, et al. Correlation between standard blastocyst morphology, euploidy and implantation: an observational study in two centers involving 956 screened blastocysts. Hum Reprod. 2014;
Gleicher N, Orvieto R. Is the hypothesis of preimplantation genetic screening (PGS) still supportable? A review J Ovarian Res. 2017;10:21.
Orvieto R. Re-analysis of aneuploidy blastocysts with an inner cell mass and different regional trophectoderm cells. J Assist Reprod Genet. 2017;34:827.
Glujovsky D, Farquhar C. Cleavage-stage or blastocyst transfer: what are the benefits and harms? Fertil Steril. 2016;106:244–50.
Harton GL, Munné S, Surrey M, Grifo J, Kaplan B, McCulloh DH, et al. Diminished effect of maternal age on implantation after preimplantation genetic diagnosis with array comparative genomic hybridization. Fertil Steril. 2013;100:1695–703.
Glujovsky D, Blake D, Farquhar C, Bardach A. Cleavage stage versus blastocyst stage embryo transfer in assisted reproductive technology. Cochrane Database Syst Rev 2012;(7):CD002118. https://doi.org/10.1002/14651858.CD002118.pub4.
Dar S, Lazer T, Shah PS, Librach CL. Neonatal outcomes among singleton births after blastocyst versus cleavage stage embryo transfer: a systematic review and meta-analysis. Hum Reprod Update. 2014;20:439–48.
Maheshwari A, Kalampokas T, Davidson J, Bhattacharya S. Obstetric and perinatal outcomes in singleton pregnancies resulting from the transfer of blastocyst-stage versus cleavage-stage embryos generated through in vitro fertilization treatment: a systematic review and meta-analysis. Fertil Steril. 2013;100:1615–21.e1-10.
Martins WP, Nastri CO, Rienzi L, van der Poel SZ, Gracia CR, Racowsky C. Obstetrical and perinatal outcomes following blastocyst transfer compared to cleavage transfer: a systematic review and meta-analysis. Hum Reprod. 2016;31:2561–9.
Wang X, Du M, Guan Y, Wang B, Zhang J, Liu Z. Comparative neonatal outcomes in singleton births from blastocyst transfers or cleavage-stage embryo transfers: a systematic review and meta-analysis. Reprod Biol Endocrinol. 2017;15:36.
Maheshwari A, Hamilton M, Bhattacharya S. Should we be promoting embryo transfer at blastocyst stage? Reprod BioMed Online. 2016;32:142–6.
Levi Setti PE, Albani E, Matteo M, Morenghi E, Zannoni E, Baggiani AM, et al. Five years (2004-2009) of a restrictive law-regulating ART in Italy significantly reduced delivery rate: analysis of 10,706 cycles. Hum Reprod. 2013;28:343–9.
Levi Setti PE, Morenghi E, Sonia C, Galliera S, Arfuso V, Menduni F. Restrictive law regulating art in Italy significantly reduced delivery rate in infertile patients art cycles. Fertil Steril. 2010;94:S265–S6.
Levi Setti PE, Albani E, Cesana A, Novara PV, Zannoni E, Baggiani AM, et al. Italian Constitutional Court modifications of a restrictive assisted reproduction technology law significantly improve pregnancy rate. Hum Reprod. 2011;26:376–81.
Levi-Setti PE, Borini A, Patrizio P, Bolli S, Vigiliano V, De Luca R, et al. ART results with frozen oocytes: data from the Italian ART registry (2005-2013). J Assist Reprod Genet. 2016;33:123–8.
Levi-Setti PE, Patrizio P, Scaravelli G. Evolution of human oocyte cryopreservation: slow freezing versus vitrification. Curr Opin Endocrinol Diabetes Obes. 2016;23:445–50.
Practice Committee of the American Society for Reproductive Medicine, and the Practice Committee of the Society for Assisted Reproductive Technology. Blastocyst culture and transfer in clinical-assisted reproduction. Fertil Steril. 2008;90:S174–7.
Practice Committee of the American Society for Reproductive Medicine, and the Practice Committee of the Society for Assisted Reproductive. Blastocyst culture and transfer in clinical-assisted reproduction. Fertil Steril. 2006;86:S89–92.
The Istambul Consensus workshop on embryo assessment:proceeding of an expert meeting. In. Vol. 26(6). Human Reprod, 2011;1270–83.
Practice Committee of the American Society for Reproductive Medicine, and the Practice Committee of the Society for Assisted Reproductive Technology. Guidance on the limits to the number of embryos to transfer: a committee opinion. Fertil Steril. 2017;107:901–3.
Neilson JP, Danskin F, Hastie SJ. Monozygotic twin pregnancy: diagnostic and Doppler ultrasound studies. Br J Obstet Gynaecol. 1989;96:1413–8.
Kissin DM, Kulkarni AD, Mneimneh A, Warner L, Boulet SL, Crawford S, et al. Embryo transfer practices and multiple births resulting from assisted reproductive technology: an opportunity for prevention. Fertil Steril. 2015;103:954–61.
Practice Committee of the American Society for Reproductive Medicine, and the Practice Committee of the Society for Assisted Reproductive Technology. Criteria for number of embryos to transfer: a committee opinion. Fertil Steril. 2013;99:44–6.
Practice Committee of the American Society for Reproductive Medicine, and the Practice Committee of the Society for Assisted Reproductive Technology. Guidelines on number of embryos transferred. Fertil Steril. 2009;92:1518–9.
Begley CG, Ellis LM. Drug development: raise standards for preclinical cancer research. Nature. 2012;483:531–3.
Meldrum DR, Su HI. There’s no difference-are you sure? Fertil Steril. 2017;108(2):231–32.
De Vos A, Van Landuyt L, Santos-Ribeiro S, Camus M, Van de Velde H, Tournaye H, et al. Cumulative live birth rates after fresh and vitrified cleavage-stage versus blastocyst-stage embryo transfer in the first treatment cycle. Hum Reprod. 2016;31:2442–9.
Acknowledgements
The authors wish to acknowledge and sincerely thank all the Humanitas Fertility Center staff for their unique support in conducting this study. We thank Pasquale Patrizio, Yale Fertility Center, for his support in revising the manuscript.
Author information
Authors and Affiliations
Contributions
PELS, EA, and EM were involved in the study concept and design. FC, EA, and AS contributed to the acquisition of data. EM analyzed data. PELS, FC, and GEGM wrote the manuscript and had a primary responsibility for the final content. PELS supervised the analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
The study protocol and specific consent form have been approved by our Ethical Committee on June 24, 2010.
ᅟ
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Levi-Setti, P.E., Cirillo, F., Smeraldi, A. et al. No advantage of fresh blastocyst versus cleavage stage embryo transfer in women under the age of 39: a randomized controlled study. J Assist Reprod Genet 35, 457–465 (2018). https://doi.org/10.1007/s10815-017-1092-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-017-1092-2