Abstract
Introduction
In thyroid eye disease (TED), all ocular components and adnexa such as extraocular muscles, orbital adipose tissues, eyelids, and tear glands could be affected. This study aimed to study the orbital biomechanical parameters in patients with TED, in terms of differences with healthy individuals and correlation with clinical findings, using Corvis ST (CST, Oculus Wetzlar).
Materials and methods
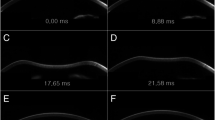
In this study, 26 consecutive patients with TED were recruited. Demographic data were collected, and patients with TED were assessed for exophthalmos, intraocular pressure, and clinical activity score. Biomechanical response parameters of one randomly-chosen eye of each patient, including whole eye movement length (WEMl) and time (WEMt), were evaluated by the CST, and data were compared between patients and age- and gender-matched healthy controls.
Results
The mean age was 39.88 ± 11.61 years old for patients with TED and 34.38 ± 8.57 years old for the healthy subjects. Nine out of 26 patients with TED and nine of 26 healthy individuals were male. The median duration of thyroid disease was 36 (IQR 54) months and the median duration of thyroid ophthalmopathy was 27 (IQR 27) months. Four out of 26 patients (7.7%) had active disease. The mean WEMl was 206.15 ± 61.58 µm in the TED group and 254.23 ± 64.01 μm in the healthy group, the difference of which was statistically significant (p = 0.008). The median of WEMt was 20.90 (1.15) msec in the TED group and 21.45 (0.93) msec in the healthy group (p < 0.001). Also, the mean of WEMl and WEMt were lower in patients with active disease compared to patients with quiescent disease.
Conclusion
The CST-derived WEMl was significantly smaller in patients with thyroid eye disease compared to normal subjects. The WEMl and WEMt were relatively shorter in the patients with active TED compared to the patients with quiescent TED, although small numbers of patients with active TED limits took a statistically significant conclusion. WEMl and WEMt might be useful in evaluating the compliance of the orbit in patients with TED.

Similar content being viewed by others
References
Chin YH, Ng CH, Lee MH, Koh JWH, Kiew J, Yang SP et al (2020) Prevalence of thyroid eye disease in Graves’ disease: a meta-analysis and systematic review. Clin Endocrinol 93:363–374
Bartalena L, Tanda ML (2009) Graves’ ophthalmopathy. N Engl J Med 360:994–1001
Forbes GGC, Brennan MD, Gehring DG, Ilstrup DM, Earnest F (1986) Ophthalmopathy of Graves’ disease: computerized volume measurements of the orbital fat and muscle. Am J Neuroradiol 7:651–656
Smith TJ, Laszlo H (2016) Graves’ disease. N Engl J Med 375:1552–1565
Frueh BR (1984) Graves’ eye disease: orbital compliance and other physical measurements. Trans Am Ophthalmol Soc 82:492
McAlinden C (2014) An overview of thyroid eye disease. Eye Vis 1:1–4
Enzmann D, Marshall WH Jr, Rosenthal AR, Kriss JP (1976) Computed tomography in Graves’ ophthalmopathy. Radiology 118:615–620
Hwang HS, Kim EC, Kim MS, Yang SW (2019) A novel method for quantifying the biomechanical parameters of orbital soft tissue using a corneal dynamic scheimpflug analyser: a retrospective study. BMC ophthalmol 19:53
Vellara HR, Ali NQ, Gokul A, Turuwhenua J, Patel DV, McGhee CNJ (2015) Quantitative analysis of corneal energy dissipation and corneal and orbital deformation in response to an air-pulse in healthy eyes. Invest Ophthalmol Vis Sci 56:6941–6947
Vellara HR, Hart R, Gokul A, McGhee CN, Patel DV (2017) In vivo ocular biomechanical compliance in thyroid eye disease. Br J Ophthalmol 101:1076–1079
Vinciguerra R, Ambrósio R Jr, Elsheikh A, Roberts CJ, Lopes B, Morenghi E et al (2016) Detection of keratoconus with a new biomechanical index. J Refract Surg 32:803–810
Leszczynska A, Moehler K, Spoerl E, Ramm L, Herber R, Pillunat LE et al (2018) Measurement of orbital biomechanical properties in patients with thyroid orbitopathy using the dynamic scheimpflug analyzer (Corvis ST). Curr Eye Res 43:289–292
Li HX, Zhao XH, Song Y, Mu BK, Pan Y, Zhao H et al (2021) Changes in ocular biomechanics after treatment for active Graves’ orbitopathy. J Endocrinol Invest 44:453–458
Mourits MP, Prummel MF, Wiersinga WM, Koornneef L (1997) Clinical Activity score as a guide in the management of patients with Graves’ ophthalmopathy. Clin Endocrinol 47:9–14
Clarke L, Perros P (2014) Medical management of mild and moderate to severe thyroid eye disease. In: Douglas RS, McCoy AN, Gupta S (eds) Thyroid eye disease. Springer, New York, pp 83–87
Pandey N, Kaur Chhabra A (2021) Evaluation of corneal biomechanical properties on ocular response analyzer and their correlation with the clinical profile of the patients with thyroid-associated ophthalmopathy. Orbit 40:193–198
Roos JC, Murthy R (2019) Update on the clinical assessment and management of thyroid eye disease. Curr Opin Ophthalmol 30:401–406
Han SB, Liu Y-C, Mohamed-Noriega K, Mehta JS (2021) Advances in imaging technology of anterior segment of the eye. J Ophthalmol 23(2021):9539765
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Study conception and design was done by [SZ-G, MYK, SHGS]. Material preparation, data collection and analysis were performed by [MYK, AMR], and [ ASM]. The first draft of the manuscript was written by [EB] and all authors commented on the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. The study protocol was approved by the Ethics Committee of Mashhad University of Medical Sciences.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Moeen Rad, A., Zarei-Ghanavati, S., Sabermoghaddam, A. et al. Evaluation of orbital soft tissue biomechanical parameters in patients with thyroid eye disease using the non-contact Corvis ST. Int Ophthalmol 43, 3615–3621 (2023). https://doi.org/10.1007/s10792-023-02770-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-023-02770-7