Abstract
Purpose
To assess and compare the efficiency of quick response (QR) code versus telephone contact for post-discharge follow-up in patients receiving low-risk ophthalmic day surgery.
Methods
One hundred and sixty patients undergoing strabismus day-care surgery with general anesthesia were randomly allocated to either the intervention group using QR code (QR group) or the control group receiving telephone call (TEL group) for post-discharge follow-up. The primary outcome was the follow-up overall attendance rate on the second postoperative day. Secondary outcomes included attendance rate at the first scheduled follow-up, number of text message reminders, elapsed time and estimated cost for follow-up, omission rate of follow-up responses, and patient satisfaction.
Results
The overall attendance rate of follow-up was significantly higher in the QR group than that in the TEL group (97.5% vs. 87.5%, p = 0.016). As compared with the TEL group, the QR group significantly reduced the number of text message reminders with higher attendances at the first scheduled follow-up (p < 0.001, p = 0.001). Besides, the TEL group cost a median time of 258 s and a median cost of RMB 5.8 yuan to complete a follow-up consultant, but was associated with a significantly high omission rate of follow-up responses comparing to the QR group (p = 0.002). Patient satisfaction was comparable between two groups.
Conclusion
QR code follow-up can be more efficient than traditional telephone contact in assessing the post-discharge recovery after strabismus day surgery, which provides a safe and intuitively alternative follow-up pathway for identifying issues that may necessitate further clinical care for more low-risk ophthalmic day surgeries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ophthalmic surgeries are primarily performed as day-care procedures, in which patients are admitted and discharged on the same day [1, 2]. Shortened hospital stays and progressively earlier discharge for day-care patients have moved the focus of care from hospital to home. After discharge, patients are expected to manage their recovery. These practices leave patients feeling insecure and worried due to a lack of feedback regarding normality and relevant expectations during recovery. Thus, day surgery generally involves a follow-up review on the first or second postoperative day (POD) and is seen as extending nursing care to monitor and guide rehabilitation after discharge, and additionally, to ensure a safe transition from hospital to home [2].
Routines for follow-up after day surgery vary, and with nearly ubiquitous access to mobile phones, telephone consultation becomes a common choice for outpatient care [3]. Although telephone follow-up has demonstrated high patient satisfaction, the time consuming in telephone consultation places an unexpected workload on nursing care. While one consultation takes 10 min, nurses may spend approximately 16 h for 100 patients, which is equal to two nursing shifts [4]. Since the outbreak of the COVID-19 pandemic, the quick response (QR) code has been extensively applied in the field of medical service [5]. QR code is a two-dimensional barcode, which can be scanned by a smartphone application (for example, WeChat) to directly open a web page, link to a video, or display a text [6]. The extensive global use of smartphone promises to enhance the feasibility of utilizing QR codes, and this is especially the case in China.
In this study, we utilized a pre-generated QR code, linking to a single-page website displaying a standard follow-up questionnaire for patients receiving strabismus day surgery. The purpose of the study is to compare the efficiency of providing follow-up via QR code with those using telephone.
Methods
Study design and ethics
This prospective, randomized, controlled study was performed at a tertiary academic eye institution in China, from March to September 2020. Study approval was obtained from the Institutional Review Board of Zhongshan Ophthalmic Center, Sun Yat-sen University (No. 2019KYPJ126). This study was preregistered at the Chinese Clinical Trial Registry (identifier No. ChiCTR1900026591). The study adheres to the Consolidated Standards of Reporting Trials (CONSORT) statement. Written informed consent was obtained from all participants.
Study population and randomization
Adult (aged 18–60 years), Chinese-speaking patients scheduled for monocular strabismus day surgery (< 24 h inpatient stay) under general anesthesia were assessed for eligibility. Exclusion criteria were as follows: no access to a smartphone or not having an available internet connection, visual or hearing impairment, cognitive disorders, and change to in-hospital observation overnight after surgery.
Enrolled patients were randomly and equally assigned to two study groups via a random number sequence generated by the SAS® software (SAS Institute, Cary, NC, USA). The QR group received a QR code for post-discharge follow-up, while the TEL group received telephone contact for follow-up after discharge home. Group allocations were concealed using sequentially numbered sealed envelopes. On the day of surgery, before patients were ready to discharge from the post-anesthesia care unit (PACU), a research assistant uninvolved in the process of follow-ups opened the envelope to reveal the group assignment. Due to the nature of the intervention, neither the participants nor the research nurse who was responsible for performing follow-ups could be blinded to randomization.
Postoperative care
After surgery, subjects were transferred to PACU Phase I recovery room where standard monitoring was applied, and vital signs were checked every 10 min [7]. When patients achieved a modified Aldrete’s score of 9 or 10, they would be transferred to PACU Phase II recovery room [8]. Finally, patients were considered safe to discharge once their Chung’s Post-Anesthetic Discharge Scoring System (PADSS) scores achieved at 9 or 10 [9]. A trained and registered nurse in the PACU evaluated all the physiological systems.
In Phase II recovery room, patients and their caregivers were educated on important signs and symptoms necessitating urgent access to care. Verbal instructions and cautions of nursing care were reinforced with a 2 min video review before discharge, and a take-home discharge brochure for common complication management was delivered to the patients at discharge. Both groups of patients were offered a 24-h telephone helpline to the physician on call if they had additional clinical questions or concerns, and they were advised to contact the local hospital emergency department if needing emergency care.
Post-discharge follow-up
Before hospital discharge, both groups were booked for follow-up on POD 2 and were notified of their appointment by a phone message at discharge.
Participants in the TEL group received follow-up by telephone consultation. The calls were placed during the daytime on POD 2. Telephone consultations were entirely made in Chinese by a trained certified research nurse, using a standard questionnaire to ensure consistency. The questionnaire was created based on the most frequent postoperative complications after ophthalmic surgeries following general anesthesia [7]. If patients had additional clinical concerns, they were provided with appropriate contact information. The satisfaction level for the follow-up method was also assessed. These variables were documented as ‘yes’ or ‘no’ in the electronic medical record, and any additional patient concerns were noted as described in detail. In the QR group, patients received follow-up using QR code. A specific QR code was pre-generated to link the web version of the follow-up questionnaire (Fig. 1), which contained questions the same as those in the group TEL. Before patient discharge, a QR code scan application (WeChat) was installed on their smartphones, and they were trained in application use, including how to move from question to question, how to input a response, and how to submit, by the nurses in the PACU. A research nurse would extract and check the responses through the computer client on the follow-up day. Based on patient responses, if the assessment demonstrated an abnormal recovery, defined as worsening pain despite the use of analgesics, signs or symptoms of uncontrolled complications (i.e., high fever, severe vomiting, etc.), or persistent bleeding at the incision site, a nurse-initiated telephone call was made to the patient with treatment advice.
For those who were incomplete follow-up at their appointment time, they were given a reminder by phone message once again. Lost to follow-up was defined as unable to complete follow-up via QR code or be contacted via telephone after 3 times of additional message reminders.
Study outcomes
The primary outcome was the overall attendance rate for post-discharge follow-up on POD 2. Secondary outcomes included attendance rate at the first scheduled follow-up, number of text message reminders, elapsed time and estimated cost for follow-up, omission rate of follow-up responses, and patient satisfaction.
Attendance rate of follow-up was defined as success to contact patients in the TEL group or initiative to complete the web-based follow-up via QR code in the QR group during the allocated period. Satisfaction level was measured on a three-point scale from 1 to 3 (1: completely unsatisfied, 2: neutral, 3: completely satisfied).
Statistical analysis
Based on our preliminary study, the overall attendance rate of post-discharge follow-up was approximately 81% for ophthalmic day-care patients. We expected a 15% increment by using a QR code for follow-up (90%), allowing a 10% drop-out. Assuming a type I error of 0.05 and a power of 0.8, a sample size of 160 was calculated with 80 allocated to each arm.
Data were analyzed using the intention to treat principle. The analysis was performed using SPSS 23.0 (SPSS Inc, Chicago, IL). Data were inspected and assessed for distribution according to the Kolmogorov–Smirnov test. Normally distributed data were expressed as mean ± SD and analyzed with Student’s t test, non-parametric data were expressed as median (IQR) and compared using Mann–Whitney U test. Categorical data were expressed as frequencies with percentages and analyzed using the chi-squared test or Fisher exact test as appropriate. Logistic regression was used to identify the potential influence factors of overall attendance rate of post-discharge follow-up. A two-tailed P value < 0.05 was considered statistically significant.
Results
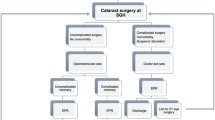
A total of 180 patients were screened for eligibility from March to September 2020, and 160 met the inclusion criteria and were randomized into two groups. Figure 2 details the flow schema of all study patients. Baseline demographics were comparable between the two groups (Table 1).
As shown in Table 2, the primary outcome, which was the overall attendance rate of follow-up, was significantly increased in the QR group than that in the TEL group (97.5% vs. 87.5%, p = 0.016). The attendance rate at the first scheduled follow-up was 91.3% for the QR group, whereas 71.3% for the TEL group (p = 0.001). The number of additional message reminders dramatically reduced in group QR than that in group TEL [0 (0–0) vs. 1 (1–2), p = 0.002]. In group TEL, a median time of 258 (217–319) s was cost on the telephone call to contact (approximately 5 min), which was equivalent to cost RMB 5.8 (4.8–7.1) yuan for each patient to complete a telephone follow-up. Meanwhile, the omission rate of follow-up responses in group QR greatly reduced to 2.5% from 18.8% in group TEL (p = 0.002). Among the reasons, 2 (2.5%) and 10 (12.5%) of patients lost to follow-up in the QR and TEL groups, respectively, and 5 (6.3%) in the TEL group were omitted during data processing. Satisfaction was relatively high with both follow-up methods (91% vs. 91.4% for satisfied, 9.0% vs. 8.6% for neutral in the QR and TEL group, respectively; p = 0.931), and none of the patients complained of dissatisfaction.
Apart from the grouping (OR = 5.571, p = 0.030), no further correlation was found between the primary outcome and other essential characteristics of the two groups (Table 3).
Discussion
This study demonstrates that, in comparison with follow-up telephone contacts, introducing QR code for routine follow-up after strabismus day surgery was found to be efficacious with better attendance and less data omission, potentially giving a reduction in the workload of nursing care as well as the medical cost.
Owing to factors such as improvements in anesthetics and advances in surgical techniques, day surgery has become common, especially for ophthalmology [10]. Yet a patient admitted for ophthalmic day surgery is postoperatively monitored for only a few hours before being discharged, at which point the patient must assume primary responsibility for monitoring his or her own recovery. Therein, day-surgery units employ a wide variety of practices for routine follow-up assessments of adults who have undergone surgery to ask about their recovery and complications. As a general approach, telephone follow-up has proved to be highly satisfactory and easy to implement after day surgery to reassure patients and manage potential early complications in the first two days [11]. However, our findings demonstrated that 12.5% of patients were lost to follow-up after hospital discharge due to difficulty contacting by telephone, which is comparable with the existing literature establishing a non-attendance rate of 14.6% at postoperative telephone review in a general surgical outpatient cohort [12]. Attendance rate is important in evaluating the effectiveness of follow-up consultation, and poor patient attendance to scheduled follow-up is associated with a high risk of missing complications. Instead of telephone follow-up, QR code-based follow-up is more effectively with lower rate of loss to follow-up for remote symptom monitoring during postoperative recovery, which will be useful in helping to guide improvements in the areas of anesthesia and postoperative care of patients who currently receive low-risk ophthalmic day surgery.
In our results, follow-up using a QR code linked to better attendance rate when comparing to those using telephone. With increased dependence on smart devices at present, mobile health has become an integral part of medical service and shapes the way patients interact with healthcare providers [13]. As COVID-19 is rapidly spreading around the world, China’s government has implemented a health QR code in normalized health surveillance to identify people potentially exposed to COVID-19. Impressively, the health QR code has been applied in more than 300 Chinese cities and covers at least 900 million users, thus raising the feasibility of applying the QR code for postoperative follow-up [14]. Moreover, using QR code follow-up gives patients the choice to complete the follow-up questionnaire at any time on the appointment day, which is flexible and avoidance of missing calls.
Other advantages of QR code follow-up comprise the omission of elapsed time for patient consultations and the elimination of the fees associated with telephone calls. As we estimated, a 5-min self-reporting questionnaire on mobile compared with a 5- to 10-min nurse-led follow-up call would most likely show savings in charges of calls and salary costs of the calling nurses. Moreover, all data of QR code follow-up could be extracted with one click on computer, which just cost a few minutes. Instead, responses of telephone follow-up needed to be manually entered into the database one by one, which approximately took one minute to entry one questionnaire. It is obviously that QR code follow-up could effectively reduce the nursing workload by consuming less time in data extraction, thus freeing up resources for more appropriate usage.
Our study included yes/no questions regarding post-discharge healthcare consultants. In the returned questionnaires, missing answers were more frequent in telephone follow-ups (18.8% vs. 2.5%). These results show that QR code follow-up is more likely to improve the quality of data, seen as a decrease in the omission of follow-up information. Previous work has shown the importance of patient education and medication reconciliation before discharge in reducing postoperative pain and disability after day surgery, therein preventing problems from occurring or worsening and reducing readmissions [15, 16]. Therefore, in our protocol, patients should receive adequate education before discharge, with those early common complications managed in the usual manner, and be given a 24-h phone number to contact if any concerns arose.
Our high patient satisfaction with post-discharge follow-up demonstrates that patients do expect follow-up in some forms, which can adequately provide reassurance. However, we noted some limitations to our study. First, it may be inconvenient for patients to use the smartphone after ophthalmic surgeries, but we educated both the patients and their caregivers before the surgery to overcome the problems. Second, the study population was relatively younger with a median age of 25.5 years because of the epidemiological characteristics of strabismus. These results may not apply to the elderly, who may prefer to be followed up with traditional ways, for example, clinic review or telephone consultation. Further study should be conducted to include a broad range of patients regarding age and different types of ophthalmic surgeries. Our future study with a larger sample size will further investigate an upgrade to the QR code application, for example, to upload pictures to the system or to add spaces for general comments, so that we can better understand the patient recovery.
In conclusion, our results show that post-discharge QR code follow-up is associated with a higher attendance rate, better quality of data, cost and nursing savings. Its success in the setting of strabismus surgery also forms a strong basis to extend its utility in other types of uncomplicated ophthalmic day surgery.
References
Steiner CA, Karaca Z, Moore BJ, Imshaug MC, Pickens G (2017) Surgeries in hospital-based ambulatory surgery and hospital inpatient settings, 2014: Statistical Brief #223. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): Agency for Healthcare Research and Quality (US)
Bailey CR, Ahuja M, Bartholomew K et al (2019) Guidelines for day-case surgery 2019: guidelines from the association of anaesthetists and the British association of day surgery. Anesthesia 74(6):778–792. https://doi.org/10.1111/anae.14639
Kimman ML, Bloebaum MM, Dirksen CD, Houben RM, Lambin P, Boersma LJ (2010) Patient satisfaction with nurse-led telephone follow-up after curative treatment for breast cancer. BMC Cancer 10:174. https://doi.org/10.1186/1471-2407-10-174
Ma Y, Jones G, Tay YK et al (2018) Post-operative telephone review is safe and effective: a prospective study—Monash outpatient review by phone trial. ANZ J Surg 88(5):434–439. https://doi.org/10.1111/ans.14280
Perez-Alba E, Nuzzolo-Shihadeh L, Espinosa-Mora JE, Camacho-Ortiz A (2020) Use of self-administered surveys through QR code and same center telemedicine in a walk-in clinic in the era of COVID-19. J Am Med Inform Assoc 27(6):985–986. https://doi.org/10.1093/jamia/ocaa054
Yuan T, Wang Y, Xu K, Martin RR, Hu SM (2019) Two-layer QR codes. IEEE Trans Image Process 28(9):4413–4428. https://doi.org/10.1109/TIP.2019.2908490
Zhu Y, Yang S, Zhang R et al (2020) Using clinical-based discharge criteria to discharge patients after ophthalmic ambulatory surgery under general anesthesia: an observational study. J Perianesth Nurs 35(6):586-591.e1. https://doi.org/10.1016/j.jopan.2020.04.012
Aldrete JA (1995) The post-anesthesia recovery score revisited. J Clin Anesth 7(1):89–91. https://doi.org/10.1016/0952-8180(94)00001-k
Chung F, Chan VW, Ong D (1995) A post-anesthetic discharge scoring system for home readiness after ambulatory surgery. J Clin Anesth 7(6):500–506. https://doi.org/10.1016/0952-8180(95)00130-a
Weingessel B, Wahl M, Vécsei-Marlovits PV (2017) More frequent requests for day-case cataract surgery : an impressive mind switch in the Austrian population within 7 years. deutlich gesteigerter Wunsch nach tagesklinischer Kataraktversorgung : ein eindrucksvoller Umdenkprozess in der österreichischen Bevölkerung innerhalb von 7 Jahren. Wien Med Wochenschr 167(13):314–319. https://doi.org/10.1007/s10354-017-0554-6
Fallis WM, Scurrah D (2001) Outpatient laparoscopic cholecystectomy: home visit versus telephone follow-up. Can J Surg 44(1):39–44
Gray RT, Sut MK, Badger SA, Harvey CF (2010) Post-operative telephone review is cost-effective and acceptable to patients. Ulster Med J 79(2):76–79
Liu T, Xie S, Wang Y et al (2021) Effects of app-based transitional care on the self-efficacy and quality of life of patients with spinal cord injury in China: randomized controlled trial. JMIR Mhealth Uhealth 9(4):22960. https://doi.org/10.2196/22960
Liang F (2021) COVID-19 and health code: how digital platforms tackle the pandemic in China. Soc Media Soc 6(3):2056305120947657. https://doi.org/10.1177/2056305120947657
Pugh J, Penney LS, Noël PH et al (2021) Evidence-based processes to prevent readmissions: more is better, a ten-site observational study. BMC Health Serv Res 21(1):189. https://doi.org/10.1186/s12913-021-06193-x
Daniels SA, Kelly A, Bachand D et al (2016) Call to care: the impact of 24-hour postdischarge telephone follow-up in the treatment of surgical day care patients. Am J Surg 211(5):963–967. https://doi.org/10.1016/j.amjsurg.2016.01.015
Acknowledgements
This study was supported by the Clinical Research Project of Zhongshan Ophthalmic Center of Sun Yat-sen University, China (3030901010073), and the National Natural Science Foundation of China (81901995 and 81571884).
Funding
This research did not receive any specific grant from the public, commercial, or not-for-profit funding agencies.
Author information
Authors and Affiliations
Contributions
PF was involved in conception and design of the study; LX contributed to data collection; ML, YL were involved in data analysis; PF, GY contributed to interpretation of results and manuscript preparation; XG, ZX critically revised the manuscript drafts; YZ read and approved the final version of this manuscript. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest related to this study.
Ethical approval
Ethics approval for the study was obtained from the Institutional Review Board of Zhongshan Ophthalmic Center, Sun Yat-sen University.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Peiting Fan and Minyan Liao are co-first authors.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fan, P., Liao, M., Xiao, L. et al. The efficiency of quick response code versus telephone contact for post-discharge follow-up after ophthalmic day surgery: a randomized controlled trial. Int Ophthalmol 43, 2669–2677 (2023). https://doi.org/10.1007/s10792-023-02666-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-023-02666-6